Abstract
In the current paper, we explore the efficacy of a four-hour self-forgiveness intervention. Participants (N = 79) undergoing a routine alcohol treatment protocol were randomly assigned to an intervention or treatment as usual condition. Those in the intervention condition completed the self-forgiveness intervention. All participants completed measures of self-forgiveness, drinking refusal self-efficacy, guilt and shame over an alcohol related transgression. Participants in the intervention condition reported more positive gains on measures of self-forgiveness and drinking refusal efficacy as well as guilt and shame related to alcohol-related offenses. Implications of the self-forgiveness intervention for alcohol misusing populations are discussed.
Keywords: Self-Forgiveness, Alcohol, Guilt, Shame, Self-Efficacy
Alcohol is the most commonly misused drug in the United States (Johnston, O’Malley, Bachman, & Schulenberg, 2009). Alcohol use, misuse, and abuse has been associated with diminished physical (Mojtabai & Singh, 2007) and mental health (Dongier, 2005; Li, Hewitt, & Grant, 2004; Snyder & Heinze, 2005), and is often considered a maladaptive coping strategy (Grüsser, Mörsen, & Flor, 2006; Holahan, Moos, Holahan, Cronkite, & Randall, 2001; Tapert, Ozyurt, & Myers, 2004; Young & Oei, 1993).
Those working within the realm of substance abuse treatment frequently address alcohol misuse (a pattern of behavior in which alcohol consumption interferes with some aspect of daily life; Edwards & Unnithan, 1994) and abuse (a clinical diagnosis; American Psychiatric Association, 1994) in their work (Birky, 2005; Harris, Aldea, & Kirkley, 2006; Scholl & Schmitt, 2009). Health care providers and mental health practitioners frequently work in situations in which alcohol use, misuse and abuse is prevalent, and they are tasked with finding ways in which to address these concerns. Mental health problems are often compounded by dual diagnoses involving substance abuse or dependence (Martens, et al., 2008). Thus, the treatment of alcohol misuse and abuse is a topic that is relevant for professionals working with substance abuse scientifically as well as clinically.
Individuals who misuse alcohol may feel emotions such as shame and guilt for damaging behaviors performed while intoxicated (e.g., arguing with a family member, getting a DUI, etc.), or about the misuse itself (Worthington, Scherer, & Cooke, 2006). Alcohol misuse may also result in reduced trust and forgiveness within their families or primary support network (Scherer et al., 2010), which may cause further friction, conflict, and elevate feelings of guilt and shame.
When considering guilt and shame, a careful distinction must be made between the two. Guilt and shame are generally perceived as two distinct and separate emotional states (Tangney & Dearing, 2002; Woien, Ernst, Patock-Peckham, & Nagoshi, 2003). Guilt is generally focused on an event (i.e., I did something wrong) whereas shame is generally focused on the person (i.e., I am a bad person; Dearing, Stuewig, & Tangney, 2005). Feelings of shame in particular have been found to be detrimental to self-esteem and hopefulness, and may increase the propensity to turn to alcohol or drugs in an attempt to cope with these feelings (Strelan, 2007; Yelsma, Brown, & Elison, 2002). Shame has been associated with lower levels of self-esteem and higher levels of stress and psychiatric symptomatology, whereas guilt was unrelated to these constructs (Woien et al., 2003).
Unlike feelings of shame, however, feelings of guilt can have both positive and negative consequences. Limited amounts of guilt can motivate a person to take actions to improve his or her situation. Because these feelings are often painful, people experiencing them may be motivated to work to lessen or assuage these feelings. For example, guilt can motivate people to (a) repair problems in their relationships and attempt to make amends to those they have wronged (Fisher & Exline, 2006), (b) make confessions to their deity and renew spiritual commitments, and (c) change their behaviors and enter treatment.
On the other hand, feelings of guilt and shame that are prolonged or unwarranted may cause people to feel overwhelmed, hopeless, and depressed. These feelings may make it less likely or even impossible for people to take the necessary actions to improve their situation (Shields & Hufford, 2005). Feelings of guilt and shame also may be detrimental to physical and mental health and result in the internalization of a negative self-image.
Coping with Guilt and Shame
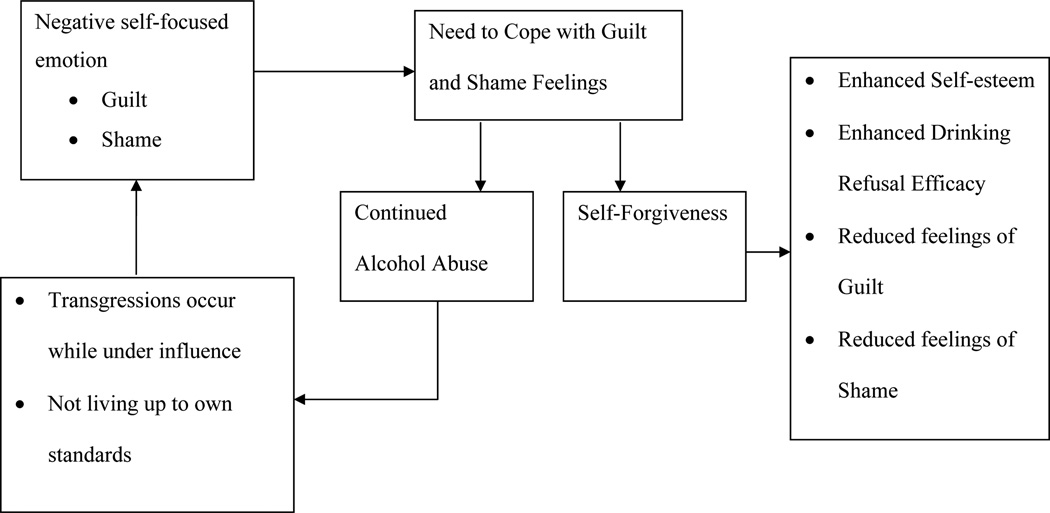
Investigators have found links between feelings of (a) guilt and shame and (b) alcohol and drug use (Dearing et al., 2005; Ianni et al., 2010; Webb et al., 2006). Alcohol misuse can result in the misuser committing interpersonal transgressions against friends or family members. After transgressions, the alcohol misuser may reflect on what he or she said or did and may make judgments about himself or herself. These self-judgments, then, may lead to feelings of guilt and shame not only about alcohol-related transgression, but also how the individual may have failed to live up to his or her own standards even if wrongdoing per se did not occur (Hall & Fincham, 2005; Worthington, 2006). These intense feelings of guilt and shame, in turn, may result in a decreased sense of the individual’s self-efficacy (Baldwin, Baldwin, & Ewald, 2006) and self-esteem (Strelan, 2007; Yelsma, Brown, & Elison, 2002). This decreased self-efficacy and self-esteem, in turn, may promote further feelings of guilt and shame (see Figure 1, which depicts a hypothesized model relating these constructs).
