Abstract
Introduction
Cardiac syndrome X (CSX) is characterized by anginal pain with ECG suggestive of ischaemia and normal coronary arteries at angiography. Pathology of CSX involves microvascular dysfunction and is possibly linked with metabolic syndrome. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) is an enzyme involved in glycolysis. The GAPDH gene is a “housekeeping” gene and is used for normalization in quantitative gene expression assays. The aim of the study was to evaluate GAPDH gene expression in CSX.
Material and methods
The study was performed in 35 CSX patients and 10 control subjects. mRNA was extracted from peripheral blood mononuclears and the mRNA was assessed by QRT-PCR.
Results
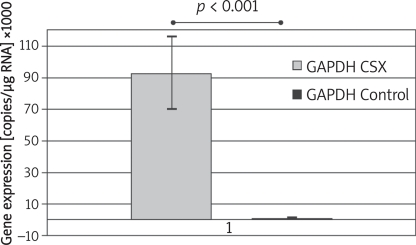
GAPDH gene expression was enhanced in CSX patients vs. controls (93022 ±23837 copies/μg vs. 1067 ±240 copies/μg respectively; p < 0.001). Moreover, transcriptional activity of the GAPDH gene was heterogeneous within the CSX group.
Conclusions
GAPDH gene expression is markedly enhanced in CSX, which reflects carbohydrate metabolism disturbances and makes the GAPDH gene unsuitable as an endogenous control in patients with CSX.
Keywords: GAPDH, cardiac syndrome X, gene expression
Introduction
Cardiac syndrome X (CSX, also referred to as microvascular angina) is characterized by effort-induced chest pain with ECG suggestive of ischaemia and normal coronary arteries at angiography [1]. In spite of better and better non-invasive techniques in the diagnostics of angina, about 20% of patients presenting with angina are still found to have a normal or near normal coronary angiogram.
The pathogenesis of syndrome X remains unclear. Two major abnormalities are thought to play a crucial role: microvascular dysfunction (with an underlying inflammatory process affecting endothelial cells) and abnormal pain sensitivity [1-2]. Recently evidence has been gathered to support the hypothesis that there is a link between microvascular angina and metabolic syndrome – a constellation of cardiovascular risk factors (obesity, dyslipidaemia, hypertension and glucose metabolism disturbances) resulting mainly from hyperinsulinaemia [3]. According to the literature, including data from our research, the pro-inflammatory state affecting endothelium in CSX patients is also reflected by activation of circulating inflammatory cells and cytokines [4, 5, 6, 7].
Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) is an enzyme participating in glucose metabolism, particularly glycolysis. The protein, however, has been reported to possess a variety of diverse biological functions including control of gene expression and more [8].
The GAPDH gene is one of the constitutive and so-called ‘housekeeping’ genes which are expressed at all stages of the cell’s life cycle. Warrington et al. indicated more than 500 such genes; however, only 47 of them keep the same level of transcriptional activity all the time and may therefore be used as an endogenous control and a standard for normalization in quantitative gene expression analyses [9]. Although under some conditions GAPDH gene expression is highly inducible, it is still one of the best characterized and therefore commonly used for normalization of gene expression in experiments [10].
The aim of this study was to evaluate expression of the GAPDH gene in CSX and to determine whether it is suitable as a normalization standard for quantitative gene expressions analysis in these patients.
Material and methods
Patients
The study was carried out in 35 patients aged 44- 77 (average 57 years old; M/F: 13/22) with CSX during their symptomatic period (patients with positive exercise test admitted to the hospital due to recurrent chest pain in which coronary angiography was found to be normal). Treatment in the CSX group involved: nitrates (10 pts, 28.5%) statins (22 pts, 62.9%) ACE inhibitors (18 pts, 51.4%) and β-blockers (27 pts, 77%). The control group consisted of 10 sexand age-matched healthy subjects (aged 39-66, average 56 years old; M/F: 3/7).
In each patient basic laboratory tests, ECG and echocardiography were performed. Patients with diabetes, arterial hypertension, chronic inflammatory diseases, chronic heart failure and renal failure were excluded. Informed consent was obtained from each patient.
Blood samples (10 mL) were collected into tubes containing EDTA and peripheral blood mononuclear cells (PBMC) were separated by Histopaque (Sigma, USA) density gradient centrifugation.
RNA extraction
Total RNA was extracted from PBMC using the phenol-chloroform method. All extracts were treated with DNase I to avoid contamination by genomic DNA. The RNA extracts were qualitatively evaluated by electrophoresis in 1% agarose gel stained with ethidium bromide, and quantitated spectrophotometrically (Gene Quant II by Pharmacia).
