Abstract
Alum adjuvants have been in continuous clinical use for more than 80 yr. While the prevailing theory has been that depot formation and the associated slow release of antigen and/or inflammation are responsible for alum enhancement of antigen presentation and subsequent T- and B-cell responses, this has never been formally proven. To examine antigen persistence, we used the chimeric fluorescent protein EαGFP, which allows assessment of antigen presentation in situ, using the Y-Ae antibody. We demonstrate that alum and/or CpG adjuvants induced similar uptake of antigen, and in all cases, GFP signal did not persist beyond 24 h in draining lymph node antigen-presenting cells. Antigen presentation was first detectable on B cells within 6–12 h of antigen administration, followed by conventional dendritic cells (DCs) at 12–24 h, then finally plasmacytoid DCs at 48 h or later. Again, alum and/or CpG adjuvants did not have an effect on the magnitude or sequence of this response; furthermore, they induced similar antigen-specific T-cell activation in vivo. Notably, removal of the injection site and associated alum depot, as early as 2 h after administration, had no appreciable effect on antigen-specific T- and B-cell responses. This study clearly rules out a role for depot formation in alum adjuvant activity.—Hutchison, S., Benson, R. A., Gibson, V. B., Pollock, A. H., Garside, P., Brewer, J. M. Antigen depot is not required for alum adjuvanticity.
Keywords: vaccine, in vivo
Antigen depot is frequently cited as the principal mechanism of action of vaccine adjuvants, in particular clinically applicable adjuvants, such as alum. That depot formation is important for alum adjuvant activity was first proposed by Glenny et al. (1, 2) in 1925. Since then, our understanding of microbial adjuvant activity has progressed greatly, particularly in the past 15 yr, with the description of Toll-like receptor (TLR) recognition of microbial patterns, directly activating dendritic cell (DC) antigen presentation and T-cell activation (3). More recently, the induction of inflammation by sensors of endogenous danger signals has been proposed as a mechanism where nonmicrobial adjuvants may have similar effects on DCs to enhance subsequent T-cell responses (4). However, the role of these mechanisms in alum adjuvant activity has remained controversial (5, 6). In the absence of a definitive mechanism of action, alum has remained in constant clinical use for the past 80 yr, and throughout this period, the depot theory of alum adjuvant activity has persisted. However, no evidence exists in the literature to demonstrate the importance, or otherwise, of the antigen depot in the enhancement of antigen presentation and subsequent primary T-cell and B-cell responses by alum adjuvants (7, 8). As there is an urgent need for the development of new adjuvants with improved immunogenicity and safety profiles, a clearer understanding of the role that the depot plays in alum adjuvant activity will clearly contribute to the rational design of these important vaccine components.
MATERIALS AND METHODS
Mice
Homozygous DO11.10x4get mice were prepared from 4get (9) and DO11.10 BALB/c TcR transgenic (tg) mice (10). Cell suspensions from secondary lymphoid organs of DO11.10x4get were labeled with the fluorescent dye Cell Tracker Orange 9′-(4-(and 5)-chloromethyl-2-carboxyphenyl)-7′-chloro-6′-oxo-1,2,2,4-tetramethyl-1,2-dihydropyrido[2′,3′-6]xanthene (CMRA); Invitrogen, Paisley, UK; ref. 11], then 3 × 106 T cells were transferred i.v. to 6- to 8-wk-old female BALB/c mice (Harlan, Bicester, UK). Procedures were performed according to the UK Home Office regulations.
Antigens and adjuvants
BALB/c mice were immunized with chromatographically purified chicken ovalbumin (OVA; Worthington Biochemical, Lakewood, NJ, USA), while C57BL/6 mice received EαGFP (12). Preparation of EαGFP and associated experimental protocols have been clearly described previously (13). Adjuvants were a 1% alum suspension (Brenntag Biosector, Frederikssund, Denmark), or 100 μg/ml CpG (CpG-ODN 1826; Coley Pharmacuetical Group, Ottawa, ON, Canada) or a combination of both. Mice received 100 μl s.c., 50 μl in the footpad or 10 μl in the ear pinna. Following ear pinna administration, the injection site (∼0.5 cm2) was removed under general anesthetic.
