Abstract
Research has not consistently supported an association between stage of change and substance abuse treatment retention. The current study examined whether social desirability response bias could help explain why. Participants (N=200), recruited from an outpatient program, completed the URICA, TREAT, Marlowe-Crowne Social Desirability Scale (MC-SDS), and other measures. Number of treatment groups attended was collected from program records. In bivariate analyses, neither the URICA nor the TREAT was related to attendance. However, higher social desirability was strongly associated with lower URICA (but not TREAT) total scores, and in a multivariate path model, a moderately strong association emerged between higher URICA scores and greater treatment attendance when accounting for social desirability. Higher social desirability was also an independent predictor of greater treatment attendance, and was strongly associated with lower ASI Alcohol, Drug, and Psychiatric severity. Results underline a critical problem in measuring motivation and problem severity that has been largely neglected.
1. Introduction
Treatment motivation is a critical limiting factor in the delivery of substance abuse treatment, and has received substantial research attention. Nevertheless, to date, the dominant measures of treatment motivation—that is, the stage of change scales—have proven to be surprisingly poor predictors of retention. The current study examines whether socially desirable responding might be responsible for attenuating relationships between existing stage of change scales and treatment retention, focusing on the URICA (University of Rhode Island Change Assessment Scale; McConnaughy, DiClemente, Prochaska, & Velicer, 1989) and TREAT (Treatment Readiness Tool; Freyer et al., 2004). I begin by reviewing the research on stage of change scales and social desirability.
1.1. Stage of Change Scales and Treatment Retention
In the 1980’s, a number of new models and scales of treatment motivation began to surface, all premised on the assumption that individuals progress through distinct stages in their motivation to change and theoretically grounded, in large part, in the transtheoretical model (TTM) of change (DiClemente &Prochaska, 1998; Prochaska & Norcross, 2001). Some of the scales, collectively known as “stage of change” scales, have become very well-recognized, including the URICA (University of Rhode Island Change Assessment Scale; McConnaughy, et al., 1989), SOCRATES (Stages of Change Readiness and Treatment Eagerness Scale; Miller &Tonigan, 1996), RTCQ (Readiness to Change Questionnaire; Rollnick, Heather, Gold, & Hall, 1992), and TREAT (Treatment Readiness Tool; Freyer, et al., 2004). Empirical work on these scales has helped to identify some important influences on the motivation to seek help, and has helped spur research on motivational interviewing, an intervention with efficacy comparable to other evidence-based treatments even in small doses (Carey, Scott-Sheldon, Carey, & De Martini, 2007; Deas, 2008; Lundahl & Burke, 2009; Vasilaki, Hosier, & Cox, 2006). Despite these successes, however, research indicates weak and inconsistent associations between stage of change scales and treatment retention.
While select studies have found that stage of change scales do predict treatment seeking and retention, and that matching intervention to stage of change can improve outcomes (DiClemente & Prochaska, 1998; Prochaska & Norcross, 2001), many studies have produced null and contrary results (e.g., Aveyard et al., 1999; Crane et al., 1998; Farkas et al., 1996; Greene & Rossi, 1998; Lancaster et al., 1999; Naylor, Simmonds, Riddoch, Velleman, & Turton, 1999; Project MATCH Research Group, 1997; Steptoe et al., 1999; Whitelaw, Baldwin, Bunton, & Flynn, 2000). Pantalon and Swanson (2003) recently found, for example, that participants scoring lower on the URICA showed greater (not less) treatment adherence than high scorers, attending more therapeutic groups while hospitalized and more clinic appointments during their first month post-discharge. Reviewers of research on the stage of change/TTM model have thus expressed serious concerns over both the findings and the methodological limitations associated with that work (Ashworth, 1997; Bandura, 1998; Davidson, 1998; Migneault, Adams, & Read, 2005; Sutton, 1996b; Whitelaw, et al., 2000).
It is not yet clear why the results for stage of change scales have been so disappointing. Critics have often focused on perceived weakness in the premise of distinct stages of motivational readiness (Bandura, 1998; Davidson, 1998; Sutton, 1996b). Indeed, the purported stage structure of motivation has been largely contradicted by the evidence (Davidson, 1992; Davidson, 1998; Littell & Girvin, 2002; Sutton, 1996a).1 This suggests that item wording of associated scales (which is explicitly tailored to “stage”) is inappropriate, and that allocating individuals to stages needlessly sacrifices variability in motivation. Application of the stage of change scales to treatment retention per se is also inconsistent with the principle of compatibility (Ajzen & Fishbein, 1977; Fishbein & Ajzen, 1975), which suggests that an attitude will be predictive of behavior only to the extent that both constructs are measured at compatible levels of specificity. Because stage of change scales typically focus on global attitudes toward change rather than attitudes toward completing treatment in a given timeframe at a given program, it makes sense that the scales are poor predictors of that specific behavior (Zemore, Ajzen, & O’Hearn, 2011).
One additional possibility, though, is that self-presentational biases, and particularly the motivation to respond in a socially desirable manner, have muddied associations between stage of change scales and treatment retention. If so, then accounting for the distortions caused by socially desirable responding could strengthen associations between self-reported stage of change and treatment retention.
1.2. Social Desirability
Social desirability is an important, yet often neglected, issue in drug and alcohol research. Social desirability, or “faking good,” is an individual difference variable and response bias reflecting the need to “obtain approval by responding in a culturally appropriate and acceptable manner” (Crowne &Marlowe, 1960, p. 350). Although social desirability has received little attention in the alcohol field, a few studies have shown that social desirability affects responses to alcohol and drug consumption and harms questions considerably. For example, a large general population survey found that higher social desirability, measured using the Marlowe-Crown Social Desirability Scale (MC-SDS; Crowne & Marlowe, 1960), was a moderately strong predictor of lower self-reported alcohol and drug use (Welte & Russell, 1993). Another study, again using general population data, found that higher social desirability predicted substantially lower odds of self-reported a) driving after drinking and b) risky driving style generally (Schell, Chan, & Morral, 2006). Mirroring these results, two parallel studies on undergraduate drinkers (Davis, Thake, & Vilhena, 2010) found that those high on impression management, a related construct, reported 20-30% less consumption and were about 50% less likely to report risky drinking than low impression managers. The second study (same article) also found that high impression managers reported 30-50% fewer acute harms following a drinking episode, and that effects maintained even after controlling for trait impulsivity/constraint.
Social desirability may also affect how individuals answer questions on motivation to change, although it is hard to predict prima facie how. On the one hand, pressures from treatment providers could cause people high on social desirability to exaggerate their willingness to change. On the other, stigma associated with alcohol and drug addiction could cause this same group to diminish their problems. Both effects could also obtain simultaneously: Among those high on social desirability, one subset may exaggerate their motivation to change, while another may seek approval by diminishing it. Further, the effects of social desirability could depend on both the scale characteristics and context of administration: Some items and contexts (e.g., face-to-face vs. computerized interviews) may be especially like to elicit biased responding. Whatever the case, to the extent that social desirability distorts measurement of motivation to change, it could dampen or alter the observed relationships between stage of change scales and treatment attendance.
A related issue is that social desirability could itself directly impact treatment retention. Theoretically, a desire for social approval could either contribute to or undermine treatment retention, depending on whether attendance is seen by the client as socially desirable, neutral, or stigmatizing. Again, there is almost no work on this question. In an exception, one (dated) study, sampling 62 male alcoholics, found that individuals completing a 6-week hospital program scored higher on the MC-SDS than individuals who terminated prematurely (Krasnoff, 1976). This finding is important because an association between social desirability and treatment retention could further complicate the relationship between stage of change and treatment retention.