Figure 1.
Hypothesized causal model from self-judgment to improved sense of self
The individual must cope with these negative self-evaluations and self-focused emotions. One positive way to cope may be authentically forgiving oneself. This self-forgiveness can be directed at forgiving specific wrongdoings, forgiving oneself for failing to live up to one’s standards and expectations (even if wrongdoing was not present), or both (Fisher & Exline, 2006; Hall & Fincham, 2005; Worthington, 2006). Promoting self-forgiveness could result in enhanced perceptions of the self including enhanced self-esteem (Strelan, 2007), self-efficacy, and reduced guilt and shame (Hall & Fincham, 2005; Ianni et al., 2010; Worthington, 2006).
If feelings of guilt and shame play a significant role in an individual’s motivation to drink, it is important to study ways to alleviate inappropriate guilt and shame. That is, if guilt and shame contribute to alcohol use and relapse, studying strategies to reduce these feelings would be important to help individuals regulate or stop their drinking. In particular, self-forgiveness has been posited as a way to lower shame over falling short of one’s standards and guilt over transgressions (Ianni et al., 2010; Worthington, 2006), but there has been little research exploring interventions to promote self-forgiveness. Such interventions, which can be targeted to different populations of those who misuse alcohol (i.e., beginning drinkers, frequent or binge drinkers, out-patients who aim to stop or reduce drinking, and inpatients in detox or short-term residential programs) are sorely needed.
Forgiveness and Alcohol Use, Misuse, and Abuse
The study of forgiveness in individuals dealing with alcohol use, misuse, and abuse has recently gained the attention of researchers. Forgiveness has been examined with catalysts to the consumption of alcohol such as anger within the individual who misuses alcohol (Lin et al., 2005), the roles of shame and guilt within the misuser (Ianni et al., 2010; Worthington et al., 2006), and how forgiveness may influence the perception of family members of alcohol misusers (Scherer et al., 2011).
Individuals who use, misuse, or abuse alcohol are likely to experience feelings of shame and guilt (Collins, Morsheimer, Shiffman, & Paty, 2005; Dearing, Stuewig, & Tangney, 2005; Saunders, Zygowicz, & D’Angelo, 2006; Webb et al., 2006). These negative emotions may cause individuals to further misuse alcohol as a coping mechanism (Webb et al., 2006). Although one may deal with feelings of guilt and shame in many ways, the focus of the current study is self-forgiveness. Thus, improving self-forgiveness may reduce feelings of shame and guilt, and thereby reduce the use of alcohol as a coping mechanism. This, in turn, may decrease the probability of relapse during treatment. Unfortunately, to date, no studies have been conducted promoting self-forgiveness interventions with individuals who use, misuse, or abuse alcohol. Traditional treatments have largely focused on penalizing the misuser for their misuse rather than exploring forgiveness.
Treatment of Problems of Substance Abuse and Related Self-Condemnation
There are a variety of interventions to promote cessation from drinking (Webb, Robinson, & Brower, 2009; Webb, Robinson, Brower, & Zucker, 2006). Outside of 12-step programs, the role of self-forgiveness in substance abuse treatment is often overlooked (Webb & Trautman, 2010). Some investigators have written about self-forgiveness as it pertains to alcohol use and misuse (Enright & Fitzgibbons, 2000; Worthington, Scherer, & Cooke, 2006; Webb & Trautman, 2010). A few studies have investigated treatment and forgiveness of others. For example, Lin, Mack, Enright, Krahn, and Baskin (2005) conducted a study utilizing forgiveness therapy on hostile emotions with clients who misuse substances. They hypothesized that the elevation of anger, depression, vulnerability and anxiety found in alcohol (and drug) misusers act as a catalyst to pursue alcohol (or drugs) as a coping response. Hence by reducing these emotions, one would also reduce the need to use alcohol. Fourteen participants were referred by their therapists and randomly assigned to and completed either the 12-week forgiveness therapy condition – which was a forgiveness intervention targeted to reducing anger – or the standard 12-week alcohol and drug psychotherapy condition – that was not focused on anger reduction. Participants completed measures of forgiveness before and after the intervention.
In their study, Lin et al. found that participants’ forgiveness scores raised significantly from pre-test (where the scores were well below the average of a non-clinical population) to post-test (where the scores were comparable to the average of a non-clinical population). Lin et al.’s intervention did not simply reduce anger and anxiety, but it also moved the participants closer to average non-clinical profiles. They concluded, then, that forgiveness is a powerful tool as a supplement to interventions, not as a substitute.
In contrast to promoting forgiveness of others, promoting self-forgiveness may increase hopefulness (Strelan, 2007), which may promote drinking refusal efficacy. It also has been hypothesized to deal directly with self-blame that yields guilt and shame, which have been implicated in drinking immoderately. Self-forgiveness, if promoted by an intervention, could increase drinking refusal self-efficacy, and thus likely reduce drinking. The extant literature indicates individuals high in refusal efficacy are less likely to use substances in response to perceived stress (Scheier, Botvin, & Diaz, 1999). Refusal efficacy, then, likely plays a key role in helping an individual to avoid substance use and misuse. Promoting self-forgiveness, then, may promote self-esteem and increase an individual’s confidence that he or she will be able to avoid drinking in the future.
The current study is the first intervention study of self-forgiveness with outpatients in alcohol treatment programs. In it, we designed a brief self-forgiveness intervention, which is consistent with theorizing about interventions to promote self-forgiveness in Worthington (2006). Specifically, the purpose of the current study was to determine whether a brief (four-hour) self-forgiveness intervention used as an adjunct to outpatient treatment as usual (TAU) could (a) promote self-forgiveness, (b) enhance an individual’s drinking refusal self-efficacy, (c) decrease reported levels of guilt, and (d) decrease reported levels of shame when compared to a treatment as usual condition.