Flow cytometry
Cell suspensions were prepared from draining lymph nodes, as described above, and analyzed using the appropriate combinations of the following antibodies: CD4, KJ1.26, B220, CD11c, CD69, CD62L, or Y-Ae (BD Biosciences, Oxford, UK) in 100 μl of FACS buffer (PBS, 2% fetal calf serum, and 0.05% NaN3) containing Fc Block (2.4G2 hybridoma supernatant). Antigen-presenting cell (APC) populations were identified as B220-expressing B cells, CD11c-positive conventional DCs, and B220/CD11c-expressing plasmacytoid DCs (pDCs), as described previously (14, 15). Data were acquired on a FACSCanto flow cytometer (BD Biosciences) and analyzed using FlowJo software (Tree Star, Ashland, OR, USA).
Enzyme-linked immunosorbent assay (ELISA) and multiplex bead cytokine analysis
Antigen-specific IgG1 and IgG2a titers were determined in serum samples as described previously (16). Cytokine levels were determined in supernatants from in vitro restimulated, draining lymph node cell cultures by multiplex bead cytokine analysis (Invitrogen), according to the manufacturer's instructions.
Statistical analysis
Results are expressed as means ± sd. Intergroup significance was determined as appropriate, by Student's 2-tailed unpaired t test or 1-way ANOVA using Prism (GraphPad Software, La Jolla, CA, USA). A value of P ≤ 0.05 was considered significant.
RESULTS
Characterization of the adjuvant activity of alum and CpG
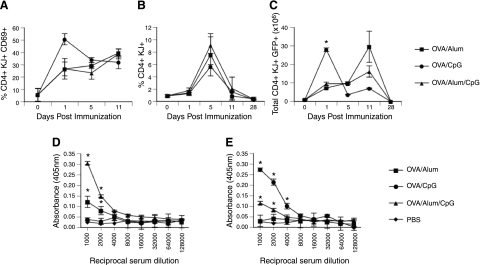
We analyzed the kinetics of T-cell activation, division, and differentiation in response to alum and compared this with CpG adjuvants. Synthetic oligonucleotides containing CpG motifs act via TLR9, expressed on a number of cell types, to create a proinflammatory environment (17). Although these two adjuvants are proposed to have quite distinct mechanisms of action, no difference in the magnitude and kinetics of antigen-specific T-cell activation (Fig. 1A), as revealed by CD69 expression (18) and T-cell expansion (Fig. 1B) in the draining lymph node, was observed following immunization. IL-4 production by antigen-specific T cells was reported by GFP expression (9) and revealed a transient population of T cells induced by CpG adjuvant (Fig. 1C), whereas the use of alum (or alum/CpG) favored sustained IL-4 production past d 5 following immunization. Previous studies have established that the use of alum is associated with Th2 response generation (16), compared with CpG, which favors generation of Th1 responses (19). Antibody subclass data confirmed this dichotomy, with alum promoting an IgG1-dominated antibody response associated with Th2 induction, and CpG adjuvants boosting only IgG2a responses that are dependent on Th1-derived IFNγ (16, 19). These responses were confirmed by analysis of cytokine production by in vitro antigen-restimulated T cells (data not shown).
Figure 1.
Magnitude and kinetics of antigen-specific immune responses are comparable following immunization with alum or CpG adjuvants. A) All adjuvants significantly increased the mean percentage of tg T cells (CD4+KJ1.26+) expressing CD69, at d 1, 5, and 11. B) Mean percentage of tg T cells at the peak of expansion at d 5 postimmunization. C) Total number of tg T cells expressing the IL-4 reporter was higher early (d 1; P<0.05) with CpG/OVA compared with alum/OVA, although later (d 11) only alum/OVA or alum/OVA/CpG produced significant numbers of GFP-positive antigen-specific cells compared with nonimmunized controls. D, E) Serum was taken from animals 14 d after immunization and assessed for the presence of anti-OVA IgG1 (D) and anti-OVA IgG2a (E) by ELISA. Results are means ± sd of 3 animals/group and are representative of ≥2 independent experiments. *P < 0.05 vs. unimmunized control; 1-way ANOVA.