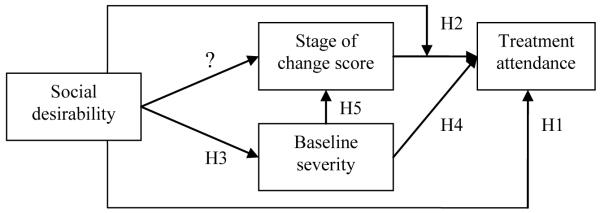
The purpose of the current study was to address, in a standard outpatient treatment sample, the impact of social desirability on a) responses to two popular stage of change scales, the URICA and TREAT, b) treatment attendance per se, and c) associations between treatment attendance and our stage of change scales. A secondary goal was to examine associations between social desirability and measures of alcohol, drug, and psychiatric severity at baseline. Based on the lack of preliminary data, we did not have expectations for how social desirability would relate to stage of change scales. However, we did hypothesize that higher social desirability would be associated with greater treatment attendance (H1), and that relationships between stage of change and treatment retention would be stronger among those low (vs. high) on social desirability (H2). We also expected negative associations between social desirability and problem severity (H3), and, consistent with the literature, that higher severity on at least some subscales would predict lower treatment attendance (H4) but higher stage of change (H5).2 Figure 1 depicts these expectations.
Figure 1.
Conceptual model.
Establishing that a response bias affects associations between stage of change scales and retention would seem to have little immediate relevance to providers, since it is not yet obvious how this information could be used to enhance identification of likely dropouts. However, understanding how response biases affect the measurement of motivation to change, problem severity, and other key constructs in addictions research is critical to understanding all relationships involving those constructs, and hence, to our understanding of addiction. Describing those response biases and their effects is thus a worthy goal.
2. Materials and Methods
2.1. Study Site and Recruitment
Baseline data from 200 participants were collected between August 2009 and August 2010 at two sister sites (N’s=134 and 66 respectively) operated by a large, public, outpatient alcohol and drug treatment program in California. All study procedures were approved by the ethical review board of the Public Health Institute. The study program offers substance abuse services to adults and special populations including adolescents and individuals legally mandated to treatment. Clients are referred from residential programs, insurance companies, Children and Family Services (CFS), and probation officers. Most (90%) of the outpatient treatment is funded by Contra Costa County. Expected treatment duration is typically 8-12 weeks in length, and includes two 90-minute group sessions per week; however, clients also attend an educational group offered once-weekly while waiting for a treatment slot to open. The curriculum addresses the individual in the context of family and social relationships, and incorporates an emphasis on the 12-step approach. Clients are encouraged to attend weekly continuing care groups for a minimum of one year post-discharge. All counselors have a master’s-level degree, doctoral-level degree, or a license in addiction counseling, and about 86% are in recovery. Clients must have a primary diagnosis of chemical dependency or substance abuse to be admitted.
Eligible participants for the current study included all males and females aged 18 and over presenting for intake at the regular adult outpatient program during baseline recruitment. Participants were required to speak English fluently. The program screens all clients and accepts only those without incapacitating mental or physical health problems, consistent with ASAM’s patient placement criteria for outpatient services level of care I (Mee-Lee, Shulman, Fishman, Gastfriend, & Griffith, 2001). Individuals mandated to the program via Proposition 36 were excluded from the study. Proposition 36 clients are nonviolent, simple drug possession offenders mandated to treatment instead of incarceration, and they receive treatment in a separate track.
Interviewers introduced the study to clients attending their first or second education group and prior to entering formal treatment. Clients were informed that the study aimed to examine clients’ opinions about treatment, and that their participation would involve one in-person interview (lasting 40-60 minutes) and a potential telephone follow-up, not relevant here. Interested clients were escorted to the experimental room, onsite, and completed consent procedures. Interviews were then administered using audio computer-assisted self interviews (ACASI), which have been found to yield more accurate reports for sensitive data than traditional in-person interviews and self-administered surveys (Lessler & O’Reilly, 1997; O’Reilly, Hubbard, Lessler, Biemer, & Turner, 1994). Participants received $50 gift certificates. Among those approached, 91% consented, and there were no significant differences between those who refused and those who consented on gender, age, or race, although there were more refusers at the smaller than the larger site, given the distribution of eligible clients (p<.01).
2.2. Measures
2.2.1. Stage of change scales
Measures included two stage of change scales: the University of Rhode Island Change Assessment Scale (URICA; McConnaughy, et al., 1989), designed to measure general readiness to change, and the Treatment Readiness Tool (TREAT; Freyer, et al., 2004), assessing readiness to seek help for an alcohol and/or drug problem specifically. The URICA is a 32-item scale measuring 4 purported stages with 8 items each; the TREAT, at 15 items, assesses 5 stages using 3 items each. To create a total score for the URICA, we reverse-coded the Precontemplation items and averaged. This scoring is consistent with Project MATCH’s approach (DiClemente, Carbonari, Zweben, Morrel, & Lee, 2001; Project MATCH Research Group, 1997) and reflects the fact that research has not reliably supported the supposed stage structure underlying any stage of change scale (Bandura, 1998; Davidson, 1998; Sutton, 1996b). The total score was transformed using a reflect-and-square-root transformation (Tabachnick & Fidell, 1989). We used a more experimental approach for the TREAT, reverse-coding the Precontemplation and Contemplation items and summing with the Preparation items to reflect the favorability of one’s attitude toward treatment, excluding the Action and Maintanence subscales. This decision was based on both conceptual and empirical grounds. The Action and Maintenance subscales measure a) the ambivalent acceptance of help in the short-term and b) acceptance of help for more than a year, respectively, which are behaviors that are conceptually distinct from, and hence not scalable with, one’s overall attitude toward treatment. Further, incorporating the full set of items seriously reduced the scale’s internal reliability.3 Cronbach’s alpha’s were good to excellent for the URICA subscales (α’s=.82-.88) and total scale (α=.93) and poor to excellent for the TREAT subscales (α’s=.62-.90) and total scale (α=.81).
To accommodate a lengthy survey, the URICA and TREAT were balloted: Half the participants completed the URICA, and half completed the TREAT. No other relevant surveys were balloted. Participants completing the URICA were equivalent to those completing the TREAT on all demographic variables, clinical variables, and treatment attendance (all p’s>.17).
2.2.2. Social desirability
We used Ballard’s 11-item short form (Ballard, 1992) of the Marlowe-Crowne Social Desirability Scale (MC-SDS; (Crowne &Marlowe, 1960). Items on the MC-SDS, all true-false, tap endorsement of “behaviors which are culturally sanctioned and approved but which are improbable” (Crowne & Marlowe, 1960, p. 350). Responses are recoded so that 1 is high and 0 is low on social desirability, and summed. Sample items are “No matter who I’m talking to, I’m always a good listener,” (true=1) and “There have been occasions when I took advantage of someone” (false=1). Ballard’s scale was developed based on factor analyses of the full MC-SDS scale and has been identified as the best among the short forms (Loo & Loewen, 2004; see also Reynolds, 1982). In the current study, internal reliability was good (α=.74); scale M=5.55, SD=2.75. The current mean was slightly higher than that obtained in studies of undergraduates (e.g., M=4.68 in Ballard, 1992; M=4.99 in Loo & Loewen, 2004). This may suggest that our sample was “defensively high” on social desirability, but it is hard to know since the scale does not seem to have been used in comparable community samples. MC-SDS scores have been positively associated with age and negatively associated with socioeconomic status (Evans, 1982; Welte & Russell, 1993), so it seems more likely that the mean differences are attributable to the relatively older age and lower socioeconomic status of our sample (vs. undergraduates). The MC-SDS was not associated with either Legal or Employment Coercion (p’s>.45; see below).
