Abstract
A young male patient complaining of vague abdominal pain, dyspnea, generalized weakness and abdominal distension for 6 months was referred for abdominal ultrasound. Ultrasound showed enlarged echogenic kidneys, perinephric and renal sinus cystic fluid collections bilaterally with ascites and right pleural effusion. The ultrasound findings were confirmed by abdomen CT scan. Renal function test was within normal. Laboratory analysis of aspirated perinephric fluid revealed abundant lymphocytes. The radiological findings and perinephric fluid aspiration analysis are consistent with renal lymphangiectasia. Pleural effusion, in addition to ascites and perinephric fluid collections, is a new presentation of the disease. Ascites and pleural effusion were improved by diuretics.
Keywords: Renal, lymphatic, cysts, pleural effusion, ascites, renal lymphangiectasia
CASE REPORT
A 22-year-old male presented with a history of generalized weakness, progressive abdominal distension, vague abdominal pain and dyspnea for 6 months. He had no other significant past or family history. On examination, his blood pressure was 120/70 mmHg. Urine analysis was normal, hemoglobin level 15 mg dl-1(13–18 dl-1), urea 20.8 mg dl-1(10–50 dl-1), creatinine 1.37 mg dl-1(1.6 mg dl-1), serum potassium 3.9 mEq l-1(3.3–5.5 mEq l-1), serum albumin 3.9 mg dl-1(3.5–5.0 mg dl-1), SGPT 24 IU/L (5 to 40 IU/L), SGOT 27 IU/L (10 to 40 IU/L) and ALP 90 IU/L (30 to 120 IU/L).
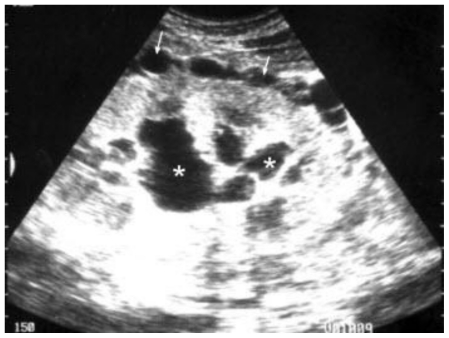
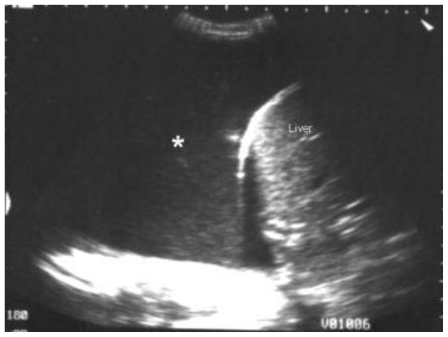
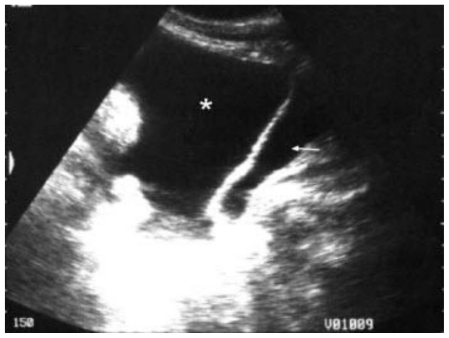
Ultrasound revealed enlarged echogenic kidneys, each measured about 14 cm long with perinephric and renal sinus cystic fluid collections bilaterally (figure 1) as well as right pleural effusion (figure 2) and ascites (figure 3).
Figure 1.
Abdomen ultrasound of a 22 male patient with renal lymphangiectasia, done by Siemens-sienna machine using a convex transducer of 3.5 MHz. The grayscale coronal view at the right flank shows enlarged right kidney, about 14 cm long, with renal sinus cysts (asterisks) and perinephric collections (arrows).
Figure 2.
Abdomen ultrasound of a 22 male patient with renal lymphangiectasia, done by Siemens-sienna machine using a convex transducer of 3.5 MHz. The grayscale coronal oblique view at the right hypochondrial region shows massive right pleural effusion (asterisk).
Figure 3.
Abdomen ultrasound of a 22 male patient with renal lymphangiectasia, done by Siemens-sienna machine using a convex transducer of 3.5 MHz. The grayscale sagittal view in the suprapubic region shows ascites (asterisk) with contracted urinary bladder (arrow).
