Abstract
Background/Aims
Recent outbreak of hepatitis A in Korea is clearly related to the epidemiological shift of hepatitis A virus (HAV). However, nationwide seroprevalence data have been limited. This study estimated the nationwide, age- and area-adjusted anti-HAV prevalence from 2005 to 2009.
Methods
Retrospective analysis of the results of total anti-HAV test in 25,140 cases which were requested by 1,699 medical institutions throughout the nation to Seoul Clinical Laboratory from Jan. 1 2005 to Dec. 31 2009 was performed. The estimated seroprevalence was adjusted by area and age of the standard population based on the 2005 Census data from Korea National Statistical Office.
Results
The area-adjusted anti-HAV prevalence in the children younger than 10 years were 33.4% in 2005 and 69.9% in 2009. The most susceptible age groups to HAV infection during the last 5 years were teenagers and the young adults in their age of twenties. The area-adjusted seroprevalence in 2009 were 11.9% in the age group of 20-29 years, 23.4% in the age group of 10-19 years, 48.4% in the age group of 30-39 years. The population in 40-49 years showed geographically different seroprevalence with the lowest rate in Seoul (80%).
Conclusions
The most susceptible age group to HAV infection is 10-29 years, while the young children less than 10 years showed about 70% seropositivity. The changing seroepidemiology should be monitored continuously for the proper vaccination and patient care.
Keywords: Hepatitis A virus, Hepatitis A antibodies, Epidemiology, Prevalence, Korea
INTRODUCTION
Hepatitis A virus (HAV) causes around 80% of acute hepatitis in South Korea and its clinical manifestation is mild in children but is severe in many adults.1 The number of cases of hepatitis A reported to Korea Centers for Disease Control and Prevention increased sharply from 798, 2,081 and 2,233 in 2005, 2006 and 2007, respectively to 7,895 and 15,231 in 2008 and 2009, respectively.2 These are data from surveillance reporting system, while the numbers of claims actually made to National Health Insurance Cooperation are at least 3-4 times higher than them. However, this increase of symptomatic hepatitis in adults does not mean the increase of infection rate of HAV around the nation. Before 1990, most Koreans were infected with HAV before they were in their 20s and over 90% of the public already had protective antibodies in their 20s, so the incidence rate of symptomatic hepatitis A in adult population was low. With the improvement of the sanitary condition associated with the current economic development, the nationwide infection of HAV was reduced significantly while young adults and adolescents aged less than 40 years became more vulnerable to the infection because most of them do not have the protective antibody following natural infection. As the clinical manifestation of hepatitis A tends to be mild in children but severe in about 80% cases of adults, the cases of severe symptomatic hepatitis A are felt to be raised in recent years.
The current epidemic of hepatitis A was observed mainly in Seoul, Gyeonggi and Incheon and it spreads around the nation.1,3 Although the patients are usually in their 20s and 30s, the number of symptomatic hepatitis patients aged over 40s has been increasing these days. Epidemiological studies on the prevalence of hepatitis A antibody (anti-HAV) have been conducted continuously since the late 1990, but most of them investigated limited areas, had a small number of subjects or were performed for a short period and there have not been sufficient researches examining the nationwide antibody positive rates by year and age. Therefore, the authors analyzed the results of 45,296 hepatitis A antibody tests from Seoul Clinical Laboratories (SCL) requested by 1,699 medical institutions around the nation for the last five years, to determine total anti-HAV positive rates by year, age and area. Moreover, it obtained age- and area-adjusted anti-HAV positive rates with the population in 2005 Census as a standard population.
MATERIALS AND METHODS
Materials
This study examined the results of 45,296 cases for whom anti-HAV tests were requested to SCL by 1,699 medical institutions around the nation from January 2005 to December 2009. Out of them 20,156 patients took IgM anti-HAV test as well as total anti-HAV, and they were excluded in this study because they were considered to contain hepatitis A patients. So, the final subjects of this study were 25,140. The subjects gradually increased from 1,140 in 2005 to 14,101 in 2009, but the ratios of males and females were similar. Their mean age became higher from 31.0±20.4 years in 2005 to 38.4±14.9 years in 2009 (Table 1). This study was approved by Institutional Review Board of Seoul Medical Science Institute (SMSI).
Table 1.
Demographic characteristics of the subjects
Antibody test
Total anti-HAV test was conducted with electro-chemiluminescence immunoassay (ECLIA) by using Modular analytics E170 (Elecsys module, Roche Diagnostics GmbH, Manheim, Germany).