Immunization with alum or CpG adjuvants gives rise to a comparable distribution, magnitude, and duration of antigen uptake and presentation in vivo
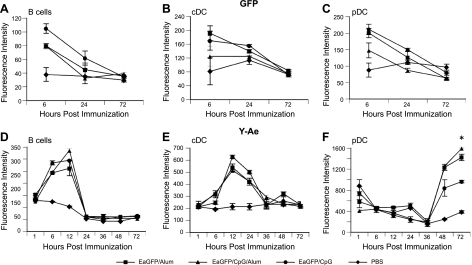
Given the similar kinetics of T-cell activation, we next analyzed whether the different adjuvant preparations affected the acquisition of antigen and the magnitude and duration of antigen presentation in vivo. This was achieved by tracking the fluorescence signal from the chimeric antigen EαGFP, together with a specific monoclonal antibody (Y-Ae; ref. 20) that recognizes presentation of the Eα peptide in the context of I-Ab (12, 13), i.e., it recognizes what the T-cell receptor sees (Supplemental Fig. S1). Antigen uptake (GFP accumulation) occurred rapidly and decayed simultaneously within each of the draining lymph node APC populations analyzed; B cells (Fig. 2A), conventional DCs (Fig. 2B), and plasmacytoid DCs (Fig. 2C). Significantly, alum did not appear to affect the dynamics of this acquisition and loss of signal, despite the proposed formation of a slow-release depot of antigen. B cells were the first APC population to become Y-Ae positive, at 6–12 h following immunization with alum adsorbed EαGFP (Fig. 2D and Supplemental Fig. S2), and choice of vaccine adjuvant did not appear to alter the magnitude or duration of antigen presentation by B cells. Conventional DCs presented antigen in a second, discrete wave, between 12 and 24 h after alum/EαGFP administration (Fig. 2E and Supplemental Fig. S2), and surprisingly, alum-induced depot formation did not alter the kinetics or magnitude of antigen presentation compared with either CpG or alum/CpG. With each of the adjuvants tested, plasmacytoid DCs represented a third discrete wave of antigen presentation in the draining lymph node at 48 to 72 h following antigen immunization (Fig. 2F and Supplemental Fig. S2). It was particularly striking that despite the proposed depot formation by alum, there was no difference in the kinetics of antigen uptake or presentation, or, indeed, the APC populations engaged in these processes in vivo, following immunization with antigen prepared in any of the adjuvants.
Figure 2.
Immunization with alum or CpG adjuvants gives rise to a comparable distribution, magnitude, and duration of antigen uptake and presentation in vivo. A–C) Duration and magnitude of antigen persistence were measured as the mean fluorescence intensity (MFI) of EαGFP protein detected at 6, 24, and 72 h postimmunization in B cells (A), CD11c DCs (B), and plasmacytoid DCs (C). D–F) Duration and magnitude of antigen presentation were measured as the MFI of Y-Ae detection of the Eα-MHCII complex at 1, 6, 12, 24, 36, 48, and 72 h postimmunization in B cells (D), CD11c DCs (E), and plasmacytoid DCs (F). Results are means ± sd of 3 animals/group and are representative of ≥3 independent experiments. *P < 0.05 for EαGFP/CpG vs. EαGFP/alum groups; 1-way ANOVA.
Immunization with alum results in a short-term persistence of antigen in comparison with CpG adjuvant
Previous in vitro studies have associated antigen persistence with enhanced T-cell activation and function (21) and, in particular, Th2 responses (22). Consequently, depot-forming adjuvants such as alum have been proposed to act in this fashion (23). However, the studies above suggest that alum does not affect the persistence of antigen or antigen presentation by APC, nor the magnitude and duration of T-cell expansion. As an indirect, but sensitive, measure of persisting antigen presentation in vivo, we transferred CMRA-labeled (11), antigen-specific DO.11.10 transgenic T cells (10) following immunization with antigen prepared in adjuvants (Fig. 3A). These studies demonstrated T-cell expansion (Fig. 3B), and division (Fig. 3C and Supplemental Fig. S3) could be detected when T cells were transferred up to 5 d following administration of antigen adsorbed to alum, but not together with CpG. However, T-cell activation was no longer detectable when cells were transferred 10 d following immunization with any adjuvant formulation tested, indicating that while the alum injection site can be observed for a considerable period of time (2, 24), immunologically recognized antigen only persists for a short period of time.
Figure 3.
Immunization with alum in comparison with CpG adjuvant results in a short-term persistence of antigen. A) Timeline outlining experiment protocol. B) Mean percentage of tg T cells at 5 d following immunization of mice that received an adoptive transfer of tg T cells 1, 5, 10, 14, and 28 d previously. C) Tg T cells (CD4+KJ1.26+) were counted and then assessed for CFSE division by flow cytometry. Results are means ± sd of 3 animals/group and are representative of ≥2 independent experiments. *P < 0.05 for OVA/alum vs. OVA/CpG; 1-way ANOVA.