Primers
Primers for amplification of GAPDH and β-actin were determined using the Primer Express Version 1.0 computer program (PE Applied Biosystems, USA), and their sequence homologies were checked using the GenBank database. Primers sequences were the following:
GAPDH:
5’ GAAGGTGAAGGTCGGAGTCA 3’ (forward),
5’ GAAGATGGTGATGGGATTTC 3’ (reverse),
β-actin:
5’ TCACCCACATGTGCCCATCTACGA 3’ (forward),
5’ CAGCGGAACCGCTCATTGCCAATGG 3’ (reverse).
Real-time PCR (QRT-PCR)
Quantitative reverse transcriptase polymerase chain reaction (QRT-PCR) was performed using QuantiTect SYBR Green RT-PCR. Cycling conditions were as follows: RT: 60°C for 30 min; polymerase activation: 94°C for 15 min; PCR: 94°C for 15 s and 68°C for 30 s, 40 cycles; final elongation: 72°C for 10 min. QRT-PCR specificity was confirmed experimentally by PAA electrophoresis, amplimers’ melting temperature measurement using ABI PRISM7000 (SYBR Green RT-PCR Kit), and sequence analysis using ABI PRISM 377 DNA Sequencer (PE Applied Biosystems). The obtained results were recalculated to 1 μg of total RNA.
Statistical analysis
All values were expressed as means ± standard error (AVG ± SEM). In order to check the normality of the distribution, the Shapiro-Wilk test was performed. Since the distribution was not normal the Mann-Whitney U test was used to compare the groups.
The investigation conforms to the principles outlined in the Declaration of Helsinki.
Results
Results are expressed as the number of mRNA copies of the assessed gene per 1 microgram of total mRNA (c/μg).
We observed a tremendously higher level of GAPDH gene expression in CSX patients vs. the control group (93022 ±23837 copies/μg vs. 1067 ±240 copies/μg respectively; p < 0.001) (Figure 1). β-actin gene expression was not different between the control and study group (p = NS).
Figure 1.
Transcriptional activity of GAPDH gene in CSX vs. Control subjects
Only samples that underwent RNA quality control were subject to statistical analysis. The RNA integrity number (RIN) for analysed samples was 6.6-8.4, which allows us to conclude that the quality of RNA in studied samples was comparable and the observed results are due to differences in transcriptional activity of the GAPDH gene between CSX and control subjects.
We did not find any correlation between studied gene expression and any of the medications the studied patients had been administered.
Discussion
The GAPDH gene is a widely used constitutive gene in quantitative assays of expression of various genes in tissues and systems. According to Barber and coworkers, who studied GAPDH gene expression in 72 healthy tissues, it shows small within-tissue variation and seems to be a good standard for normalization [10]. Under pathological circumstances, however, some factors may cause alterations in activity of genes that are normally expressed at a constant level. In this study we have demonstrated that 1) transcriptional activity of the GAPDH gene is significantly higher in mononuclears from CSX patients and 2) cannot therefore be a good endogenous control in this pathology.
As stated, PBMC from patients with syndrome X present with increased activity and enhanced generation of oxidative stress. According to our previous reports [5, 6] mononuclears from CSX patients overexpress pro-inflammatory genes, i.e. interferon gamma receptor or kinin signalling system. GAPDH, despite being commonly used as a constitutive gene, has been shown to be disturbed in various conditions. It has been proved that inflammatory factors [11], hyperinsulinaemia [12] and finally hypoxia [13] may enhance transcriptional activity of GAPDH. There are also other factors to influence GAPDH activity (glucose, NO, superoxide) [11, 14], although their effect has not been studied at the transcriptional level.
Increased activity of the GAPDH gene observed in our study may be related to enhanced activation of circulating mononuclears, the proinflammatory state and increased oxidative stress. However, this study was not designed to specify which mechanism was responsible for GAPDH gene expression. To rule out major glucose metabolism disturbances, patients with pre-diabetes and diabetes were excluded.
Apart from pathology of CSX itself, pharmacological treatment might have had an effect on GAPDH gene expression. As presented, treatment in the CSX group involved statins, beta-blockers and ACE inhibitors – groups of drugs of known anti-inflammatory effect and gene expression down-regulating potential. However, we did not observe a correlation of GAPDH expression with any treatment, which may have been due to the small number of participants – a major limitation of the study.
Apart from glycolysis, GAPDH is a protein involved in a number of processes [9] and elevated GAPDH expression might also reflect processes which are not yet well evaluated. To confirm that however, more thorough research needs to be performed.
In conclusion, transcriptional activity of the GAPDH gene in PBMC from patients with syndrome X is markedly enhanced. The increased activity may be due to an inflammatory state, may result from prolonged hypoxia, or may reflect subclinical glucose metabolism disturbance in CSX patients. Moreover, such enhanced activity and heterogeneity of GAPDH gene expression does not allow it to be used as a standard for endogenous control in patients with CSX.