2.2.3. Baseline problem severity
Surveys also included items from the Alcohol, Drug, and Psychiatric Severity subscales of the Addiction Severity Index (ASI; McLellan, Luborsky, Cacciola, & Griffith, 1985; McLellan, Luborsky, Woody, & O’Brien, 1980). The ASI is a structured clinical interview for the evaluation of substance abuse severity showing high reliability and validity (McLellan, et al., 1980). Alcohol and Drug subscales elicit 30-day consumption rates for alcohol and drugs in 12 different categories; alcohol- and drug-related problems; and the subjective importance of treatment. The Psychiatric subscale assesses various symptoms of psychiatric distress, such as serious depression, anxiety, confusion, and suicidal behavior, as well as the subjective importance of treatment for the same. Scores were aggregated using the standard algorithms (McLellan, et al., 1980).
2.2.4. Coercion
As a potential covariate, we included the Legal and Employment subscales of the Perceived Coercion Questionnaire (PCQ; Klag, Creed, & O’Callaghan, 2006), at 5 items each. Prior research has been supportive of the scales’ dimensional structure, internal reliability, test-retest reliability, and validity, the latter evidenced by positive associations with male gender, younger age, and illegal drug use (Klag, et al., 2006). We created total scores by averaging within subscale (Legal α=.86, Employment α=.85) and across items (α=.84).
2.2.5. Demographic and clinical variables
Additional variables included race, gender, age, marital status, education, employment status, annual household income, and number of prior alcohol or drug treatment episodes.
2.2.6. Treatment attendance
Total number of treatment groups attended was collected from program records, with participants’ written permission. Number of education groups attended was included in this variable.
2.3. Analysis
For descriptive purposes, Pearson correlations were used to examine the associations between social desirability and all items on the URICA and TREAT. We also conducted correlations between all variables of key conceptual interest, including URICA and TREAT subscales (though we did not plan to use these separately in the main analysis). These analyses helped to describe the data and identify variables for inclusion in the main analysis, such as those severity scales that were related to treatment attendance, and determine whether the URICA, the TREAT, or both should be tested. The main analysis was a path analysis, implemented in mplus (Muthén & Muthén, 2007), testing our conceptual model. Choice of control variables was determined on the basis of preliminary analyses and initial model results (see below).
Excluding participants who discontinued treatment because they were referred elsewhere or died had very little effect on the associations of interest, so these participants were retained for all analyses.
3. Results
3.1. Sample Characteristics
Table 1 displays the sample characteristics. Respondents tended to be male, single, and White, and the mean age was 35.7. The sample was very low on socioeconomic status, as indicated by the high unemployment rates, low income, and low education. Most participants reported prior treatment, and only a minority reported alcohol as their drug of choice. The most common drug of choice after alcohol was methamphetamine. (Drug of choice rates do not sum to 100% because of missing data.) A minority of participants (45%) completed treatment. Participants who attended formal treatment attended an average of 3.22 education groups (SD=2.18, range=1-9) prior to entry (not shown).
Table 1.
Sample characteristics.
| % Sample (N=200) | |
|---|---|
| GENDER | |
| Male | 70.0 |
| Female | 29.5 |
| Transgender/Intersex | 0.5 |
| AGE | |
| 18-29 | 34.0 |
| 30-39 | 24.5 |
| 40-49 | 29.0 |
| 50-59 | 9.0 |
| 60 or higher | 2.5 |
| MARITAL STATUS | |
| Married/living with sig. other | 32.0 |
| Single | 68.0 |
| ETHNICITY | |
| White/Caucasian | 62.0 |
| Latino/Hispanic | 16.0 |
| Black/African American | 13.5 |
| Other | 8.5 |
| EMPLOYMENT | |
| Employed full-time | 14.0 |
| Employed part-time/self-employed | 21.0 |
| Not employed | 65.0 |
| INCOME | |
| UNDER $10,000 | 40.0 |
| $10,001-$20,000 | 20.0 |
| $20,001-$30,000 | 14.5 |
| $30,001-$50,000 | 11.0 |
| $50,001 or higher | 12.5 |
| EDUCATION | |
| Less than high school diploma | 21.0 |
| High school diploma or equivalent | 37.5 |
| Some college or higher | 41.5 |
| PRIOR TX EPISODES | |
| 0 | 39.0 |
| 1-2 | 37.5 |
| 3 or more | 22.5 |
| DRUG OF CHOICE | |
| Alcohol only | 29.5 |
| Methamphetamine only | 25.5 |
| Marijuana only | 8.0 |
| Other drug or poly-drug | 30.0 |
| TREATMENT DISCHARGE STATUS | |
| Complete | 45.0 |
| Incomplete, no referral | 33.5 |
| Incomplete, referred elsewhere | 19.0 |
| Deceased | 2.5 |
3.2. Associations between Social Desirability and Stage of Change Scales
Tables 2 and 3 display correlations between the Marlowe-Crowne Social Desirability Scale (MC-SDS) and all items on the URICA and TREAT arranged (within subscale) in order of size. These tables show considerable variation in associations between the MC-SDS and items assessing stage of change.
Table 2.
Correlations (Pearson r’s) between URICA items and scores on the Marlowe-Crowne Social Desirability Scale (MC-SDS). 1
| PRECONTEMPLATION SCALE | |
| Being here is pretty much a waste of time for me because the problem doesn’t have to do with me. | .38*** |
| As far as I’m concerned, I don’t have any problems that need changing. | .33*** |
| I’m not the problem one. It doesn’t make much sense for me to be here. | .28** |
| I guess I have faults, but there’s nothing that I really need to change. | .24* |
| I may be part of the problem, but I don’t really think I am. | .19+ |
| I would rather cope with my faults than try to change them. | .09 |
| All this talk about psychology is boring. Why can’t people just forget about their problems? | .06 |
| I have worries but so does the next guy. Why spend time thinking about them? | .02 |
| CONTEMPLATION SCALE | |
| I think I might be ready for some self-improvement. | −.40*** |
| I wish I had more ideas on how to solve the problem. | −.38*** |
| I have a problem and I really think I should work at it. | −.37*** |
| I’ve been thinking that I might want to change something about myself. | −.37*** |
| Maybe this place will be able to help me. | −.32*** |
| It might be worthwhile to work on my problem. | −.26** |
| I’m hoping this place will help me to better understand myself. | −.24* |
| I hope that someone here will have some good advice for me. | −.14 |
| ACTION SCALE | |
| At times my problem is difficult, but I’m working on it. | −.49*** |
| I have started working on my problems but I would like help. | −.39*** |
| Even though I’m not always successful in changing, I am at least working on my problem. | −.29** |
| I am doing something about the problems that had been bothering me. | −.18+ |
| I am actively working on my problem. | −.17+ |
| I am finally doing some work on my problem. | −.15 |
| I am really working hard to change. | −.02 |
| Anyone can talk about changing; I’m actually doing something about it. | .01 |
| MAINTENANCE SCALE | |
| I thought once I had resolved my problem I would be free of it, but sometimes I still find myself struggling with it. | −.45*** |
| After all I had done to try to change my problem, every now and again it comes back to haunt me. | −.41*** |
| It is frustrating, but I feel I might be having a recurrence of a problem I thought I had resolved. | −.40*** |
| I may need a boost right now to help me maintain the changes I’ve already made. | −.36*** |
| I’m not following through with what I had already changed as well as I had hoped, and I’m here to prevent a relapse of the problem. |
−.36*** |
| I’m here to prevent myself from having a relapse of my problem. | −.35*** |
| It worries me that I might slip back on a problem I have already changed, so I am here to seek help. | −.34*** |
| I have been successful in working on my problem but I’m not sure I can keep up the effort on my own. | −.34*** |
p<.001
p<.01
p<.05
p<.10.
URICA and TREAT scales were given to non-overlapping samples of 100 participants.
Table 3.