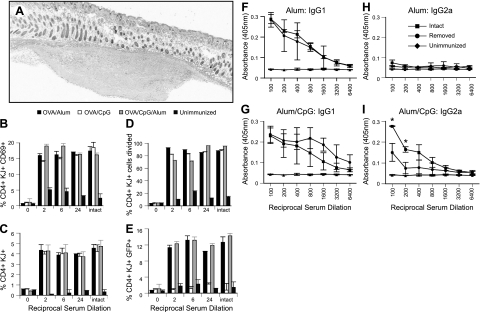
Removal of the depot does not alter the magnitude and kinetics of antigen-specific immune responses following alum immunization
Alum, and the associated injection site reaction, remain focal and discrete following subcutaneous administration, for example, in the footpad or ear (Fig. 4A). Consequently, it was relatively straightforward to directly address the importance of the depot by removing the injection site at various times following immunization and evaluating the effect of ablation on the resulting immune response. Immediate removal of the injection site after administration of antigen and adjuvant prevented any detectable activation of antigen-specific T cells, as measured by CD69 expression (Fig. 4B), T-cell expansion (Fig. 4C), division (Fig. 4D), and IL-4 production (revealed by GFP expression; Fig. 4E and ref. 9). However, much to our surprise, removal of the injection site as early as 2 h following antigen/adjuvant administration had no effect on these parameters (Fig. 4B–E). Further experiments removed the injection site 2 h after antigen/adjuvant administration and analyzed the resulting antibody response 14 d later (Figs. 4F–I). These studies demonstrated that alum-induced IgG1 titers were unaffected by injection site ablation (Fig. 4F) and confirmed the lack of Th1-associated IgG2a production previously observed (Fig. 4H). Interestingly, the IgG2a response induced by CpG/alum adjuvants did appear to be partially dependent on the intact injection site (Fig. 4I). In vitro restimulation and analysis of cytokines at 14 d after immunization confirmed that injection site ablation did not significantly affect the magnitude and profile of T-cell cytokine production (data not shown).
Figure 4.
Ear ablation does not alter the magnitude and kinetics of antigen-specific immune responses following alum immunization. A) Histological analysis demonstrates a discrete subcutaneous depot of alum up to 24 h after injection. Injection sites were subsequently removed immediately, or at 2, 6, or 24 h postimmunization. B–E) Effect of injection site removal on mean percentage of tg T cells expressing CD69 (B), mean percentage of tg T cells in draining lymph nodes (C), mean percentage of tg T cells (CD4+KJ1.26+) that divided (D), and mean percentage of tg T cells (CD4+KJ1.26+) expressing GFP, a marker of IL4 production, at 5 d postimmunization (E). F–I) Effect of injection site removal 2 h postimmunization on titers of anti-OVA IgG1 after immunization with OVA/alum (F), alum/CpG and titers of anti-OVA IgG2a (G), OVA/alum (H), and alum/CpG (I). Results are means ± sd of 3 animals/group and are representative of ≥2 independent experiments. *P<0.05 for intact vs. removed; 1-way ANOVA.
Removal of the depot does not alter the magnitude or phenotype of recall memory responses following alum immunization
While primary T- and B-cell responses were unaffected by removal of the alum depot, it remained possible that the depot and associated prolonged release of antigen affects recall memory responses. We therefore examined the effect of injection site ablation on the ability of mice to mount antigen-specific, recall immune responses (Fig. 5A). Surprisingly, injection site ablation induced a small increase in OVA-specific IgG1 titer at 1 wk postchallenge (Fig. 5C), although this was transient, and no effect of ablation on IgG1 responses was observed at other time points (Fig. 5D, E). Consistent with the results from Fig. 4, injection site ablation did not affect the inability of alum/OVA-immunized mice to produce Th1-associated, IgG2a responses.
Figure 5.
Ear ablation following OVA/alum immunization does not alter the magnitude or phenotype of recall memory responses. A) Mice were immunized with OVA adsorbed to alum, and the injection site was ablated 2 h later. After 2 wk, OVA-specific responses were recalled in control (intact) and ablated mice by immunization with heat-aggregated OVA (HAO). B–E) IgG1 responses were detectable prior to (B) and at 1 wk (C), 2 wk (D) or 3 wk (E) following challenge. Injection site ablation induced a small increase in IgG1 titer at 1 wk postchallenge; no effect of ablation was observed at other time points. F–I) Injection site ablation did not affect the inability of alum/OVA immunized mice to produce IgG2a responses at 1 wk (G), 2 wk (H) or 3 wk (I) postchallenge, compared to prechallenge (F). Results are means ± sd of 5 animals/group. ***P < 0.01.