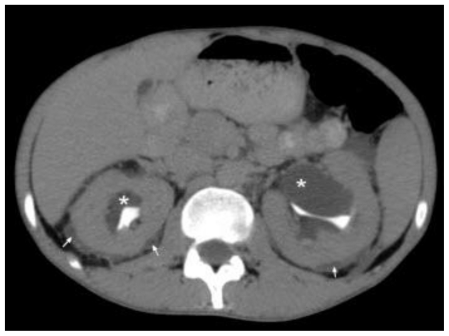
Abdomen CT scan showed bilateral perinephric fluid collections, which were almost symmetrical (figure 4), right pleural effusion (figure 5) and gross ascites (figure 5 and 6). No cystic areas were seen in the pancreas or liver. No other abnormality was found on the CT scan. The mean CT density of the renal sinus cysts was 3 Hounsfield units. The mean CT density of the perinephric fluid collection was 2, of the pleural effusion; 3 and that of ascites; 3 Hounsfield units, suggesting transudate.
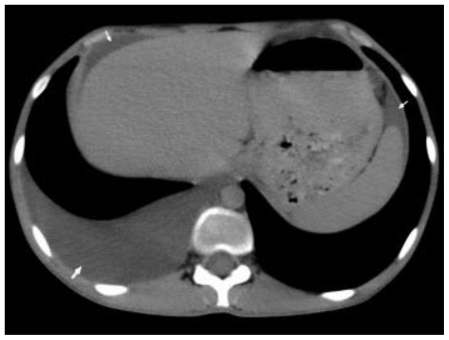
Figure 4.
Abdomen CT scan of a 22 male patient with renal lymphangiectasia. The examination was done by Brilliance 64 Philips machine; kV 120.0, mAs 246 and 3 mm slice thickness. Oral contrast and 70 ml IV contrast (ultravist) were given. The axial contrast enhanced section in the excretory phase at level of the upper abdomen shows renal sinus cysts (asterisks) and perinephric fluid collections (arrows) bilaterally.
Figure 5.
Abdomen CT scan of a 22 male patient with renal lymphangiectasia. The examination was done by Brilliance 64 Philips machine; kV 120.0, mAs 246 and 3 mm slice thickness. Oral contrast and 70 ml IV contrast (Ultravist) were given. The axial contrast enhanced section in the excretory phase at level of the upper abdomen shows Rt. pleural effusion (thick arrow) and ascites (thin arrows).
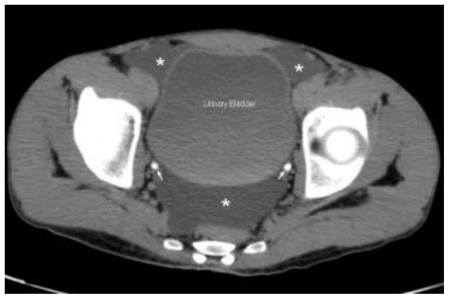
Figure 6.
Abdomen CT scan of a 22 male patient with renal lymphangiectasia. The examination was done by Brilliance 64 Philips machine; kV 120.0, mAs 246 and 3 mm slice thickness. Oral contrast and 70 ml IV contrast (Ultravist) were given. The axial contrast enhanced section in the excretory phase at level of the pelvis shows ascites (asterisks). Ureters are filled with contrast (arrows).
Needle aspiration of the perinephric fluid was carried out, and laboratory analysis revealed abundant lymphocytes. This patient underwent anti TB treatment for one year with no improvement and the pleural effusion and ascites were improved by diuretics only (figures 7 and 8).
Figure 7.
Follow up abdomen CT scan of a 22 male patient with renal lymphangiectasia. The examination was done by Brilliance 64 Philips machine; kV 120.0, mAs 246 and 3 mm slice thickness. Oral contrast and 70 ml IV contrast (Ultravist) were given. The axial contrast enhanced section in the excretory phase at level of the upper abdomen shows relative improvement in the Rt. pleural effusion (arrow).
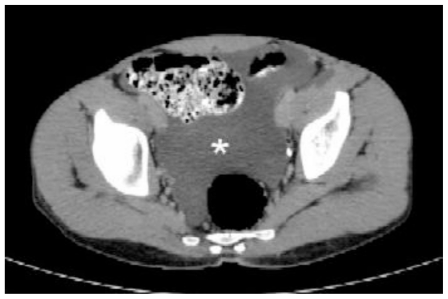
Figure 8.
Follow up abdomen CT scan of a 22 male patient with renal lymphangiectasia. The examination was done by Brilliance 64 Philips machine; kV 120.0, mA 246 and 3 mm slice thickness. Oral contrast and 70 ml IV contrast (Ultravist) were given. The axial contrast enhanced section in the excretory phase at level of the pelvis shows relative improvement in the ascites (asterisk).
DISCUSSION
Renal lymphangiectasia is a rare benign disorder of renal lymphatics that has been confused with other cystic disease of the kidney (1). Knowledge of the condition is based mostly on solitary case reports. Approximately 40 cases have been reported since 1890 (2). It is known by many different names including renal lymphangiomatosis (1), renal lymphangioma (3), renal peripelvic multicystic lymphangiectasia" (4), peripelvic lymphangiectasia (5), hygroma renale (2) and polycystic disease of the renal sinus (6). The origins and cause of the condition are unclear (7).