Correlations (Pearson r’s) between TREAT items and scores on the Marlowe-Crowne Social Desirability Scale (MC-SDS). 1
| PRECONTEMPLATION SCALE | |
| I do not think treatment will work for me. | −.10 |
| I do not think that other people can help me. | .05 |
| It’s nobody’s business what I do with my life. | −.04 |
| CONTEMPLATION SCALE | |
| I eventually may want help, but not now. | −.19+ |
| I’m uncertain about the need for treatment. | .10 |
| Treatment may help but I’m not yet ready for it. | −.08 |
| PREPARATION SCALE | |
| I think I need help. | −.23* |
| I want to talk to somebody now about my problems. | −.13 |
| I have decided to seek appropriate treatment. | −.11 |
| ACTION SCALE | |
| I have been seeking help for a short time now, but only half-heartedly. | −.18+ |
| I have been grudgingly accepting help for a short time now. | −.08 |
| For a short time now I have been accepting help but I have not gotten used to it, yet. | .00 |
| MAINTENANCE SCALE | |
| For more than a year now seeking and accepting help has been part of my life. | .07 |
| I have been accepting help for a long time. | .04 |
| I have been accepting help for more than a year now. | .00 |
p<.05
p<.10.
URICA and TREAT scales were given to non-overlapping samples of 100 participants.
As Table 2 shows, participants high on social desirability generally strongly agreed with the URICA’s Precontemplation items and strongly disagreed with items tapping Contemplation, Action, and Maintenance. However, certain items were not at all correlated with social desirability, such as the final 1-3 items on the Precontemplation, Contemplation, and Action scales. Some Action items were also only weakly associated with social desirability.
Conversely, social desirability was not strongly associated with responses to the TREAT. None of the TREAT’s items were significantly associated with the MC-SDS, with the exception of one (“I think I need help”), which elicited disagreement from those high on social desirability. Those high on social desirability were also marginally less likely to agree with the items, “I eventually may want help, but not now,” and “I have been seeking help for a short time now, but only half-heartedly.”
3.3. Bivariate Associations involving Variables of Key Theoretical Interest
Table 4 presents bivariate associations between variables of key theoretical interest. The row and column for the MC-SDS (Marlowe-Crowne Social Desirability Scale) speak to important pathways, indicating a strong, negative association between social desirability and self-reported change readiness as measured by the URICA total score as well as all URICA subscales. The MC-SDS was not associated with the TREAT total score or subscales, except for Preparation, which showed a marginal, unexpectedly negative association with the MC-SDS. As expected, the MC-SDS was meanwhile negatively and rather strongly associated with ASI Alcohol severity (r=−.19, p<.01), Drug severity (r=−.28, p<.001), and Psychiatric severity (r=−.38, p<.001), but positively associated with treatment attendance (r=.15, p<.05). Further, and again as expected, higher ASI severity scores were generally associated with higher URICA and TREAT total scores, though associations were stronger for the URICA (vs. the TREAT), and ASI Alcohol severity was not significantly associated with the TREAT total score. Besides the MC-SDS, significant correlates of greater treatment attendance were higher ASI Drug and Psychiatric severity, as expected; not surprisingly, none of the URICA or TREAT scores were associated with attendance in these bivariate analyses, except for the TREAT’s Preparation and Action subscales (again in the direction opposite to expectations). Finally, it bears notice that the pattern of associations for neither the URICA nor the TREAT supports the purported underlying stage structure: Associations between adjacent stages were not as a rule stronger than associations between distal stages. This provides further justification for our unidimensional scoring.
Table 4.
Correlations (Pearson r’s) between key variables considered for the path modeling, including stage of change subscales for descriptive purposes.1
| URICA Total |
URICA Pre. |
URICA Con. |
URICA Action |
URICA Main. |
TREAT Total |
TREAT Pre. |
TREAT Con. |
TREAT Prep. |
TREAT Action |
Treat Main. |
MC- SDS |
ASI Alcohol |
ASI Drug |
ASI Psych. |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| URICA Total |
1.00 | ||||||||||||||
| URICA Pre. |
−.74*** 100 |
1.00 | |||||||||||||
| URICA Con. |
.91*** 100 |
−.59*** 100 |
1.00 | ||||||||||||
| URICA Action |
.88*** 100 |
−.51*** 100 |
.80*** 100 |
1.00 | |||||||||||
| URICA Main. |
.88*** 100 |
−.43*** 100 |
.81*** 100 |
.75*** 100 |
1.00 | ||||||||||
| TREAT Total |
-- | -- | -- | -- | -- | 1.00 | |||||||||
| TREAT Pre. |
-- | -- | -- | -- | -- | −.77*** 100 |
1.00 | ||||||||
| TREAT Con. |
-- | -- | -- | -- | -- | −.79*** | .44*** 100 |
1.00 | |||||||
| TREAT Prep. |
-- | -- | -- | -- | -- | .83*** | −.39*** 100 |
−.51*** 100 |
1.00 | ||||||
| TREAT Action |
-- | -- | -- | -- | -- | −.06 100 |
.08 100 |
.25* 100 |
.14 100 |
1.00 | |||||
| TREAT Main. |
-- | -- | -- | -- | -- | .16 100 |
.01 100 |
−.10 100 |
.27** 100 |
−.10 100 |
1.00 | ||||
| MC-SDS | −.46*** 100 |
.28** 100 |
−.42*** 100 |
−.34*** 100 |
−.49*** 100 |
−.06 100 |
−.03 100 |
−.04 100 |
−.19† 100 |
−.11 100 |
.04 100 |
1.00 | |||
| ASI Alcohol |
.38*** 100 |
−.31** 100 |
.33*** 100 |
.26** 100 |
.36*** 100 |
.04 100 |
.06 100 |
.06 100 |
.20* 100 |
.24* 100 |
.03 100 |
−.19** 200 |
1.00 | ||
| ASI Drug |
.35*** 100 |
−.14 100 |
.38*** 100 |
.24* 100 |
.42*** 100 |
.22* 100 |
.02 100 |
−.12 100 |
.39*** 100 |
.21* 100 |
−.03 100 |
−.28*** 200 |
.17* 200 |
1.00 | |
| ASI Psych. |
.36*** 99 |
−.14 99 |
.35*** 99 |
.25* 99 |
.44*** 99 |
.21* 100 |
.03 100 |
−.06 100 |
.44*** 100 |
.19† 100 |
.08 100 |
−.38*** 199 |
.38*** 199 |
.46*** 199 |
1.00 |
| Tx. Attend. |
.05 100 |
−.10 100 |
.07 100 |
.03 100 |
.00 100 |
−.09 100 |
−.13 100 |
.07 100 |
−.26* 100 |
−.17† 100 |
−.12 100 |
.15* 200 |
−.02 200 |
−.16* 200 |
−.21** 199 |
p<.001
p<.01
p<.05
p<.10.
URICA and TREAT scales were given to non-overlapping samples of 100 participants. MC-SDS is Marlowe-Crowne Social Desirability Scale; Pre is Precontemplation; Con is Contemplation; Prep is Preparation; Main is Maintenance; Psych is Psychiatric; Attend is Attendance.
3.4. Full Conceptual Model
Path modeling was applied in the main analysis to take account of the complex relationships among variables. Preliminary analyses indicated no evidence of a relationship between the MC-SDS and the TREAT (Table 4), and additional analyses showed that neither including MC-SDS in the model as a main effect nor interacting the TREAT with MC-SDS produced significant effects on attendance (not shown). Hence, the current analysis focused exclusively on the URICA. Similarly, ASI Alcohol severity was not included in the model because it was not associated with treatment attendance, our main outcome. The model was run using maximum likelihood estimation.
In estimating the initial model, all demographic and clinical variables that were associated with treatment attendance at p<.10 were selected for use as covariates, including race (Latino, Black, or Other, vs. White), annual household income (middle, at $10,001-$30,000, or high, at $30,001 or more, vs. low, at $10,000 or less), and parenting status (parenting a child under 18 vs. not parenting). Neither measures of coercion nor treatment site were related to treatment attendance, so these variables were omitted from the model. The initial model was refined by removing nonsignificant pathways and predictors, and by adding pathways where indicated by modification indices and where theoretically plausible. All pathways depicted in the conceptual model (Figure 1) were included in the initial model.