Depot ablation does not alter the magnitude and duration of antigen uptake and presentation in vivo following immunization with alum
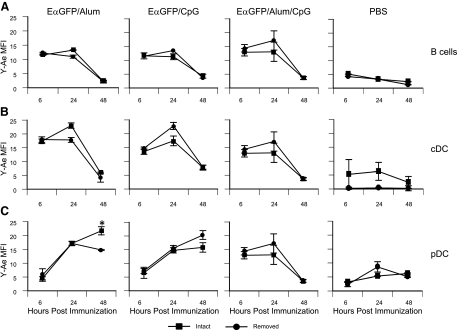
We therefore determined the influence of injection site ablation on the characteristic distribution of antigen uptake and presentation in vivo using the EαGFP/Y-Ae system described above. The uptake of GFP by B cells, conventional DCs, and plasmacytoid DCs peaked at 6 h and decreased thereafter, as shown above (Fig. 2A–C), and this was not affected by injection site ablation 2 h after EαGFP administration (data not shown). Notably, injection site ablation did not affect the magnitude of kinetics of antigen presentation by B cells (Fig. 6A) or conventional DCs (Fig. 6B) compared with intact mice, although there was a minor though significant reduction in presentation by plasmacytoid DCs, 72 h after immunization with alum (Fig. 6C).
Figure 6.
Ear ablation does not alter the magnitude and duration of antigen uptake and presentation in vivo following immunization with alum/EαGFP. Effect of injection site ablation at 2 h postimmunization on duration and magnitude of antigen presentation. Lymph nodes were collected at 6, 24, and 48 h postimmunization and antigen presentation by B cells (A), CD11c DCs (B), and plasmacytoid DCs (C) was expressed as Y-Ae mean fluorescence intensity. Results are means ± sd of 3 animals/group and are representative of ≥2 independent experiments. *P<0.05 for intact vs. removed; Student's 2-tailed unpaired t test.
DISCUSSION
In the current study, we have demonstrated that alum adjuvants fail to sustain antigen availability and presentation in draining lymph nodes, which would be inconsistent with a depot-forming mechanism of action. Irrespective of adjuvant used, antigen uptake by APC populations (B cells, conventional DCs, and plasmacytoid DCs) in the draining lymph node occurred rapidly and decayed simultaneously. Similar kinetics have previously been described with soluble antigen (12), and here, we show that alum did not appear to affect the dynamics of this acquisition and loss of signal, despite the proposed formation of a slow-release depot of antigen. Significantly, recent in vitro data demonstrated that in the presence of interstitial fluid, elution of antigen from alum occurs rapidly, within 1–2 h (25), suggesting that the majority of antigen administered in alum will travel to the draining lymph node in a soluble rather than adsorbed form.
Following uptake of antigen, we then analyzed presentation of antigen, directly ex vivo, using the Eα/Y-Ae system (12, 13). Despite the simultaneous acquisition of antigen by APCs noted above, presentation of antigen occurred in 3 discrete waves; B cells presented antigen within 6 h, conventional DCs after 12–24 h, and finally plasmacytoid DCs >48 h following antigen administration. Previous studies have demonstrated similar kinetics of B-cell and conventional DC antigen presentation in vivo following soluble antigen administration (12). Surprisingly, the choice of vaccine adjuvant did not appear to alter the magnitude or duration of antigen presentation, despite the ability of CpG adjuvants to directly activate APCs (26–28). Therefore, despite the supposed formation of an antigen depot by alum, the kinetics and cellular distribution of antigen uptake and presentation in vivo, appeared unaffected by the choice of adjuvant. These results are, therefore, consistent with previous studies demonstrating rapid elution of antigen from alum in vitro (25) and in vivo (29), directly questioning whether alum acts as an antigen depot at all. These results were broadly confirmed by studies demonstrating that adoptive transfer of antigen-specific transgenic T cells 10 d or longer after antigen/adjuvant treatment failed to respond. There were, however, some differential effects of adjuvants in maintaining this response, with alum prolonging T-cell responses to antigen compared with CpG. Likewise, antigen presentation by pDCs at 72 h was significantly higher when using alum adjuvant compared with CpG.