Methods
Participants
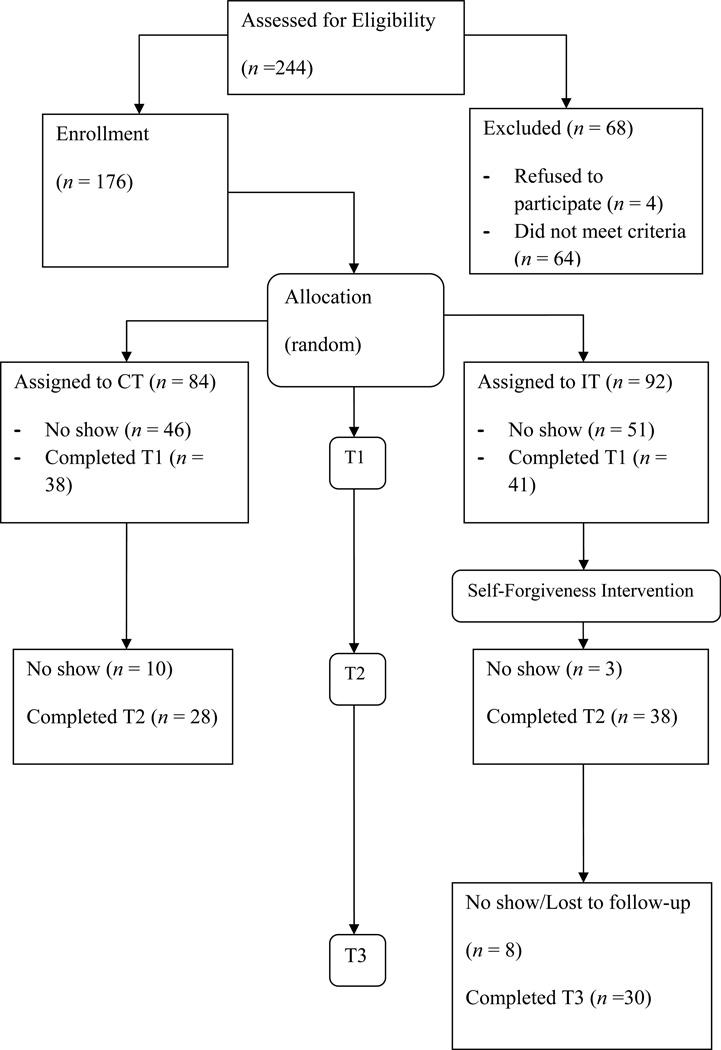
Participants (randomized, n = 176; analyzed, n = 79) were recruited from an alcohol abuse treatment program at one of two community-based mental health centers in Western Michigan. The participant selection process is described in Figure 2. Two-hundred forty-four individuals were assessed for eligibility. Participants were eligible to participate in the study if they were (a) at least 18 years of age, (b) met the requirements for a clinical diagnosis of either alcohol abuse or dependence as outlined by the Diagnostic and Statistical Manual-IV (DSM-IV; American Psychiatric Association, 1994), and (c) enrolled in outpatient group psychotherapy at the mental health center for alcohol abuse. As noted in Figure 2, 176 individuals were eligible for the study and were randomly assigned to either the intervention or TAU conditions, but only 79 individuals completed at least T1 questionnaires and were included in the current analyses.
Figure 2.
CONSORT Flow chart
Prior to data collection, this study was approved by the institutional review board at Virginia Commonwealth University. Participation in the study was optional. All participants were enrolled in standard alcohol abuse treatment psychotherapy throughout the course of the study. Participants were given a detailed description of the study and the procedures necessary for its completion and then consented to participate. Participants completed questionnaires at three points in time (i.e., pretest, posttest, 3-week follow-up). Of the participants assessed at T1 (n = 79), 84% returned for T2 (n = 66). Of the 38 participants in the intervention condition who completed T2, 79% completed follow-up data at T3. The participants in the TAU condition were given the option of completing the intervention after T2, and thus were not analyzed after T2.
Participant characteristics
Participants were 79 individuals (67 male, 12 female) in an alcohol abuse treatment program at one of two community-based mental health centers in Western Michigan. Participants reported a mean age of 36.1 years (SD = 12.6), and primarily identified as European American (n = 75, 94.9%). All were enrolled in outpatient group psychotherapy for alcohol abuse and were court-mandated to complete community service or attend psychoeducational groups in addition to attending treatment. The standard addictions treatment used in this treatment facility allows individuals to enter at any point. Therefore, some individuals participating in the study had more time in the standard addictions treatment setting than did others. However, no participants had more than 4 weeks of standard addictions treatment prior to the study, and randomization equalized the amount of treatment across groups. Participation in the present study was optional, and participants were not reimbursed for participating; however, participants were able to count participation in this psychoeducational intervention as partial fulfillment of the supplement to their court mandated psychotherapy.
Group leaders
Group leaders were Master’s level counselors trained in both substance abuse treatment and general group psychotherapy, and were licensed to practice in the state of Michigan. All group leaders received a two-hour training session in how to conduct the manualized self-forgiveness intervention.
The Intervention to Promote Self-Forgiveness
The intervention was designed to promote self-forgiveness. The intervention lasted four hours and was designed to be completed in three 90-minute sessions over three consecutive weeks. The first ten minutes of each session were spent recapping the material from the previous week. The remaining time was spent on the self-forgiveness intervention. The self-forgiveness intervention followed a manual for leaders and participants. Participants in the intervention condition completed measures of self-forgiveness, drinking refusal efficacy, and state guilt and shame (outlined below) at the onset of the intervention (T1), after the intervention (T2), and at three-week follow-up (T3). Participants in the TAU condition did not receive the intervention as part of the study, but were given the option to do so after T2. Participants in the TAU condition completed the same measures at T1 and T2. Using Campbell and Stanley (1966) notation of “X” for intervention and “O” for observation, the design can be represented as follows:
| Week 1 | Week 4 | Week 7 | ||
| Intervention Condition: | O1 | X | O2 | O3 |
| TAU Condition: | O1 | O2 |
The self-forgiveness intervention adapted for alcohol misuse was created for the present study (manuals for leaders and participants are available upon request from the corresponding author). The intervention was based on previous theorizing on the role of forgiveness in alcohol misuse (Worthington et al., 2006), self-forgiveness (Fisher & Exline, 2006; Hall & Fincham, 2005; Worthington, 2006), and motivational interviewing (Miller & Rollnick, 2002). The intervention uses motivational interviewing techniques to reduce resistance to participating in the intervention and to promote motivations to change. Following the motivational interviewing portion, the study adapts Worthington’s five-step model to REACH forgiveness to self-forgiveness (see Worthington, 2006 for a summary of research support and for guidelines to adapt for self-forgiveness). Though Worthington’s model was created to deal primarily with interpersonal forgiveness, it was adapted, for the current study, to focus on forgiving the self—including considerations of wrongdoing associated with alcohol misuse and failure to meet one’s expectations and standards for reduction or cessation of alcohol misuse. Generally, in line with motivational interviewing, a self-discovery method was used rather than a direct educational method.