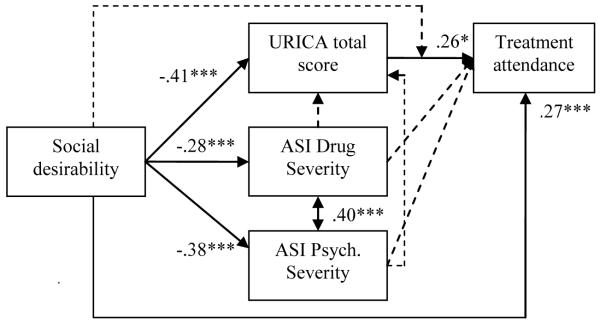
After some modifications, the final model, shown in Figure 2, achieved excellent fit (see fit statistics). Consistent with the bivariate results and H1, higher MC-SDS scores were significantly associated with both lower URICA scores and greater treatment attendance, with an especially strong effect for the former. Perhaps most important, when accounting for the impact of social desirability on treatment attendance, URICA total score became a significant, moderately strong, positive predictor of attendance. This was not an expected result and may indicate a suppressor effect, described in detail in the Discussion. The hypothesized interaction between MC-SDS score and change readiness (H2) was not significant, and was dropped from the model. The MC-SDS was also strongly and negatively associated with ASI Drug and Psychiatric severity, confirming H3. However, when the effects of social desirability on treatment attendance and stage of change were considered, there were no effects for ASI Drug or Psychiatric severity on either of these variables (violating H4 and H5). This may suggest that associations between higher severity scores and these variables were at least in part artifacts of shared associations with lower social desirability, again discussed subsequently.
Figure 2.
Multivariate path model examining the joint influence of social desirability and URICA (stage of change) total score on treatment attendance. 1
***p<.001, *p<.05.
χ2 (12, 87)=17.73, p=.12, CFI=.96, TLI=.89, RMSEA=.049 (95% CI .000-.094).
1Additional covariates, not shown, were parenting status (for treatment attendance) and race (for treatment attendance, social desirability, and URICA total score). Dashed lines represent tested, but nonsignificant, pathways.
Turning to the covariates, income was dropped from the model because it was not a significant predictor of treatment attendance with the other variables in the model. Race and parenting status remained: Latino (vs. White) race and parenting a young child both predicted significantly greater treatment attendance at p<.05. Based on modification indices, pathways were also included from race to MC-SDS score and URICA score. Results showed that participants self-categorizing as Other (vs. White) scored significantly higher on the MC-SDS (p<.01) and lower on the URICA (p<.001). Relationships shown in the figure remained very similar when a model was run excluding race and parenting status. For example, greater attendance was still associated with higher social desirability (B=.26, p<.01) and URICA (B=.25, p<.05) scores.
4. Discussion
4.1. Evidence that Social Desirability Can Affect Self-reported Stage of Change
The current study found good evidence that social desirability can affect self-reported stage of change. Results from both the bivariate and multivariate analyses showed that scores on the Marlowe Crowne Social Desirability Scale (MC-SDS) were strongly associated with lower self-reported stage of change, as assessed by the URICA. Respondents high on social desirability were especially likely to agree with items suggesting that they did not have any problems needing attention (e.g., “Being here is pretty much a waste of time for me because the problem doesn’t have to do with me,” and “As far as I’m concerned, I don’t have any problems that need changing”) and to disagree with items suggesting the opposite, or implying a lack of self-sufficiency (e.g., “At times my problem is difficult, but I am working on it,” and “I have started working on my problems, but I would like help”). Several items that did not fall into these categories, or that were positively worded, were not associated with the MC-SDS. These results suggests that individuals inclined to present themselves in socially desirable ways can be reluctant to admit that they have a serious drug or alcohol problem, and that they need help for the same, even on a confidential, computerized survey. Importantly, social desirability was not significantly related to TREAT scale scores or items, excepting one item (“I think I need help”). This makes sense because the remaining TREAT items adopt much milder language than does the URICA in referring to the respondents’ problems. Many items do not address problem recognition at all, but rather, target beliefs and behaviors that may be less emotionally evocative, such as opinions about treatment efficacy and treatment attendance patterns.
These findings have important implications for the development and administration of motivational readiness measures in substance-using populations. They highlight a strong need to account for the potential effect of social desirability in interpreting responses to such measures, since failing to do so could lead to distortions in the relationships of interest. The results also suggest that, in order to avoid such bias, it is desirable to avoid accusatory-sounding language regarding individuals’ problems, since such language is likely to elicit dissimulation.
Admittedly, results for the URICA are not consistent with results from a study conducted on anxiety, but also using the URICA (Dozois, Westra, Collins, Fung, & Garry, 2004). That study, sampling self-identified anxious undergraduates, found that stage of change (in relation to anxiety) was not associated with the MC-SDS. Also, in a follow-up study (same article), the Action subscale was a significant if modest predictor of treatment retention among individuals with panic disorder. This may indicate that socially desirable responding poses less of a problem for disorders that are less stigmatized than substance use problems, and hence, that the URICA may be a reasonable predictor of treatment retention in those cases.
4.2. Evidence that Social Desirability May Affect Treatment Attendance
Paralleling and extending Krasnoff’s (1976) early study, the current study also found, again in both bivariate and multivariate analyses, that higher social desirability was associated with greater treatment attendance. Although the association was modest, this is a noteworthy finding because it seems to imply an unrecognized source of treatment motivation: the desire to create a positive impression of oneself. Existing conceptualizations of treatment motivation have focused on both internal and external motivations for treatment (e.g., Ryan, Plant, & O’Malley, 1995), but external motivations have been largely conceptualized as legal pressures and/or social coercion, and self-image has not been emphasized. If this finding can be replicated, implications are that treatment retention might be maximized by capitalizing on this motivation. However, caution is warranted here, as the current data suggest that clients high on social desirability want to be seen as self-sufficient. Further, emphasizing social approval contingencies could alter or worsen treatment efficacy. It seems unlikely, in fact, that individuals whose attendance was based primarily on a desire for social approval would enjoy lasting benefits. Still, other motivations and processes may kick in once attendance has been initiated that do promote deeper change. Consistent with this argument, one prior study conducted on alcoholics found that higher social desirability was associated with better treatment outcomes (Yoshino & Kato, 1995). Regardless, more work on the association between social desirability and treatment-related mechanisms and outcomes is needed before firm conclusions can be drawn. Notably and contrary to our results, Strickland and Crowne (1963), in a very early study, found that social desirability was related to higher odds of termination from psychotherapy for psychiatric problems, suggesting that the relationship between social desirability and treatment-related behaviors and outcomes may depend on the nature of the problem and treatment.
4.3. Effects for Social Desirability on the Predictive Power of Stage of Change Scales
Of critical interest, the present study found that accounting for the effect of social desirability on treatment attendance yielded a moderately strong, significant association between higher URICA scores and more treatment attendance, whereas previously the association was null. Further, with both variables in the model, the association between social desirability and treatment attendance was also stronger.
This pattern of effects seems to imply suppressor effects. A suppressor variable is a variable that “increases the predictive value of another variable (or set of variables) by its inclusion in a regression equation” (Conger, 1974, p. 36). More specifically, results are consistent with Conger’s “reciprocal suppression,” which occurs where two variables are negatively correlated with each other but positively correlated with the outcome. In such cases, the bivariate effects for both predictors will typically be smaller than the effects generated when predictors are entered simultaneously, since in bivariate analyses the effect of an increase in one predictor is counteracted by the effect of the concomitant decrease in the other; conversely, multivariate analyses provide mutually adjusted effect estimates. Because social desirability and stage of change were negatively correlated in the current data, including them in the equation simultaneously allowed for a better estimate of their unique impact, and stronger results. This interpretation is bolstered by the finding of a robust pattern of effects for the MC-SDS and URICA even when eliminating covariates, and hence alternative explanations.