Nevertheless, these studies do not rule out a role for other adjuvant-driven, depot-associated events, such as injection site inflammation that could affect T-cell activation. Therefore, to directly address this, we removed the injection site from 2 to 24 h following administration of antigen and adjuvant. These data demonstrated that the alum injection site is dispensable for adjuvant activity within 2 h of administration, clearly ruling out any role for an antigen depot. Previous studies have demonstrated that removal of the alum injection site 7 d after immunization does not affect the production or maintenance of subsequent antibody responses (30). We have, therefore, extended these studies to show that the depot is not responsible for adjuvant-driven enhancement of the T-cell or the B-cell response. More significantly, the 7-d ablation studies described by Holt (30) allowed ample time for the development of a primary T-cell and subsequent B-cell response, which have been shown to initiate within 48 h of antigen injection (31). Therefore, in contrast to previous work, our current study more directly addresses the issue of the role of depot in the enhancement of primary T-cell responses by adjuvants. However, it remained possible that prolonged release of antigen from an alum depot would contribute more to memory than acute primary responses (32). We therefore analyzed the effect of depot ablation on the ability of mice to mount subsequent antigen-specific recall responses. Surprisingly, removal of the injection site had no effect on the magnitude or phenotype of the recall antibody response. Given the role of antigen in the maintenance of memory responses (32), this result strongly suggests that alum does not form an antigen depot at all. Interestingly, studies with Freund's adjuvants have also demonstrated that injection site ablation in a similar 2-h window does not affect induction of disease in an adjuvant-induced arthritis model (33).
The speed at which the depot becomes redundant was also surprising given the various adjuvant-host cell interactions that are thought to occur in these tissues in order to drive adjuvant enhancement of primary T-cell responses. First, inflammatory cells recruited into the site of inoculation of depot and inflammatory adjuvants have been thought to play an important role in mediating adjuvant activity (8, 34). Second, adjuvant-induced inflammation is thought to evoke activation of DCs at the injection site and consequently increase DC migration to draining lymph nodes (27, 35), and these migratory DCs are required for T-cell activation (12, 36). While alum is known to induce injection site inflammation (6, 8), clearly further studies are required to confirm when this process occurs, its role in adjuvant activity, and specifically, whether alum induces a migratory DC population and the role that these cells play in mediating adjuvant activity. Analysis of antigen presentation following alum/antigen injection site ablation produced a similar duration, sequence, and magnitude of antigen presentation as intact controls. The most likely explanation for this response is that antigen released from alum at the injection site moves to the draining lymph node as soluble antigen and is presented by lymph node resident rather than migratory DCs. However, this hypothesis remains to be formally tested.
In summary, our studies clearly demonstrate that antigen depot does not play an important role in alum adjuvant activity, demonstrating that this particular hypothesis, untested for over 80 yr, does not explain how these clinically important vaccine adjuvants function. This finding has two main implications in vaccine research. First, the tissue reactions induced by the alum depot that persist for several days, such as pain, redness and swelling, do not appear to be required for adjuvant activity. Second, in the absence of conclusive evidence for alternative mechanisms of action (8), it highlights that there are other processes involved in alum adjuvant activity, knowledge of which will clearly facilitate the rational design of novel and more effective vaccine adjuvants that are urgently required.
Supplementary Material
Acknowledgments
This work was funded by grants from the UK Biotechnology and Biological Sciences Research Council and The Wellcome Trust.
This article includes supplemental data. Please visit http://www.fasebj.org to obtain this information.
- APC
- antigen-presenting cell
- CMRA
- 9′-(4-(and 5)-chloromethyl-2-carboxyphenyl)-7′-chloro-6′-oxo-1,2, 2,4-tetramethyl-1,2-dihydropyrido[2′,3′-6]xanthene
- DC
- dendritic cell
- tg
- transgenic
- OVA
- ovalbumin
- pDC
- plasmacytoid dendritic cell
- TLR
- Toll-like receptor.