Statistical analysis
Anti-HAV positive rates of all age groups were investigated by dividing age at a five year interval. The data were primarily analyzed by area and year of test. The number of cases of the test was significantly higher in 2009 than in 2005 and the number of subjects living in the capital area was also higher than that in other areas. So, age- and area-adjusted positive rates by year were calculated with the population in 2005 Census as the standard population by classifying age at a 10-year interval and by arbitrarily dividing area into Seoul, Incheon/Gyeonggi/Gangwon, Chungcheong, Honam/Jeju and Gyeongsang. Using direct standardized method, all expected numbers of anti-HAV positive persons was calculated in the five areas and six age groups. For example, the expected number of anti-HAV positive persons in Seoul was obtained by adjusting the antibody positive rate of the subjects to the standard population of each age group and the sum of the expected numbers was divided by the sum of the standard population in Seoul. Statistical analysis was conducted with SPSS 15.0 and the positive rates by area and year were compared by using Pearson Chi-square test and Fischer's Exact test. A P-value of less than 0.05 was considered to be statistically significant.
RESULTS
Anti-HAV positive rate by area and year from 2005 to 2009
Although the total positive rates by year were examined by dividing age group at a 5-year interval from 2005 to 2009, it was hard to have accurate positive rates by age and area because of insufficient numbers of subjects by age and area. Therefore, the area was groups into 5 area districts and the age was classified at a 10-year interval for a direct standardization, to obtain standardized anti-HVA positive rate by age and year. The standardized rates showed a statistically significant difference compared to the previous year or the following year (P<0.001, Table 2). For age, the positive rate of young children aged less than 10 years increased sharply around the nation from 33.4% in 2005 to 69.9% in 2009. The age with the lowest positive rates from 2005 to 2009 was 10-29 years. The positive rate of the persons in their 10s went up slightly from 15.3% in 2005 to 23.4% in 2009 but that of the persons in their 20s was reduced from 23.1% in 2005 to 11.9% in 2009. The prevalence rates of the persons in their 30s and 40s tended to decline from 69.9% in 2005 to 48.4% in 2009 and from 97.9% in 2005 to 89.0% in 2009, respectively.
Table 2.
Area-adjusted anti-HAV seroprevalence rate (%) by year and age*
*Area was grouped as Seoul, Incheon+Gyeonggi+Gangwon, Chungcheong, Honam+Jeju, and Gyeongsang. 2005 Census population was used for standard population.
HAV, hepatitis A virus.
Changes of anti-HAV positive rates by area and age from 2005 to 2009
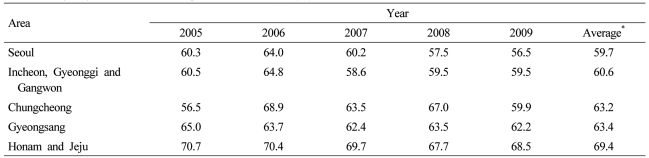
The antibody positive rates of the total subjects by year from 2005 to 2009 are shown in detail in Table 3. The rates of young children aged less than 10 years was only 16.7% in Seoul in 2005, but it skyrocketed to 73.3% in 2009. The rates of Incheon/Gyeonggi/Gangwon and Honam/Jeju also increased rapidly from 30.0% in 2005 to 69.9% in 2009 and from 37.8% in 2005 to 76% in 2009, respectively. Those of Chungcheong and Gyeongsang became higher from 44-43% in 2005 to 60-69% in 2009, respectively. The age with the lowest antibody positive rate in all areas in 2009 was 20s years by recording 10.4-13.3% and 10s years followed them by recording 17.8-30.1%. Interestingly, the rates of the persons in their 40s were reduced to 80% in Seoul and to 88.9-96.8% in other areas in 2009 compared to those in 2005. The positive rate of the persons in their 30s was 39-69.2%. All difference by area, year and age was statistically significant (P<0.001). The age-adjusted antibody positive rates by area are presented in Table 4. The rate in Seoul recorded the lowest level (59.7%) while the rate in Honam/Jeju showed the highest level (69.4%), and the difference by area was also statistically significant (P<0.001).
Table 3.
Age-specific anti-HAV seroprevalence rate (%) by area and year*
*P-values by Chi-square test for area, year and age were all < 0.001.
HAV, hepatitis A virus.
Table 4.
Age-adjusted anti-HAV seroprevalence rate (%) by year and area
*P-value by Chi-square test was<0.001.
HAV, hepatitis A virus.
DISCUSSION
This study investigated area- and age-adjusted anti-HAV positive rate from 2005 to 2009 by analyzing the results of totally 25,140 cases of anti-HAV test from one central laboratory requested by 1,699 medical institutions around the nation. Although the nationwide anti-HAV positive rates were not largely different from 62.5% in 2005 to 60.7% in 2009, the rates by area and age changed dynamically. The antibody positive rate of the young children aged less than 10 years increased sharply in the capital area for the recent five years, and the age which was the most vulnerable to hepatitis A infection was found to be 20s years with the seroprevalence rate of 11.9% which was followed by 10s years having the rate of 23.4%. The seropositive rates of the persons in their 30s and 40s were 48% and 89%, respectively, and particularly the rate of the persons in their 40s in Seoul was reduced to 80%.