Implications are that the poor prior results for the URICA are partially attributable to the fact that individuals high on social desirability disagree with the URICA’s pro-change items, and that these same individuals also show high treatment attendance for other reasons. Indeed, in interpreting the URICA’s empirical record, theoretical problems may be secondary to the scale’s tendency to elicit biased responding from individuals concerned about appearing dysfunctional. TREAT total score was unrelated to treatment attendance, whether or not social desirability was in the model. This suggests that the TREAT is not a reliable predictor of attendance for reasons that do not involve social desirability. Further, we did not find evidence that the relationship between URICA score and treatment attendance was moderated by social desirability, countering expectations of a stronger relationship among respondents low on social desirability. It may be that power limitations explain the null effect, which should be especially severe given the somewhat restricted range in URICA total scores (M=3.92 of 5 possible; SD=.63).
4.4. Evidence that Social Desirability Can Affect Self-reported Problem Severity
Finally, across analyses, higher social desirability as measured by the MC-SDS was very strongly associated with lower self-reported ASI Alcohol, Drug, and Psychiatric severity (r’s=−.35 to −.37, p’s<.001). These results imply that relationships between self-reported problem severity in these domains and other variables obtained in the literature are subject to some suspicion. It remains unclear how failing to account for the effect of social desirability on these measures may have affected the reported results. Attenuation of the relationships seems likely in some cases, although more complex effects (and even the reverse pattern) may have obtained where social desirability was also related to the outcomes. To point, the current study found that, despite significant bivariate associations, there were no effects for ASI Drug and Psychiatric severity on either treatment attendance or URICA total score once the effect of social desirability was partialled out, suggesting that social desirability confounded and partly explains the bivariate effects. This means that associations between baseline severity and both higher stage of change and lower treatment attendance may be artefactual. Not too much should be made of these results, since power was limited for the multivariate analysis. Still, the findings are clearly provocative and should be pursued in further research. It will also be important for future research testing the effects of problem severity to directly account for potential interactions between social desirability and problem severity (see below).
4.5. Limitations
The current study suggests some important effects for social desirability with wide-reaching implications. However, the findings are somewhat difficult to interpret because it is not completely clear how social desirability was related to other clinical and personality variables in our sample. More to the point, it is not known whether social desirability was associated with genuinely better adaptation or psychological health, which could partially explain the observed effects for social desirability on treatment attendance and problem severity. Although this possibility cannot be completely discounted, it seems unlikely. It is true that the MC-SDS has been related to lower clinical severity (Crowne & Marlowe, 1960) and other adaptive traits such as lower sensation seeking, trait impulsivity, and trait hostility (Schell, et al., 2006; Welte & Russell, 1993). However, these associations do seem to stem from simple response biases and not associations between social desirability and better functioning: Supporting this point, there have now been several studies that have differentiated those defensively high on social desirability from those who are genuinely high on psychological functioning (see Evans, 1982, for a review). Still, future research would be helpful to confirm these findings. It would be particularly useful to examine associations between social desirability and more objective measures of problem severity (e.g., biological or implicit measures, see Roefs et al., 2011, on the latter).
A related point is that some particulars regarding the impact of social desirability remain to be specified. A prior study factor-analyzing various social desirability scales concluded that the Marlowe-Crowne actually taps two factors: other-deception and self-deception (Paulhus, 1984). So, a relationship between the MC-SDS and problem severity, for example, could reflect some impression management and some (less conscious) repression. Future work should attempt to disentangle the impact of each on sensitive questions. Subsequent research could also be directed toward identifying the contextual factors most likely to elicit response bias among treatment populations. Like many traits, social desirability may be more likely to be elicited in certain contexts. Some factors, such as coercion, may also affect response style to alcohol-and-drug-related questions, while they do not affect global behavior or responses to the (global) Marlowe-Crowne, complicating measurement (see Kim & Hill, 2003).
A more general limitation is that the current study was quite small. This limited our ability to detect any potential interaction between social desirability and stage of change in predicting treatment attendance, and may have produced nonrepresentative results as a result of sampling biases. Future research is needed to test replication of the results. Relatedly, generalizability to women, people of color, and individuals of higher socioeconomic status must be established, since our sample was predominantly male, White, and low on socioeconomic status.
4.6. Final Conclusions
Results tentatively suggest that social desirability can have substantial impact on responses to some stage of change scales, certainly including the URICA, and to questions regarding alcohol, drug, and psychiatric problems. Further, it appears that failing to account for these biases can lead to serious distortions. Results suggest a need to reconsider theoretically plausible relationships involving these variables, such as relationships between problem severity and both treatment retention and efficacy. Where standard measures of sensitive topics are used, investigators should consider incorporating a measure of social desirability and accounting for the same in evaluating relationships in their data. Further, new scales may be needed that show little sensitivity to social desirability (Del Boca &Darkes, 2003; Embree & Whitehead, 1993).
An important point here is that simply partialling out the effect of social desirability, although extremely common, is not sufficient to address problems associated with socially desirable responding. Using social desirability as a control will only strengthen a relationship under study if there are suppressor effects similar to those the current study found. It does not address the fundamental reality that, if social desirability concerns have biased responses to a survey measure, then position on that measure means something different, and must be interpreted differently, for individuals who are higher versus lower on social desirability. This implies that social desirability moderates associations involving the measure, and hence, calls for an interaction test. Careful studies addressing this and other response biases associated with core measures in the field would do much to advance the agenda of addictions research.
Acknowledgements
I gratefully acknowledge the support of the National Institute on Alcohol Abuse and Alcoholism, which funded the current study (#R21AA016578). Also, I would like to thank Lee Ann Kaskutas, who assisted with interpreting the study’s results, as well as the journal reviewers, whose contributions significantly improved this article.
Footnotes
In fact, it has been argued that stage theories in psychology are falsified more or less as a rule, excepting those in the domain of human development (Bandura, 1998; Robin Davidson, 1998).
Research fairly consistently suggests associations between higher treatment attendance and both higher drug (Blood & Cornwall, 1994; Brecht, Greenwell, & Anglin, 2005; Zanis, Coviello, Lloyd, & Nazar, 2009) and psychiatric (Blood & Cornwall, 1994; Evans, Li, & Hser, 2009; Green, Polen, Dickinson, Lynch, & Bennett, 2002; Haller & Miles, 2004; Mangrum, 2009; McMahon, 2008; Petry & Bickel, 1999) severity, as well as associations between higher stage of change and alcohol and drug problem severity (Carpenter, Miele, & Hasin, 2002; Field, Adinoff, Harris, Ball, & Carroll, 2009; Maisto et al., 2011; Satre, Chi, Eisendrath, & Weisner, 2011).