REFERENCES
- 1. Glenny A. T., Pope C. G. (1925) The antigenic effect of intravenous injection of diphtheria toxin. J. Pathol. Bacteriol. 28, 273–278 [Google Scholar]
- 2. Glenny A. T., Buttle G. A. H., Stevens M. F. (1931) Rate of disappearance of diphtheria toxoid injected into rabbits and guinea-pigs: toxoid precipitated with alum. J. Pathol. Bacteriol. 34, 267–275 [Google Scholar]
- 3. Van Duin D., Medzhitov R., Shaw A. C. (2006) Triggering TLR signaling in vaccination. Trends Immunol. 27, 49–49 [DOI] [PubMed] [Google Scholar]
- 4. Shi Y., Evans J. E., Rock K. L. (2003) Molecular identification of a danger signal that alerts the immune system to dying cells. Nature 425, 516–521 [DOI] [PubMed] [Google Scholar]
- 5. Gavin A. L., Hoebe K., Duong B., Ota T., Martin C., Beutler B., Nemazee D. (2006) Adjuvant-enhanced antibody responses in the absence of Toll-like receptor signaling. Science 314, 1936–1938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McKee A. S., Munks M. W., MacLeod M. K. L., Fleenor C. J., Van Rooijen N., Kappler J. W., Marrack P. (2009) Alum induces innate immune responses through macrophage and mast cell sensors, but these sensors are not required for alum to act as an adjuvant for specific immunity. J. Immunol. 183, 4403–4414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Oakley C. L. (1966) Alexander Thomas Glenny. 1882–1965. Biog. Mem. Fellows R. Soc. 12, 163–180 [Google Scholar]
- 8. Marrack P., McKee A. S., Munks M. W. (2009) Towards an understanding of the adjuvant action of aluminium. Nat. Rev. Immunol. 9, 287–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mohrs M., Shinkai K., Mohrs K., Locksley R. M. (2001) Analysis of type 2 immunity in vivo with a bicistronic IL-4 reporter. Immunity 15, 303–311 [DOI] [PubMed] [Google Scholar]
- 10. Murphy K. M., Heimberger A. B., Loh D. Y. (1990) Induction by antigen of intrathymic apoptosis of CD4+CD8+TCRlo thymocytes in vivo. Science 250, 1720–1723 [DOI] [PubMed] [Google Scholar]
- 11. Hawkins E. D., Hommel M., Turner M. L., Battye F. L., Markham J. F., Hodgkin P. D. (2007) Measuring lymphocyte proliferation, survival and differentiation using CFSE time-series data. Nat. Protoc. 2, 2057–2067 [DOI] [PubMed] [Google Scholar]
- 12. Itano A. A., McSorley S. J., Reinhardt R. L., Ehst B. D., Ingulli E., Rudensky A. Y., Jenkins M. K. (2003) Distinct dendritic cell populations sequentially present antigen to CD4 T cells and stimulate different aspects of cell-mediated immunity. Immunity 19, 47–57 [DOI] [PubMed] [Google Scholar]
- 13. Rush C. M., Brewer J. M. (2010) Tracking dendritic cells in vivo. Methods Mol. Biol. 626, 169–185 [DOI] [PubMed] [Google Scholar]
- 14. Jongbloed S. L., Benson R. A., Nickdel M. B., Garside P., McInnes I. B., Brewer J. M. (2009) Plasmacytoid dendritic cells regulate breach of self-tolerance in autoimmune arthritis. J. Immunol. 182, 963–968 [DOI] [PubMed] [Google Scholar]
- 15. Benson R. A., Patakas A., Conigliaro P., Rush C. M., Garside P., McInnes I. B., Brewer J. M. (2010) Identifying the cells breaching self-tolerance in autoimmunity. J. Immunol. 184, 6378–6385 [DOI] [PubMed] [Google Scholar]
- 16. Brewer J. M., Conacher M., Mohrs M., Brombacher F., Alexander J. (1999) Aluminium hydroxide adjuvant initiates strong antigen specific Th2 responses in the absence of IL-4 or IL-13 mediated signalling. J. Immunol. 163, 6448–6454 [PubMed] [Google Scholar]
- 17. Hemmi H., Takeuchi O., Kawai T., Kaisho T., Sato S., Sanjo H., Matsumoto M., Hoshino K., Wagner H., Takeda K., Akira S. (2000) A Toll-like receptor recognizes bacterial DNA. Nature 408, 740–745-740–745 [DOI] [PubMed] [Google Scholar]
- 18. Ziegler S. F., Levin S. D., Johnson L., Copeland N. G., Gilbert D. J., Jenkins N. A., Baker E., Sutherland G. R., Feldhaus A. L., Ramsdell F. (1994) The mouse CD69 gene. Structure, expression, and mapping to the NK gene complex. J. Immunol. 152, 1228–1236 [PubMed] [Google Scholar]