Measures
State self-forgiveness
State self-forgiveness was measured using Self-Forgiving Feeling and Action (SFFA; Wohl, DeShea, & Wahkinney, 2008). Participants completed 17 items measuring the degree to which their own feelings and actions were congruent with self-forgiveness (e.g., “I regret what I did”). Participants rated how they feel right now in regards to their transgression and rated items on a ten point scale from 1 = don’t feel like this to 10 = feel very much like this. For the current sample, the SFFA was found to have a Cronbach’s alpha of .79 (95% CI = .65–.87).
Drinking refusal self-efficacy
Drinking refusal self-efficacy was measured using the Drinking Refusal Self-Efficacy Questionnaire-Revised (DRSEQ-R; Oei, Hasking, & Young 2005). Participants completed 19 items assessing how likely they felt they were able to resist a drink in a situation (e.g., “How sure are you that you’ll have a drink when you go to dinner”). Participants rated each item on a six point scale from 1 = I am sure I would have a drink, to 6 = I am sure I would NOT have a drink. High scores on the DRSEQ indicate high self-efficacy to refuse a drink. Estimates of six-week test-retest temporal stability ranged from .84 to .93 (Cronbach’s alpha = .84). There is evidence supporting the construct validity of this measure. For example, differences in drinking refusal efficacy were observed between clinical and non-clinical populations (Oei et al., 2005). For the current sample, the Cronbach’s alpha for the DRSEQ was .97 (95% CI = .95–.99).
Guilt and shame
Guilt and shame were measured using the Personal Feelings Questionnaire-2 (PFQ-2; Harder & Lewis, 1987). The PFQ-2 is a 22-item measure of guilt and shame. The scale consists of ten items that measure guilt (e.g., remorse, regret; PFQ-2-G) and six items that measure shame (e.g., feeling you deserve to be punished for what you did, feeling stupid; PFQ-2-S) as well as six filler items (e.g., euphoric, enjoyment). Participants rate the degree to which they experience each of the emotions on a five point scale from 0 = I do not experience the feeling to 4 = I experience the feeling very strongly. Higher scores indicate stronger experiences of guilt or shame. Estimates of internal consistency (Cronbach’s alpha) for the guilt and shame subscales were.72 and .78 respectively (Harder & Greenwald, 1999). For the purposes of the present study, the instructions for this scale asked participants to consider a specific drinking-related offense when completing the questionnaire. For the current sample, the Cronbach’s alphas for the guilt and shame subscales were .66 (95% CI = .47–.74) and .88 (95% CI = .82–.93) respectively.
Data Analysis
The primary aim of this research study was to evaluate the effectiveness of a self-forgiveness intervention on variables of self-forgiveness, drinking refusal self-efficacy, guilt, and shame. The data are grouped as repeated measures nested within individuals. Multilevel modeling is a statistical method that is appropriate for such data, as it allows for the examination of individual growth trajectories by analyzing the information contained in the repeated measures (Raudenbush & Bryk, 2002). Multilevel modeling is also able to analyze data from individuals with an unequal number of repeated observations. A two-level multilevel model was used for the present analyses that consisted of repeated measures (level 1) nested within individuals (level 2). The basic multilevel model took the following form:
where t indexes time and i indexes individuals. For these analyses, we included a random intercept at the individual level, which allows for individual-specific intercepts. Condition (intervention vs. TAU) was entered as a level-2 covariate. Multilevel models assume normality and homoscedasticity of all error terms and conditional independence of the outcome, given the random effects.
Results
Fidelity checks were completed by participants to ensure group leader adherence to the manual. Participants completed check lists of materials covered at each session as a means to ensure the participants in the TAU did not cover any material covered exclusively in the self-forgiveness intervention protocol. No breaches of fidelity were found in the current study.
Prior to conducting the primary analyses, we examined the data for missing items, outliers, and deviations from normality. If a participant completed less than 80% of the items on a scale, a total scale score was not computed. For those participants who failed to complete less than 20% of the items on a scale, the mean score for individual items was imputed (7% or less per item). All outliers were found to fall inside the expected range of values. As such, these values are believed to represent true responses and were retained for analysis.
Means and standard deviations for each variable by condition and time are listed in Table 1. We conducted a series of independent-sample t-tests to determine whether there were any differences between conditions at the beginning of the study. Participants in the intervention and TAU conditions had similar levels of self-forgiveness (p = .122), drinking refusal self-efficacy (p = .805), and shame (p = .856). Participants in the TAU condition had higher levels of guilt than did participants in the intervention condition (p = .004).
Table 1.
Means and Standard Deviations of Dependent Variables by Time and Condition
| Condition Variable |
Intervention Condition | Wait Control Condition | |||||
|---|---|---|---|---|---|---|---|
| Time | N | Mean | SD | N | Mean | SD | |
| Self- Forgiveness | 1 | 41 | 25.73 | 12.75 | 38 | 21.66 | 10.12 |
| 2 | 38 | 38.13 | 3.67 | 28 | 18.04 | 6.54 | |
| 3 | 30 | 39.17 | 3.89 | -- | -- | -- | |
| Drinking Refusal Self- Efficacy |
1 | 41 | 74.64 | 22.50 | 38 | 75.87 | 21.23 |
| 2 | 38 | 92.58 | 15.26 | 28 | 80.96 | 20.72 | |
| 3 | 30 | 95.67 | 14.21 | -- | -- | -- | |
| Guilt | 1 | 41 | 11.68 | 3.89 | 38 | 14.61 | 4.81 |
| 2 | 38 | 7.47 | 4.73 | 28 | 15.46 | 4.81 | |
| 3 | 30 | 7.30 | 3.89 | -- | -- | -- | |
| Shame | 1 | 41 | 16.34 | 7.47 | 38 | 16.66 | 7.05 |
| 2 | 38 | 14.87 | 6.15 | 28 | 18.68 | 6.86 | |
| 3 | 30 | 13.07 | 5.36 | -- | -- | -- | |
The main hypothesis was that participants in the intervention condition would report more improvement over time on measures of (a) self-forgiveness, (b) drinking refusal self-efficacy, (c) guilt, and (d) shame compared to participants in the TAU condition. To test these hypotheses, we conducted a series of multilevel models with self-forgiveness, drinking refusal self-efficacy, guilt, and shame as outcome variables, and time, condition (intervention vs. TAU) and the interaction between time and condition as predictor variables. For these analyses, a significant interaction would indicate differential improvement over time in the intervention vs. TAU condition.