Table 4, displaying inter-correlations between stages for both scales, provides more information supportive of these scaling decisions (see Results).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ajzen I, Fishbein M. Attitude-behavior relations: a theoretical analysis and review of empirical research. Psychological Bulletin. 1977;84:888–918. [Google Scholar]
- Ashworth P. Breakthrough or bandwagon? Are interventions tailored to stage of change more effective than non-staged interventions? Health Education Journal. 1997;56:166–174. [Google Scholar]
- Aveyard P, Cheng K, Almond J, Sherratt E, Lancashire R, Lawrence T, Griffin C, Evans O. Cluster randomised controlled trial of expert system based on the transtheoretical (‘Stages of Change’) model for smoking prevention and cessation in schools. British Medical Journal. 1999;319:948–953. doi: 10.1136/bmj.319.7215.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballard R. Short forms of the Marlowe–Crowne Social Desirability Scale. Psychological Reports. 1992;71(3, Pt. 2):1155–1160. doi: 10.2466/pr0.1992.71.3f.1155. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology and Health. 1998;13:623–649. [Google Scholar]
- Blood L, Cornwall A. Pretreatment variables that predict completion of an adolescent substance abuse treatment program. Journal of Nervous and Mental Disease. 1994;182(1):14–19. doi: 10.1097/00005053-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Brecht M-L, Greenwell L, Anglin MD. Methamphetamine treatment: trends and predictors of retention and completion in a large state treatment system (1992-2002) Journal of Substance Abuse Treatment. 2005;29(4):295–306. doi: 10.1016/j.jsat.2005.08.012. [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Carey MP, De Martini KS. Individual-level interventions to reduce college student drinking: a meta-analytic review. Addictive Behaviors. 2007;32(11):2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter KM, Miele GM, Hasin DS. Does motivation to change mediate the effect of DSM-IV substance use disorders on treatment utilization and substance use? Addictive Behaviors. 2002;27(2):207–225. doi: 10.1016/s0306-4603(00)00178-7. [DOI] [PubMed] [Google Scholar]
- Conger AJ. A revised definition for suppressor variables: a guide to their identification and interpretation. Educational and Psychological Measurement. 1974;34(1):35–46. [Google Scholar]
- Crane LA, Leakey TA, Rimer BK, Wolfe P, Woodworth MA, Warnecke RB. Effectiveness of telephone outcall intervention to promote screening mammography among low income women. Preventive Medicine. 1998;27(5, Pt. 2):S39–S49. doi: 10.1006/pmed.1998.0395. [DOI] [PubMed] [Google Scholar]
- Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. Journal of Consulting Psychology. 1960;24(4):349–354. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- Davidson R. Prochaska and DiClemente’s model of change: a case study. British Journal of Addiction. 1992;87:821–822. doi: 10.1111/j.1360-0443.1992.tb01971.x. [DOI] [PubMed] [Google Scholar]
- Davidson R. The transtheoretical model: a critical overview. In: Miller WR, Heather N, editors. Treating Addictive Behaviors. 2nd. ed Plenum Press; New York, NY: 1998. pp. 25–38. [Google Scholar]
- Davis CG, Thake J, Vilhena N. Social desirability biases in self-reported alcohol consumption and harms. Addictive Behaviors. 2010;35(4):302–311. doi: 10.1016/j.addbeh.2009.11.001. [DOI] [PubMed] [Google Scholar]
- Deas D. Evidence-based treatments for alcohol use disorders in adolescents. Pediatrics. 2008;121(Suppl. 4):S348–S354. doi: 10.1542/peds.2007-2243G. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;98(Suppl. 2):1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari J, Zweben A, Morrel T, Lee RE. Motivation hypothesis causal chain analysis. In: Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and causal chain analyses. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. pp. 206–222. [Google Scholar]
- DiClemente CC, Prochaska JO. Toward a comprehensive, transtheoretical model of change: stages of chage and addictive behaviors. In: Miller WR, Health N, editors. Treating Addictive Behaviors. 2nd ed Plenum Press; New York, NY: 1998. pp. 3–24. [Google Scholar]
- Dozois DJA, Westra HA, Collins KA, Fung TS, Garry JKF. Stages of change in anxiety: psychometric properties of the University of Rhode Island Change Assessment (URICA) Behaviour Research and Therapy. 2004;42(6):711–729. doi: 10.1016/S0005-7967(03)00193-1. [DOI] [PubMed] [Google Scholar]
- Embree BG, Whitehead PC. Validity and reliability of self-reported drinking behavior: dealing with the problem of response bias. Journal of Studies on Alcohol. 1993;54(3):334–344. doi: 10.15288/jsa.1993.54.334. [DOI] [PubMed] [Google Scholar]
- Evans E, Li L, Hser Y-I. Client and program factors associated with dropout from court mandated drug treatment. Evaluation and Program Planning. 2009;32(3):204–212. doi: 10.1016/j.evalprogplan.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans RG. Clinical relevance of the Marlowe-Crowne Scale: a review and recommendations. Journal of Personality Assessment. 1982;46(4):415–425. doi: 10.1207/s15327752jpa4604_14. [DOI] [PubMed] [Google Scholar]
- Farkas AJ, Pierce JP, Shu S-H, Rosbrook B, Gilpin EAB,C, Kaplaj RM. Addiction versus stages of change models in predicting smoking cessation. Addiction. 1996;91(9):1271–1280. [PubMed] [Google Scholar]
- Field CA, Adinoff B, Harris TR, Ball SA, Carroll KM. Construct, concurrent and predictive validity of the URICA: data from two multi-site clinical trials. Drug and Alcohol Dependence. 2009;101(1-2):115–123. doi: 10.1016/j.drugalcdep.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Belief, Attitude, Intention and Behavior: An introduction to theory and research. Addison-Wesley Publishers; Reading, MA: 1975. [Google Scholar]
- Freyer J, Tonigan JS, Keller S, John U, Rumpf H-J, Hapke U. Readiness to change versus readiness to seek help for alcohol problems: the development of the Treatment Readiness Tool (TReaT) Journal of Studies on Alcohol. 2004;65(5):801–909. doi: 10.15288/jsa.2004.65.801. [DOI] [PubMed] [Google Scholar]
- Green CA, Polen MR, Dickinson DM, Lynch FL, Bennett MD. Gender differences in predictors of initiation, retention, and completion in an HMO-based substance abuse treatment program. Journal of Substance Abuse Treatment. 2002;2002(23):4. doi: 10.1016/s0740-5472(02)00278-7. [DOI] [PubMed] [Google Scholar]
- Greene GW, Rossi SR. Stages of change for reducing dietary fat intake over 18 months. Journal of the American Dietetic Association. 1998;98(5):529–534. doi: 10.1016/S0002-8223(98)00120-5. [DOI] [PubMed] [Google Scholar]
- Haller DL, Miles DR. Psychopathology is associated with completion of residential treatment in drug dependent women. Journal of Addictive Diseases. 2004;23(1):17–28. doi: 10.1300/J069v23n01_02. [DOI] [PubMed] [Google Scholar]
- Kim MT, Hill MN. Validity of self-report of illicit drug use in young hypertensive urban African American males. Addictive Behaviors. 2003;28(4):795–802. doi: 10.1016/s0306-4603(01)00277-5. [DOI] [PubMed] [Google Scholar]
- Klag S, Creed P, O’Callaghan F. Development and initial validation of an instrument to measure perceived coersion to enter treatment for substance abuse. Psychology of Addictive Behaviors. 2006;20(4):463–470. doi: 10.1037/0893-164X.20.4.463. [DOI] [PubMed] [Google Scholar]
- Krasnoff A. Differences between alcoholics who complete or withdraw from treatment. Journal of Studies on Alcohol. 1976;37(11):1666–1671. doi: 10.15288/jsa.1976.37.1666. [DOI] [PubMed] [Google Scholar]
- Lancaster T, Dobbie W, Vos K, Yudkin P, Murphy M, Flowler G. Randomised trial of nurse-assisted strategies for smoking cessation in primary care. British Journal of General Practice. 1999;49(440):191–194. [PMC free article] [PubMed] [Google Scholar]
- Lessler JT, O’Reilly JM. Mode of interview and reporting of sensitive issues: design and implementation of audio computer-assisted self-interviewing. In: Harrison L, Hughes A, editors. Validity of Self-reported Drug Use. Improving the accuracy of survey estimates. National Institute on Drug Abuse; Rockville, MD: 1997. pp. 366–382. [PubMed] [Google Scholar]