Clinically, it is usually asymptomatic and incidentally diagnosed. When symptomatic, the most common presentations are abdominal pain (42%), abdominal distension (21%), followed by fever, haematuria, fatigue, weight loss and hypertension and occasional deterioration in renal function (mostly reversible) (2,7).
Imaging findings of renal lymphangiectasia include peripelvic cysts and perirenal fluid collections (1,5,6,8). On sonography, characteristics of simple cysts are seen. Cysts are seen to be anechoic, with enhancement through transmission and a sharply defined far wall (3). Kidneys may appear enlarged, and cortico-medullary differentiation may be lost (1). On CT, similar appearances of fluid collections are seen, but the septa may not be very conspicuous. The attenuation within the cysts lies in the range of fluid (7,9). Surrounding structures are not seen to be invaded, but only abutted or displaced. Ascites may be found, and is a known complication. However, features on ultrasound and CT are known to be diagnostic of the condition (9).
Differentials of renal lymphangiectasia include polycystic renal disease, nephroblastomatosis, lymphoma and multilocular cystic nephroma depending on the age and appearance of the disease (6,9). The diagnosis of renal lymphangiectasia can be confirmed with needle aspiration of chylous fluid from the perinephric fluid collections (6).
Causes of ascites (as shown in table 1) can be classified according to if associated with peritoneal diseases or not (10).
Table 1.
Causes of ascites according to if associated with peritoneal disease or not.
| Without Peritoneal Disease: |
| Portal hypertension |
| Cirrhosis |
| Alcoholic hepatitis |
| Hepatic congestion |
| Congestive heart failure |
| Tricuspid insufficiency |
| Constrictive pericarditis |
| Inferior vena cava obstruction |
| Hepatic vein obstruction (Budd-Chiari syndrome) |
| Cardiomyopathy |
| Portal vein occlusion |
| Thrombosis |
| Tumor |
| Idiopathic tropical splenomegaly |
| Partial nodular transformation |
| Hypervitaminosis A |
| Fulminant hepatic failure |
| Idiopathic |
| Hypoalbuminemia |
| Cirrhosis |
| Nephrotic syndrome |
| Protein-losing enteropathy |
| Lymphangiectasia |
| Severe malnutrition |
| Miscellaneous |
| Myxedema |
| Hepatocellular carcinoma (usually with cirrhosis) |
| Ovarian disease |
| Tumor (Meigs' syndrome) |
| Struma ovarii |
| Ovarian overstimulation syndrome |
| Pancreatic ascites |
| Rupture of pseudocyst |
| Leak from pancreatic duct |
| Bile ascites |
| Gallbladder rupture |
| Traumatic bile leak |
| Chylous ascites |
| Rupture (traumatic, surgical) of abdominal lymphatics |
| Congenital lymphangiectasia |
| Obstructed lymphatics (especially secondary to malignancy, tuberculosis, filariasis) |
| Constrictive pericarditis |
| Cirrhosis |
| Sarcoidosis |
| With Peritoneal Disease: |
| Infection |
| Mycobacterial |
| Bacterial |
| Primary (spontaneous bacterial peritonitis in cirrhosis) |
| Secondary (ruptured viscus) |
| Fungal (rare, especially candidiasis, histoplasmosis, cryptococcosis) |
| Parasitic (rare, especially schistosomiasis, ascariasis, enterobiasis) |
| AIDS |
| Neoplasm |
| Primary mesothelioma |
| Metastatic carcinomatosis |
| Ovarian |
| Pancreatic |
| Gastric |
| Colonic |
| Lymphoma |
| Miscellaneous |
| Peritoneal vasculitides |
| Systemic lupus erythematosus |
| Henoch-Schönlein purpura |
| Köhlmeier-Degos disease |
| Eosinophilic peritonitis |
| Familial Mediterranean fever |
| Pseudomyxoma peritonei |
| Whipple's disease |
| Granulomatous peritonitis |
| Foreign bodies (especially starch) |
| Sarcoidosis |
| Gynecologic lesions (especially endometriosis, ruptured dermoid cyst) |
| Peritoneal lymphangiectasis |
The CT density of the pleural fluid is in our case 3 Hounsfield units suggesting transudate. The causes of pleural transudate can be also cardiac, renal, hepatic or due to thrmboembolic diseases (11).
Complications of renal lymphangiectasia can include haematuria, ascites, occasional renal venous thrombosis, deterioration in renal function and renin-dependent hypertension (2,6). Treatment is not usually necessary. Conservative treatment with diuretics and anti-hypertensives may be initiated for symptomatic patients (10). Complicated cases may be treated with nephrectomy (if unilateral), percutaneous drainage, or marsupialization (6).