References
- 1.Kemp HG., Jr Left ventricular function in patients with the anginal syndrome and normal coronary angiograms. Am J Cardiol. 1973;32:375–6. doi: 10.1016/s0002-9149(73)80150-x. [DOI] [PubMed] [Google Scholar]
- 2.Vázquez-Rey E, Kaski JC. Cardiovascular syndrome X and endothelial dysfunction. Rev Esp Cardiol. 2003;56:181–92. doi: 10.1016/s0300-8932(03)76843-2. [DOI] [PubMed] [Google Scholar]
- 3.Jadhav ST, Ferrell WR, Petrie JR, et al. Microvascular function, metabolic syndrome, and novel risk factor status in women with cardiac syndrome X. Am J Cardiol. 2006;97:1727–31. doi: 10.1016/j.amjcard.2005.12.069. [DOI] [PubMed] [Google Scholar]
- 4.Leu HB, Lin CP, Lin WT, Wu TC, Lin SJ, Chen JW. Circulating mononuclear superoxide production and inflammatory markers for long-term prognosis in patients with cardiac syndrome X. Free Radic Biol Med. 2006;40:983–91. doi: 10.1016/j.freeradbiomed.2005.10.047. [DOI] [PubMed] [Google Scholar]
- 5.Dabek J, Wilczok T, Gasior Z, Kucia-Kuzma S, Twardowski R, Kulach A. Gene expression of kinin receptors B1 and B2 in PBMC from patients with cardiac syndrome X. Scand Cardiovasc J. 2007;41:391–6. doi: 10.1080/14017430701499379. [DOI] [PubMed] [Google Scholar]
- 6.Dabek J, Kulach A, Wilczok T, Mazurek U, Jakubowski D, Gasior Z. Transcriptional activity of genes encoding interferon gamma (IFNgamma) and its receptor assessed in peripheral blood mononuclear cells in patients with cardiac syndrome X. Inflammation. 2007;30:125–9. doi: 10.1007/s10753-007-9028-0. [DOI] [PubMed] [Google Scholar]
- 7.Li JJ, Zhu CG, Nan JL, et al. Elevated circulating inflammatory markers in female patients with cardiac syndrome X. Cytokine. 2007;40:172–6. doi: 10.1016/j.cyto.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Sirover MA. Role of the glycolytic protein, glyceraldehyde- 3-phosphate dehydrogenase, in normal cell function and in cell pathology. J Cell Biochem. 1997;66:133–40. [PubMed] [Google Scholar]
- 9.Warrington JA, Nair A, Mahadevappa M, Tsyganskaya M. Comparison of human adult and fetal expression and identification of 535 housekeeping/maintenance genes. Physiol Genomics. 2000;2:143–7. doi: 10.1152/physiolgenomics.2000.2.3.143. [DOI] [PubMed] [Google Scholar]
- 10.Barber RD, Harmer DW, Coleman RA, Clark BJ. GAPDH as a housekeeping gene: analysis of GAPDH mRNA expression in a panel of 72 human tissues. Physiol Genomics. 2005;21:389–95. doi: 10.1152/physiolgenomics.00025.2005. [DOI] [PubMed] [Google Scholar]
- 11.Bereta J, Bereta M. Stimulation of glyceraldehyde-3- phosphate dehydrogenase mRNA levels by endogenous nitric oxide in cytokine-activated endothelium. Biochem Biophys Res Commun. 1995;217:363–9. doi: 10.1006/bbrc.1995.2785. [DOI] [PubMed] [Google Scholar]
- 12.Alexander-Bridges M, Dugast I, Ercolani L, Kong XF, Giere L, Nasrin N. Multiple insulin-responsive elements regulate transcription of the GAPDH gene. Adv Enzyme Regul. 1992;32:149–59. doi: 10.1016/0065-2571(92)90014-q. [DOI] [PubMed] [Google Scholar]
- 13.Graven KK, McDonald RJ, Farber HW. Hypoxic regulation of endothelial glyceraldehyde-3-phosphate dehydrogenase. Am J Physiol. 1998;274(2 Pt 1):C347–355. doi: 10.1152/ajpcell.1998.274.2.C347. [DOI] [PubMed] [Google Scholar]
- 14.Knight RJ, Kofoed KF, Schelbert HR, Buxton DB. Inhibition of glyceraldehyde-3-phosphate dehydrogenase in postischaemic myocardium. Cardiovasc Res. 1996;32:1016–23. doi: 10.1016/s0008-6363(96)00137-x. [DOI] [PubMed] [Google Scholar]