For self-forgiveness, there was a significant interaction between condition and time, B = 16.37, SE = 2.35, t(66.85) = 6.96, p < .001. Participants in the intervention condition reported greater increases in self-forgiveness over time than did participants in the TAU condition.
For drinking refusal self-efficacy, there was a significant interaction between condition and time, B = 13.33, SE = 5.20, t(70.32) = 2.56, p = .013. Participants in the intervention condition reported greater increases in drinking refusal self-efficacy over time than did participants in the TAU condition.
For guilt, there was a significant interaction between condition and time, B = −4.81, SE = 1.19, t(68.96) = 4.04, p < .001. Participants in the intervention condition reported greater decreases in guilt over time than did participants in the TAU condition.
For shame, there was a significant interaction between condition and time, B = −3.52, SE = 1.37, t(67.96) = 2.57, p = .012. Participants in the intervention condition reported greater decreases in shame over time than did participants in the TAU condition.
Participants in the intervention condition completed the assessment measures again three weeks after the end of the intervention. Thus, we tested the extent to which gains were maintained from T2 (end of intervention) to T3 (3 week follow-up). To test this hypothesis, we conducted a series of multilevel models with self-forgiveness, drinking refusal self-efficacy, guilt, and shame as outcome variables, and time (time 2 to time 3) as the predictor variable. For these analyses, a non-significant effect of time would indicate treatment gains were maintained (e.g., there would be no significant decrease in self-forgiveness from the end of the intervention to the 3-week follow-up). For self-forgiveness, drinking refusal self-efficacy, and guilt, participants in the intervention condition reported no change from T2 to T3, indicating maintenance of treatment gains. For shame, participants in the intervention condition reported a decrease from T2 to T3, B = −1.47, SE = .49, t(30.88) = 3.04, p = .005, indicating that participants continued to report decreases in shame even after the intervention was completed.
Discussion
In this study, we tested the efficacy of an adjunctive intervention to promote self-forgiveness within a community sample undergoing outpatient treatment for alcohol abuse. Though it has been previously theorized that self-forgiveness would be correlated with health concerns including reduced problematic drinking (Worthington, Scherer & Cooke, 2006), there is little empirical evidence supporting this link. Previous research has established a relationship between alcohol use and self-forgiveness (Ianni et al., 2010; Webb et al., 2006), but there has been no research that has examined promoting self-forgiveness in the context of alcohol use. The present study represents one of the first steps in applying the forgiveness and self-forgiveness literatures to practical use by creating an intervention focused on self-forgiveness for alcohol-related transgressions to augment traditional alcohol treatment protocols.
As we hypothesized, participants in the intervention condition reported greater overall improvement over time in self-forgiveness, drinking refusal self-efficacy, guilt and shame than did participants in the TAU condition. That is, those in the intervention condition reported greater self-forgiveness and drinking refusal efficacy as well as decreased guilt and shame over a drinking-related transgression than did those in the TAU condition.
Further examination of the growth curves separated by condition revealed some interesting findings. For the all variables (i.e., self-forgiveness, drinking refusal self-efficacy, guilt, and shame), participants in the intervention condition showed a similar pattern in which they improved from T1 to T2, and maintained their improvement at T3 (for shame, participants in the intervention condition continued to show positive gains even after the intervention). Participants in the TAU condition, on the other hand, either had no change or got worse from T1 to T2 on measures of self-forgiveness, guilt and shame. The decrease in self-forgiveness (and increase in guilt and shame) is somewhat puzzling. It may be that as a part of standard alcohol treatment, participants are required to take responsibility for their actions while under the influence of alcohol which may result in the formation of negative self-evaluations – including decreased levels of self-forgiveness and increased levels of guilt and shame. If this is true, a major benefit of the intervention would be that participants in the intervention received the same treatment but did not experience the same negative self-appraisals as did those in the TAU. For drinking refusal self-efficacy, participants in the TAU condition reported a small improvement from T1 to T2 as might be expected from a standard addictions protocol.
The results of the current study support findings by Webb and his colleagues (2006), who reported a relationship between alcohol use variables and self-forgiveness. Specifically, Webb and his colleagues found that even after participants ceased using alcohol, negative consequences associated with drinking left notable need for both self-forgiveness and forgiveness by others. That is, Webb et al. found that forgiveness (both of self and other) was found to have beneficial effects on participants entering substance abuse treatment protocols. Webb et al. found that forgiveness was related to several alcohol related variables. They theorized that promoting forgiveness (both self and other) would reduce an individual’s need to use or misuse alcohol. The cross-sectional nature of Webb et al.’s research, however, only allowed for theorizing that self-forgiveness would promote salutary relationships with alcohol and its use. The current research supported prior findings but used an experimental intervention, permitting tentative causal inferences.
The findings of the current study are also congruent with theorizing by Worthington et al. (2006) that the introduction of a forgiveness component may decrease feelings of guilt and shame and thereby reduce probability of relapse and using alcohol as a coping mechanism. Worthington and his colleagues note the risk factors associated with the development of unforgiving emotions. Though Worthington et al. were primarily addressing forgiveness of others, his theorizing can be applied to forgiveness of the self. The formulation of self-unforgiveness (which may be manifested in guilt and shame) may lead to using alcohol as a means to cope. Within this theoretical framework, it seems logical that introducing a self-forgiveness intervention to reduce guilt and shame would reduce the need to cope with those feelings by drinking. In the current study, participants reported significantly lower levels of guilt and shame over an alcohol-related transgression following the intervention.
Limitations of the Current Study
One limitation of the current study is the rate of attrition witnessed in the TAU condition. This differential dropout is problematic because the participants who dropped out of the study may have been systematically different than the participants who remained in the study. For example, if participants who dropped out of the study reported more positive outcomes than participants who remained in the study, this would have made it more likely for participants in the intervention condition to report greater improvement than participants in the TAU condition. Although this is a possible confound to our results, we believe that it is more likely for this differential attrition to actually work against support of the hypotheses by systematically retaining participants in the TAU condition who were likely to be more internally motivated and thus were more likely to benefit by treatment as usual without the benefit of the intervention. Further, we speculate that the strong attrition for the TAU condition may be a product of impatience in a population that is often impulsive (Fox, Hong, & Sinha, 2008; Li, Luo, Yan, Bergquist, & Sinha, 2009) and has shown a resistance to self-control (Neal & Carey, 2007; Shamloo & Cox, 2010)—at least in their inability to control alcohol use.