TEACHING POINT
Renal lymphangiectasia is a rare disease and diagnosis is based primarily on the radiological findings of renal sinus cysts and aspiration of perinephric fluid collections. This case presents with pleural effusion in addition to ascites and perinephric fluid collections, which is a new finding of the disease and should be considered in the differential diagnosis of pleural effusion.
Table 2.
Differential diagnoses of pleural transudate.
| Cardiac disease |
| Congestive heart failure |
| Fluid overload |
| Constrictive pericarditis |
| Obstruction of superior vena cava or azygos vein |
| Renal disease |
| Nephrotic syndrome |
| Acute glomerulonephritis |
| Urinary tract obstruction |
| Peritoneal dialysis |
| Liver disease |
| Cirrhosis with ascites |
| Thromboembolic disease |
| Pulmonary embolism |
| Others |
| Meigs' syndrome |
| Myxedema |
| Sarcoidosis |
| Severe malnutrition (with hypoalbuminemia) |
| Iatrogenic (e.g., venous catheter in pleural space) |
| After lung transplantation |
ABBREVIATIONS
- mmHg
millimeter mercury
- mg dl−1
milligram per deciliter
- mEq l−1
milli-equivalent per liter
- cm
centimeter
- CT
computed tomography
- TB
tuberculosis
- ALP
Alkaline phosphatase
- SGPT
Serum Glutamic Pyruvate Transaminase
- SGOT
Serum Glutamic Oxaloacetic Transaminase
- IU
International unit
- IV
intravenous
REFERENCES
- 1.Meredith WT, Ahlstrom NG, Levine E, Grantham JJ. Exacerbation of familial renal lymphangiomatosis during pregnancy. Am J Roentgenol. 1988;151:965–6. doi: 10.2214/ajr.151.5.965. [DOI] [PubMed] [Google Scholar]
- 2.Schwarz A, Lenz T, Klaen R, Offermann G, Ulrich F, Nussberger J. Hygroma renale: pararenal lymphatic cysts associated with renin dependent hypertension (page kidney). Case report on bilateral cysts and successful therapy by marsupialization. J Urol. 1993;150:953–7. doi: 10.1016/s0022-5347(17)35660-4. [DOI] [PubMed] [Google Scholar]
- 3.Blumhagen JD, Wood BJ, Rosenbaum DM. Sonographic evaluation of abdominal lymphangiomas in children. J Ultrasound Med. 1987;6:487–495. doi: 10.7863/jum.1987.6.9.487. [DOI] [PubMed] [Google Scholar]
- 4.Kutcher R, Mahadevia P, Nussbaum MK, Rosenblatt R, Freed S. Renal peripelvic multicystic lymphangiectasia. Urology. 1987;30:177–179. doi: 10.1016/0090-4295(87)90191-9. [DOI] [PubMed] [Google Scholar]
- 5.Murray KK, McLellan GL. Renal peripelvic lymphangiectasia: appearance at CT. Radiology. 1991;180:455–456. doi: 10.1148/radiology.180.2.2068311. [DOI] [PubMed] [Google Scholar]
- 6.Riehl J, Schmitt H, Schafer L, Schneider B, Sieberth G. Retroperitoneal lymphangiectasia associated with bilateral renal vein thrombosis. Nephrol Dial Transplant. 1997;12:1701–3. doi: 10.1093/ndt/12.8.1701. [DOI] [PubMed] [Google Scholar]
- 7.Davidson AJ, Hartman DS. Lymphangioma of the retroperitoneum: CT and sonographic characteristics. Radiology. 1990;175:507–10. doi: 10.1148/radiology.175.2.2183287. [DOI] [PubMed] [Google Scholar]
- 8.Varela JR, Bargiela A, Requejo I, Fernandez R, Darriba M, Pombo F. Bilateral renal lymphangiomatosis: US and CT findings. Eur Radiol. 1998;8:230–231. doi: 10.1007/s003300050368. [DOI] [PubMed] [Google Scholar]
- 9.Ramseyer LT. Case 34: Renal lymphangiectasia. Radiology. 2001;219:442–4. doi: 10.1148/radiology.219.2.r01ma17442. [DOI] [PubMed] [Google Scholar]
- 10.Zakim D, Boyer TD. Hepatology. :764–788. [Google Scholar]
- 11.Connors AF, Altose MD. Pleural Disease. p. 1839. [Google Scholar]
- 12.Ashraf K, Raza SS, Ashraf O, Memon W, Memon A, Zubairi TA. Renal lymphangiectasia. Br J Radiol. 2007 Jun;80(954):e117–8. doi: 10.1259/bjr/16931054. [DOI] [PubMed] [Google Scholar]