- Littell JH, Girvin H. Stages of change: a critique. Behavior Modification. 2002;26(2):233–273. doi: 10.1177/0145445502026002006. [DOI] [PubMed] [Google Scholar]
- Loo R, Loewen P. Confirmatory factor analyses of scores from full and short versions of the Marlowe–Crowne Social Desirability Scale. Journal of Applied Social Psychology. 2004;34(11):2343–2352. doi: 10.1080/00224540009600503. [DOI] [PubMed] [Google Scholar]
- Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: a practice-friendly review of four meta-analyses. Journal of Clinical Psychology. 2009;65(11):1232–1245. doi: 10.1002/jclp.20638. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Krenek M, Chung T, Martin CS, Clark D, Cornelius J. Comparison of the concurrent and predictive validity of three measures of readiness to change marijuana use in a clinical sample of adolescents. Journal of Studies on Alcohol and Drugs. 2011;72(4):592–601. doi: 10.15288/jsad.2011.72.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangrum LF. Client and service characteristics associated with addiction treatment completion of clients with co-occurring disorders. Addictive Behaviors. 2009;34(10):898–904. doi: 10.1016/j.addbeh.2009.03.006. [DOI] [PubMed] [Google Scholar]
- McConnaughy EA, DiClemente CC, Prochaska JO, Velicer WF. Stages of change in psychotherapy: a follow-up report. Psychotherapy: Theory, Research, Practice, Training. 1989;26(4):494–503. [Google Scholar]
- McLellan AT, Luborsky L, Cacciola JS, Griffith J. Guide to the addiction severity index: background, administration, and field testing results. U.S. Department of Health and Human Services, National Institute on Drug Abuse; Rockville, MD: 1985. [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. The Journal of Nervous and Mental Disease. 1980;168(1):26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- McMahon RC. Substance abuse problems, psychiatric symptoms, and post-treatment status in MCMI psychopathology subgroups of cocaine dependent males. American Journal of Alcohol Abuse. 2008;34(2):195–202. doi: 10.1080/00952990701877094. [DOI] [PubMed] [Google Scholar]
- Mee-Lee D, Shulman GD, Fishman M, Gastfriend DR, Griffith JH, editors. ASAM Patient Placement Criteria for the Treatment of Substance-Related Disorders. 2nd. rev. ed American Society of Addiction Medicine, Inc.; Chevy Chase, MD: 2001. [Google Scholar]
- Migneault JP, Adams TB, Read JP. Application of the Transtheoretical Model to substance abuse: historical development and future directions. Drug and Alcohol Review. 2005;24(5):437–448. doi: 10.1080/09595230500290866. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers’ motivation for change: the Stages of Change Readiness and Treatment Eagerness (SOCRATES) Psychology of Addictive Behaviors. 1996;10(2):81–89. [Google Scholar]
- Muthén LK, Muthén B. Mplus Version 5. Muthén & Muthén; Los Angeles, CA: 2007. [Google Scholar]
- Naylor P, Simmonds G, Riddoch C, Velleman G, Turton P. Comparison of stage-matched and unmatched interventions to promote exercise behaviour in the primary care setting. Health Education Research. 1999;14:653–666. doi: 10.1093/her/14.5.653. [DOI] [PubMed] [Google Scholar]
- O’Reilly JM, Hubbard M, Lessler JT, Biemer P, Turner CF. Audio and video computer-assisted self-interviewing: preliminary tests of new technologies for data collection. Journal of Official Statistics. 1994;10(2):197–214. [PMC free article] [PubMed] [Google Scholar]
- Pantalon MV, Swanson AJ. Use of the University of Rhode Island Change Assessment to measure motivational readiness to change in psychiatric and dually diagnosed individuals. Psychology of Addictive Behaviors. 2003;17(2):91–107. doi: 10.1037/0893-164x.17.2.91. [DOI] [PubMed] [Google Scholar]
- Paulhus DL. Two-component models of socially desirable responding. Journal of Personality and Social Psychology. 1984;46(3):598–609. [Google Scholar]
- Petry NM, Bickel WK. Therapeutic alliance and psychiatric severity as predictors of treatment for opioid dependence. Psychiatric Services. 1999;50(2):219–227. doi: 10.1176/ps.50.2.219. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Norcross JC. Stages of change. Psychotherapy. 2001;38(4):443–448. [Google Scholar]
- Project MATCH Research Group Matching alcoholism treatment to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58(1):7–29. [PubMed] [Google Scholar]
- Reynolds WM. Development of reliable and valid short forms of the Marlowe–Crowne Social Desirability Scale. Journal of Clinical Psychology. 1982;38(1):119–125. [Google Scholar]
- Roefs A, Huijiding J, Smulders FTY, MacLeod CM, de Jong PJ, Wiers RW, Jansen ATM. Implicit measures of association in psychopathology research. Psychological Bulletin. 2011;137(1):149–193. doi: 10.1037/a0021729. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. The British Journal of Addiction. 1992;87:743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Plant RW, O’Malley S. Initial motivations for alcohol treatment: relations with patient characteristics, treatment involvement, and dropout. Addictive Behaviors. 1995;20(3):279–297. doi: 10.1016/0306-4603(94)00072-7. [DOI] [PubMed] [Google Scholar]
- Satre DD, Chi FW, Eisendrath S, Weisner C. Subdiagnostic alcohol use by depressed men and women seeking outpatient psychiatric services: consumption patterns and motivation to reduce drinking. Alcoholism: Clinical and Experimental Research. 2011;35(4):695–702. doi: 10.1111/j.1530-0277.2010.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schell TL, Chan KS, Morral AR. Predicting DUI recidivism: personality, attitudinal, and behavioral risk factors. Drug and Alcohol Dependence. 2006;82(1):33–40. doi: 10.1016/j.drugalcdep.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Doherty S, Rink E, Kerry SM, Kendrick T, Hilton S. Behavioural conselling in general practice for the promotion of healthy behaviour among adults at increased risk of coronary heart disease. British Medical Journal. 1999;319:943–948. doi: 10.1136/bmj.319.7215.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland BR, Crowne DP. Need for approval and the premature termination of psychotherapy. Journal of Consulting Psychology. 1963;27(2):95–101. doi: 10.1037/h0040686. [DOI] [PubMed] [Google Scholar]
- Sutton S. Can ‘stages of change’ provide guidance in the treatment of addiction? A critical examination of Prochaska and DiClemente’s model. In: Edwards G, Dare C, editors. Psychotherapy, Psychological Treatment and the Addictions. Cambridge University Press; Cambridge, UK: 1996a. pp. 189–205. [Google Scholar]
- Sutton S. Further support for the stages of change model? Addiction. 1996b;91(9):1287–1289. doi: 10.1111/j.1360-0443.1996.tb03613.x. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 2nd ed Harper & Row; New York, NY: 1989. [Google Scholar]
- Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol and Alcoholism. 2006;41(3):328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- Welte JW, Russell M. Influence of socially desirable responding in a study of stress and substance abuse. Alcoholism: Clinical and Experimental Research. 1993;17(4):758–761. doi: 10.1111/j.1530-0277.1993.tb00836.x. [DOI] [PubMed] [Google Scholar]
- Whitelaw S, Baldwin S, Bunton R, Flynn D. The status of evidence and outcomes in stages of change research. Health Education Research. 2000;15(6):707–718. doi: 10.1093/her/15.6.707. [DOI] [PubMed] [Google Scholar]
- Yoshino A, Kato M. Influence of social desirability response set on self-report for assessing the outcome of treated alcoholics. Alcoholism: Clinical and Experimental Research. 1995;19(6):1517–1519. doi: 10.1111/j.1530-0277.1995.tb01016.x. [DOI] [PubMed] [Google Scholar]
- Zanis DA, Coviello DM, Lloyd JJ, Nazar BL. Predictors of drug treatment completion among parole violators. Journal of Psychoactive Drugs. 2009;41(2):173–180. doi: 10.1080/02791072.2009.10399910. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Ajzen I, O’Hearn P. An application of the theory of planned behavior to substance abuse treatment completion. Alcohol Research Group, Public Health Institute; Emeryville, CA: 2011. under review. [Google Scholar]