A second limitation of the current study is lack of diversity in the participants, which may limit the generalizability of the current study. In the current study, the community mental health centers were located in rural Michigan, in which the population is overwhelmingly European American. Obviously, alcohol use and the guilt and shame associated with it are not unique to this population. Further studies are needed with more diverse samples. For example, in some communities, substance use may be more taboo and bring with it greater levels of shame and guilt for its use. These communities, then, may experience deeper levels of shame than would the current population and react to a self-forgiveness intervention differently. Alternately, more collectivistic cultures may respond primarily to forgiveness from others rather than seeking forgiveness within themselves. With such a population, it might stand to reason that a self-forgiveness intervention may be less beneficial than an intervention promoting seeking forgiveness from others. Further research should examine nuances between populations in regards to achieving self-forgiveness for drinking related transgressions.
Furthermore, the current study did not examine exactly where participants’ lack of self-forgiveness originates. That is, it is conceivable that an individual might feel guilt and shame over his or her behaviors while under the influence of substances (as is theorized in the current study). It is also possible that an individual may feel guilt or shame simply for being caught by police for drinking rather than for wrongdoing under the influence or for the alcohol misuse itself. Because the current study deals with court-mandated treatment, this is a likely premise. That is, the majority of participants in the current study were mandated by the judicial system. Though this is extremely common in addiction treatment in community settings, it may nonetheless impact feelings of guilt and shame. An individual’s feelings of guilt and shame may also be compounded by legal problems. That is, though they feel guilt or shame for a transgression, the feelings may be exacerbated by legal complications thereby making the feelings more difficult to cope with. It was not examined in the current research how guilt or shame about getting caught may differ from guilt or shame about misusing alcohol. These are valid questions that require further study.
Another area in which the current study could have been improved is the measurement of actual alcohol use. Self-report of alcohol use in the current study was appropriate as it allows for more robust information for a greater duration and has been established as a reliable and valid method of describing substance use (Darke, 1998). Further, participants did not report the amount of alcohol presently consumed. A condition of treatment in the typical protocol was sobriety. Thus, we assumed that alcohol intake was non-existent (or that its effects could at least be controlled through random assignment) and hence we deemed it unnecessary to gather these data. The study, however, could have been strengthened by including such a measure to (a) gauge whether participants were actually abstaining from drinking, and (b) aid in the follow-up analyses. It would have been ideal to gauge whether participants did maintain sobriety or avoid risky drinking behaviors as a result of coping with feelings of guilt and shame. Though the current study examined only drinking refusal self-efficacy, and not drinking behaviors, the correlation with drinking self-efficacy and abstinence is well established in the literature (Forys, McKellar, & Moos, 2007; Litt, Kadden, Kabela-Cormier, & Petry, 2009; Oei, Fergusson, & Lee, 1998; Oei & Jardim, 2007; Young, Knight, & Oei, 1990).
Finally, it is not uncommon for individuals who misuse alcohol to be polysubstance users (Staines, Magura, Foote, Deluca & Kosanke, 2001). Hence, the cessation or reduction of alcohol misuse may be but one part in the long road to cessation of overall substance misuse. Indeed, it may even be meaningless to reduce alcohol use if it means that the individual simply substitutes another substance in its place. It may be a limitation of the current study that polysubstance use was not monitored within the participant pool. It is feasible that even as participants reported greater drinking refusal self-efficacy they may be substituting another substance in place of alcohol. This was not assessed in the current research and is an area where further study is warranted.
Of note, the current study theorizes that the reduction of guilt and shame would reduce the need to cope with transgressions by drinking. However, this relationship need not be limited to alcohol alone. That is, it is also feasible that an individual uses benzodiazepines, barbiturates, or any number of other substances in an attempt to cope with those feelings of guilt and shame. In such a case, it is possible that a similar intervention only slightly tailored to a different substance would be as effective. This is an area that would warrant further study.
Implications for Research
There are several important implications for future research. First, the study should be replicated with participants from different cultural backgrounds. Second, a measure could be created that specifically links desire to drink with feelings of guilt and shame. A future study could specifically address how the participants’ feelings about their drinking-related transgressions influence their desire to drink. Third, these findings should be replicated with different types of drug problems. Though a similar relationship could be hypothesized between any substance misuse and guilt and shame over a use-related transgression, the socially acceptable nature of alcohol may make this relationship unique. That is, it could be that a transgression would be worsened if the transgressor was misusing an illegal substance due to the even greater negative associations made with using illicit substances. The effects of introducing a similar intervention with such a dynamic warrants further investigation.
Similarly, the key to this or any intervention is whether it results in an increase in desired behaviors or decrease in undesired behaviors over an extended period of time. That is, in the case of the current study, the value of the intervention is determined by whether it results in a greater likelihood of recovery or abstinence from alcohol misuse for a greater duration. Though this study has found this in the short-term, it would be wise to examine this for an extended period of time. Therefore, it would be advantageous to replicate this study and lengthen the follow-up.
Implications for Clinical Practice
The results of the current study indicated that the inclusion of a self-forgiveness component to a traditional alcohol and drug treatment protocol increased gains in both self-forgiveness and drinking refusal self-efficacy. Because drinking refusal self-efficacy has been found to be a major predictor of abstinence or reduction in risky drinking behaviors (Forcehimes & Tonigan, 2008), incorporating a self-forgiveness intervention in existing alcohol and drug treatment protocols may be beneficial in optimizing an individual’s ability to refrain or limit his or her drinking.
Furthermore, because guilt and shame create stress for an individual (Worthington et al., 2006) and because forgiveness has been conceptualized as an emotion-focused coping strategy (Worthington & Scherer, 2004), an intervention such as the one in the current study would be a useful tool to develop positive coping strategies with clients who are dealing with guilt and shame over any transgression. Though the intervention was geared toward alcohol use in this study, it need not be limited to that type of transgression.
