Fig. 4.
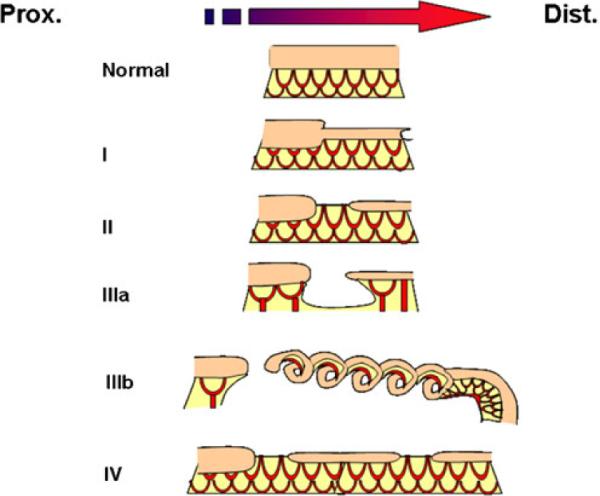
Atresias range in severity from a segmental narrowing or stenosis of the intestine to much more severe defects where there is an absence of a segment of the intestine and its blood supply. They are categorized based on increasing severity of the defect determined by three factors: (1) loss on intestinal tissue, (2) disruption of the accompanying intestinal blood supply, and (3) number of defects present. Type I atresias are a defect in which the intestinal mesoderm remains in continuity, but the lumen is obstructed by a diaphragm of tissue. In some cases, there is a small central opening, which allows for the restricted passage of contents. This variant includes the defect known as intestinal stenosis. Type II atresias are a defect wherein a small solid core of tissue connects the proximal and distal portions of the intestine; the core of tissue entirely lacks a lumen. In type IIIa atresias, the affected segment of intestine disappears and a V-shaped defect is visible in the adjacent mesentery or blood supply to the intestine. Type IIIb defects have an extensive gap in the blood supply between the proximal and distal limbs in intestine and they are frequently referred to as “apple peel defects” or “Christmas tree defects” because the distal limb of the bowel coils around its own mesentery. Type IV atresias have multiple points of interruption in the intestine, but the intestinal mesentery remains largely intact