- 19. Weiner G. J., Liu H. M., Wooldridge J. E., Dahle C. E., Krieg A. M. (1997) Immunostimulatory oligodeoxynucleotides containing the CpG motif are effective as immune adjuvants in tumor antigen immunization. Proc. Natl. Acad. Sci. U. S. A. 94, 10833–10837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Murphy D. B., Rath S., Pizzo E., Rudensky A. Y., George A., Larson J. K., Janeway C. A. (1992) Monoclonal antibody detection of a major self peptide. MHC class II complex. J. Immunol. 148, 3483–3491 [PubMed] [Google Scholar]
- 21. Obst R., van Santen H. M., Mathis D., Benoist C. (2005) Antigen persistence is required throughout the expansion phase of a CD4+ T cell response. J. Exp. Med. 201, 1555–1565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Guery J. C., Galbiati F., Smiroldo S., Adorini L. (1996) Selective development of T helper (Th)2 cells induced by continuous administration of low dose soluble proteins to normal and beta(2)- microglobulin-deficient BALB/c mice. J. Exp. Med. 183, 485–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brewer J. M. (2006) (How) do aluminium adjuvants work? Imm. Lett. 102, 10–15 [DOI] [PubMed] [Google Scholar]
- 24. Harrison W. T. (1935) Some observations on the use of alum precipitated diphtheria toxoid. Am. J. Public Health Nations Health 25, 298–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hansen B., Sokolovska A., HogenEsch H., Hem S. L. (2007) Relationship between the strength of antigen adsorption to an aluminum-containing adjuvant and the immune response. Vaccine 25, 6618–6624 [DOI] [PubMed] [Google Scholar]
- 26. Kreig A. M., Yi A. K., Matson S., Waldschmidt T. J., Bishop G. A., Teasdale R., Koretzky G. A., Klinman D. M. (1995) CpG motifs in bacterial DNA trigger direct B cell activation. Nature 374, 546–549 [DOI] [PubMed] [Google Scholar]
- 27. Randolph G. J., Angeli V., Swartz M. A. (2005) Dendritic-cell trafficking to lymph nodes through lymphatic vessels. Nat. Rev. Immunol. 5, 617–628 [DOI] [PubMed] [Google Scholar]
- 28. Kaisho T., Akira S. (2002) Toll-like receptors as adjuvant receptors. Biochim Biophys Acta 1589, 1–13 [DOI] [PubMed] [Google Scholar]
- 29. Weissburg R. P., Berman P. W., Cleland J. L., Eastman D., Farina F., Frie S., Lim A., Mordenti J., Nguyen T. T., Peterson M. R. (1995) Characterization of the MN gp120 HIV-1 vaccine: antigen binding to alum. Pharm. Res. 12, 1439–1446 [DOI] [PubMed] [Google Scholar]
- 30. Holt L. B. (1950) Developments in Diphtheria Prophylaxis, Heinemann, London [Google Scholar]
- 31. Catron D. M., Itano A. A., Pape K. A., Mueller D. L., Jenkins M. K. (2004) Visualizing the first 50 hr of the primary immune response to a soluble antigen. Immunity 21, 341–341 [DOI] [PubMed] [Google Scholar]
- 32. Gray D., Matzinger P. (1991) T cell memory is short-lived in the absence of antigen. J. Exp. Med. 174, 969–974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ward J. R., Jones R. S. (1962) Studies on adjuvant-induced polyarthritis in rats. I. Adjuvant composition, route of injection, and removal of depot site. Arthritis Rheum. 5, 557–564 [DOI] [PubMed] [Google Scholar]
- 34. Jordan M. B., Mills D. M., Kappler J., Marrack P., Cambier J. C. (2004) Promotion of B cell immune responses via an alum-induced myeloid cell population. Science 304, 1808–1810 [DOI] [PubMed] [Google Scholar]
- 35. Banchereau J., Briere F., Caux C., Davoust J., Lebecque S., Liu Y. J., Pulendran B., Palucka K. (2000) Immunobiology of dendritic cells. Annu. Rev. Immunol. 18, 767–811 [DOI] [PubMed] [Google Scholar]
- 36. Allenspach E. J., Lemos M. P., Porrett P. M., Turka L. A., Laufer T. M. (2008) Migratory and lymphoid-resident dendritic cells cooperate to efficiently prime naive CD4 T cells. Immunity 29, 795–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.