Conclusion
Alcohol use is a maladaptive coping strategy (Tapert, Ozyurt, & Myers, 2004; Young & Oei, 1993) and an individual may choose to engage in alcohol misuse to deal with guilt or shame (Ianni et al., 2010; Worthington et al. 2006; Webb et al., 2006). Though there are many potential ways to deal with feelings of guilt and shame, self-forgiveness is one such strategy (Hall & Fincham, 2005). Self-forgiveness is an area that has seldom been considered – and even more rarely explored – as a way to augment existing addiction treatment protocols with the idea of minimizing an individual’s need to rely on alcohol as a coping strategy and maximize efforts to prevent relapse into misuse. The addition of the self-forgiveness intervention in the current study to a traditional addictions treatment protocol promoted not only self-forgiveness and drinking refusal self-efficacy, but also reduced feelings of guilt and shame associated with alcohol use. The current study represents a major step forward in developing and applying a self-forgiveness intervention protocol to populations who misuse or abuse alcohol. Specifically, it adds support to the growing literature suggesting that forgiveness interventions help promote and maintain decreased alcohol misuse and abstinence.
Acknowledgments
The current research was supported by NIDA T32DA007292.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: American Psychiatric Association; 1994. [Google Scholar]
- Baldwin KM, Balwin JR, Ewald T. The relationship among shame, guilt, and self-efficacy. Am J of Psychother. 2006;60:1–21. doi: 10.1176/appi.psychotherapy.2006.60.1.1. [DOI] [PubMed] [Google Scholar]
- Birky IT. Evidence-based and empirically supported college counseling center treatment of alcohol related issues. J College Stud Psychother. 2005;20:7–21. [Google Scholar]
- Campbell DT, Stanley JC. Experimental and quasi-experimental designs for research. Chicago, IL: Rand McNally; 1966. [Google Scholar]
- Collins RL, Morsheimer ET, Shiffman S, Paty JA. The morning after: Limit violations and the self-regulation of alcohol consumption. Psychol Addict Behav. 2005;19:253–262. doi: 10.1037/0893-164X.19.3.253. [DOI] [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: A review. Drug Alcohol Depend. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Dearing RL, Stuewig J, Tangney JP. On the importance of distinguishing shame from guilt: Relations to problematic alcohol and drug use. Addict Behav. 2005;30:1392–1404. doi: 10.1016/j.addbeh.2005.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dongier M. What are the treatment options for comorbid alcohol abuse and depressive disorders? J Psychiatry Neurosci. 2005;30:224. [PMC free article] [PubMed] [Google Scholar]
- Edwards G, Unnithan S. Alcohol misuse. In: Stevens S, Raftery J, editors. Health care needs assessment: Volume 2. Oxford: Radcliffe Medical; 1999. pp. 341–374. [Google Scholar]
- Enright RD, Fitzgibbons RP. Helping clients forgive: An empirical guide for resolving anger and restoring hope. Washington, DC: American Psychological Association; 2000. [Google Scholar]
- Fisher ML, Exline JJ. Self-forgiveness versus excusing: The roles of remorse, effort, and acceptance of responsibility. Self Identity. 2006;5:127–146. [Google Scholar]
- Forcehimes AA, Tonigan JS. Self-efficacy as a factor in abstinence from alcohol/other drug abuse: A meta-analysis. Alcohol Treat Q. 2008;26:480–489. [Google Scholar]
- Forys K, McKellar J, Moos R. Participation in specific treatment components predicts alcohol-specific and general coping skills. Addict Behav. 2007;32:1669–1680. doi: 10.1016/j.addbeh.2006.11.023. [DOI] [PubMed] [Google Scholar]
- Fox HC, Hong KA, Sinha R. Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addict Behav. 2008;33:388–394. doi: 10.1016/j.addbeh.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Grüsser SM, Mörsen CP, Flor H. Alcohol craving in problem and occasional alcohol drinkers. Alcohol Alcohol. 2006;41:421–425. doi: 10.1093/alcalc/agl035. [DOI] [PubMed] [Google Scholar]
- Hall JH, Fincham FD. Self-forgiveness: The stepchild of forgiveness research. J Soc Clin Psychol. 2005;24:621–637. [Google Scholar]
- Harder DW, Greenwald DF. Further validation of the shame and guilt scales of the Harder Personal Feelings Questionnaire-2. Psychol Rep. 1999;85:271–281. doi: 10.2466/pr0.1999.85.1.271. [DOI] [PubMed] [Google Scholar]
- Harder DW, Lewis SJ. In: The assessment of shame and guilt. Spielberger CD, Harder DW, Lewis SJ, editors. Hillsdale: Erlbaum; 1987. pp. 89–114. [Google Scholar]
- Harris RS, Jr, Aldea MA, Kirkley DE. A motivational interviewing and common factors approach to change in working with alcohol use and abuse in college students. Prof Psychol: Res Prac. 2006;37:614–621. [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, et al. Drinking to cope, emotional distress and alcohol use and abuse: A ten-year model. J Stud Alcohol. 2001;62:190–198. doi: 10.15288/jsa.2001.62.190. [DOI] [PubMed] [Google Scholar]
- Ianni PA, Hart KE, Hibbard S, et al. The association between self-forgiveness and alcohol misuse depends on the severity of drinker’s shame: Toward a buffering model. Addict Disord Their Treat. 2010;9:106–111. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the Future national survey results on drug use, 1975–2008, Volume I. Secondary school students. Bethesda, MD: National Institute on Drug Abuse; 2009. (NIH Publication No. 09-7402) [Google Scholar]
- Li CS, Lou X, Yan P, et al. Altered impulse control in alcohol dependence: Neural measures of stop signal performance. Alcohol: Clin Exper Res. 2009;33:740–750. doi: 10.1111/j.1530-0277.2008.00891.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T, Hewitt BG, Grant BF. Alcohol use disorders and mood disorders: A National Institute on Alcohol Abuse and Alcoholism perspective. Biol Psychiatry. 2004;56:718–720. doi: 10.1016/j.biopsych.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Lin W, Mack D, Enright RD, et al. Effects of forgiveness therapy on anger, mood, and vulnerability to substance use among inpatient substance-dependent clients. J Consult Clin Psychol. 2005;72:1114–1121. doi: 10.1037/0022-006X.72.6.1114. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, et al. Changing network support for drinking: Network Support Project 2-year follow-up. J Consult Clin Psychol. 2009;77:229–242. doi: 10.1037/a0015252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Cimini MD, Barr AR, et al. Implementing a screening and brief intervention for high-risk drinking in university-based health and mental health care settings: Reductions in alcohol use and correlates of success. Addict Behav. 2007;32:2563–2572. doi: 10.1016/j.addbeh.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Martens MP, Martin JL, Hatchett ES, et al. Protective behavioral strategies and the relationship between depressive symptoms and alcohol-related negative consequences among college students. J Couns Psych. 2008;55:535–541. doi: 10.1037/a0013588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford; 2002. [Google Scholar]
- Mojtabai R, Singh P. Implications of co-occurring alcohol abuse for role impairment, health problems, treatment seeking, and early course of alcohol dependence. Am J Addict. 2007;16:300–309. doi: 10.1080/10550490701389815. [DOI] [PubMed] [Google Scholar]
- Neal DJ, Carey KB. The association between alcohol intoxication and alcohol-related problems: An event-level analysis. Psych Addict Behav. 2007;21:194–204. doi: 10.1037/0893-164X.21.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oei TPS, Fergusson S, Lee N. The differential role of alcohol expectancies and drinking refusal self-efficacy in problem and non-problem drinkers. J Stud Alcohol. 1998;59:704–711. doi: 10.15288/jsa.1998.59.704. [DOI] [PubMed] [Google Scholar]
- Oei TPS, Hasking PA, Young RM. Drinking refusal self-efficacy questionnaire-revised (DRSEQ-R): A new factor structure with confirmatory factor analysis. Drug Alcohol Depend. 2005;78:297–307. doi: 10.1016/j.drugalcdep.2004.11.010. [DOI] [PubMed] [Google Scholar]
- Oei TPS, Jardim CL. Alcohol expectancies, drinking refusal self-efficacy and drinking behavior in Asian and Australian students. Drug and Alcohol Depend. 2007;87:281–287. doi: 10.1016/j.drugalcdep.2006.08.019. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Saunders SM, Zygowicz KM, D’Angelo BR. Person-related and treatment-related barriers to alcohol treatment. J Subst Abuse Treat. 2006;30:261–270. doi: 10.1016/j.jsat.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Scheier LM, Botvin GD, Diaz T. Social skills, competence, and drug refusal self-efficacy as predictors of adolescent alcohol use. J Drug Educ. 1999;29:251–278. doi: 10.2190/M3CT-WWJM-5JAQ-WP15. [DOI] [PubMed] [Google Scholar]
- Scherer M, Worthington EL, Jr, Hook JN, et al. Forgiveness and familial cohesion in college students’ perceptions of families with alcohol misuse. 2011 Manuscript submitted for publication. [Google Scholar]
- Scholl MB, Schmitt DM. Using motivational interviewing to address college client alcohol abuse. J College Couns. 2009;12:57–70. [Google Scholar]
- Shamloo ZS, Cox WM. The relationship between motivational structure, sense of control, intrinsic motivation and university students’ alcohol consumption. Addict Behav. 2010;35:140–146. doi: 10.1016/j.addbeh.2009.09.021. [DOI] [PubMed] [Google Scholar]
- Shields AL, Hufford MR. Assessing motivation to change among problem drinkers with and without co-occurring major depression. J Psychoactive Drug. 2005;37:401–408. doi: 10.1080/02791072.2005.10399813. [DOI] [PubMed] [Google Scholar]
- Snyder CR, Heinze LS. Forgiveness as a mediator of the relationship between PTSD and hostility in survivors of childhood abuse. Cogn Emot. 2005;19:413–431. doi: 10.1080/02699930441000175. [DOI] [PubMed] [Google Scholar]
- Staines GL, Magura S, Foote J, Deluca A, Kosanke N. Polysubstance use among alcoholics. J Addict Dis. 2001;20:53–69. doi: 10.1300/j069v20n04_06. [DOI] [PubMed] [Google Scholar]
- Strelan P. The prosocial, adaptive qualities of just world beliefs: Implications for the relationship between justice and forgiveness. Pers Individ Dif. 2007;43:881–890. [Google Scholar]
- Tangney JP, Dearing RL. Shame and guilt. New York: Guilford; 2002. [Google Scholar]
- Tapert SF, Ozyurt SS, Myers MD. Neurocognitive ability in adults coping with alcohol and drug relapse temptations. Am J Drug Alcohol Abuse. 2004;30:445–460. doi: 10.1081/ada-120037387. [DOI] [PubMed] [Google Scholar]
- Webb JR, Trautman RP. Forgiveness and alcohol use: Applying a specific spiritual principle to substance abuse problems. Addict Disord Their Treat. 2010;9:8–17. [Google Scholar]
- Webb JR, Robinson EAR, Brower KJ. Forgiveness and mental health among people entering outpatient treatment with alcohol problems. Alcohol Treat Q. 2009;27:368–388. [Google Scholar]
- Webb JR, Robinson EAR, Brower KJ, et al. Forgiveness and alcohol problems among people entering substance abuse treatment. J Addict Dis. 2006;25:55–67. doi: 10.1300/J069v25n03_08. [DOI] [PubMed] [Google Scholar]
- Wohl MJA, DeShea L, Wahkinney RL. Looking within: Measuring state self-forgiveness and its relationship to psychological well-being. Canadian J of Beh Sci. 2008;40:1–10. [Google Scholar]
- Woien SL, Ernst HAH, Patock-Peckham JA, et al. Validation of the TOSCA to measure shame and guilt. Pers Individ Diff. 2003;35:313–326. [Google Scholar]
- Worthington EL., Jr . Forgiveness and reconciliation: Theory and application. New York: Brunner-Routledge; 2006. [Google Scholar]
- Worthington EL, Jr, Scherer M. Forgiveness is an emotion-focused coping strategy that can reduce health risks and promote health resilience: Theory, review, and hypotheses. Psychol Health. 2004;19:385–405. [Google Scholar]
- Worthington EL, Jr, Scherer M, Cooke KL. Forgiveness in alcohol dependence, abuse, and their treatment. Alcohol Treat Q. 2006;24:125–145. [Google Scholar]
- Yelsma P, Brown NM, Elison J. Shame-focused coping styles and their association with self-esteem. Psychol Rep. 2002;90:1179–1189. doi: 10.2466/pr0.2002.90.3c.1179. [DOI] [PubMed] [Google Scholar]
- Young RM, Oei TP. Grape expectations: The role of alcohol expectancies in the understanding and treatment of problem drinking. Int J Psychol. 1993;28:337–364. [Google Scholar]
- Young RM, Knight R, Oei TPS. The stability of alcohol-related expectancies in social drinking situations. Australian J Psychol. 1990;42:321–330. [Google Scholar]