In South Korea, anti-HAV positive rate had been over 50% in the persons in their 10s and it had reached nearly 100% in adults in the 1970s and the early 1980s, but it reduced remarkably from the 1990s by recording 54% in the personsaged 21-25 years in the late 1990s and 20-23% and 40-42% in the personsaged 10-24 years and 25-30 years, respectively in Seoul and Gyeonggi in the mid 2000s. The overall decrease of the antibody positive rate was found to move to older age.4-7 This tendency was observed in other countries such Spain, Greece and Israel.8-10 This epidemiological change could show a regional difference between urban and rural areas and the difference by income level was also reported. It was also found in developing countries including the Middle East, China and Central and South America and a study conducted in Bangladesh revealed that income level provoked the epidemiological difference.11-14 In South Korea, Song et al. reported that the anti-HAV positive rates of the persons in their 20s and 30s (25.6%) were significantly lower in Seoul than in other areas (55.6%) in 2007, but Kim et al. did not find any significance difference in the rate between Seoul and Gyeonggi in 2007.5,7 The study of Song et al. revealed that the positive rate of particularly Gangnam in Seoul was lower (20.0%) in the persons aged less than 40 years compared to the rate of other areas (55.6%). However, the number of the subjects in their study was not sufficient to compare the difference in the antibody positive rates by nationwide area and there has been no study on age- and area-adjusted rates based on Census in South Korea.5
The subjects of this study were 25,140 patients out of 45,296 for whom anti-HAV test were done by 1,699 medical institutions around the nation by excluding 20,156 ones for whom total anti-HAV test was requested along with IgM anti-HAV test because some of them could be acute hepatitis A patients. However, on what purposes the 25,140 subjects underwent total anti-HAV could not be defined, which was a limitation of this study. Medical institutions having asked SCL to conduct the antibody tests consist of hospitals or higher institutions in 55%, clinics in 30% and public health centers and others in 15%. As the cases of hepatitis A went up dramatically in 2008 and 2009, the public interest in the disease also increased to raise cases requesting the test by year.
This study calculated nationwide area- and age-adjusted hepatitis A antibody positive rates with 2005 Census, the latest population survey as a standard. However, the number of cases of the test by area and year was not sufficient to obtain standardized positive rates by administrative districts, so the whole nation was arbitrarily divided into five areas- Seoul, Incheon/Gyeonggi/Gangwon, Chungcheong, Gyeongsang and Honam/Jeju. As the antibody positive rate by gender was not significantly different in each age group and in each area, adjustment by gender was not applied. In addition, because this study examined the antibody positive rate of patients visiting hospitals rather than general population, their positive rate was likely to be lower than that of the general population and that can be a limitation of this study.
According to the result of this study, the antibody positive rate of the young children aged less than 10 years around the nation doubled from 33% in 2005 to 70% in 2009 and especially the increase was the largest in the capital area including Seoul. Vaccination against hepatitis A focusing on children had been conducted from 1997 and then the vaccination mainly for infants have been done. When the imported dose of hepatitis A vaccine for the last five years was examined, the vaccines for young children increased from 290,000 doses in 2005 to 400,000 doses in 2007, and 880,000 doses in 2009, while vaccine dose for adults were raised from 10,000 doses in 2006 to 20,000 in 2008 and 620,000 doses in 2009. Even though some vaccines for children were administered to adults due to the insufficient supply of vaccines for adults following the rapid increase of incidences hepatitis A in adults for the last three years, the numbers of vaccines for children are considered to show a continuous increase. Because children conventionally play an important role in the transmission of HAV and the vaccination for children reduced the adult cases of hepatitis A outstandingly in the U.S., Israel and Chile, it is considered that universal vaccination against hepatitis A for children should be recommended in South Korea.
The persons in their 10s and 20s were found to be the most vulnerable to the infection of HAV with the lowest antibody positive rates from 2005 to 2009. In 2009, the positive rate of the persons in their 20s recorded the lowest level (12%) and it was followed by that of the persons in their 10s (23%), which was not significantly different by area. In the meantime, although the total antibody positive rate of the persons in their 30s was 48%, the rates by area were different significantly (39%, 69% and 48% in Seoul, Honam/Jeju and other areas, respectively).
In particular, the positive rate of the persons in their 40s was lower in Seoul than in other areas. Therefore, even in persons in their early 40s living in the capital area becomes at risk of HAV infection although they have been thought to be relatively safe from the risk. The mortality rate of hepatitis A becomes higher at older age and the mortality rates of the persons in their 30s, 40s, 50s and 60s are estimated to be 0.04-0.06%, 0.03-0.1%, 0.08-0.23% and 0.58%, respectively.15 Moreover, Kim et al. reported that factors affecting the severity with 716 patients with hepatitis A were hepatitis B virus carriers, history of alcohol drinking and old age.16
In the U.S., around 200,000 cases of hepatitis A occurred to the mid 1990s and the cyclic epidemic with a cycle of 10-15 years, but an active vaccination for children from 1996 reduced its incidences considerably.17 However, in South Korea the vaccination rate against hepatitis A for children reaches 50-70%, which suggests the possibility of food-born transmission rather than children as a major source of infection. So, catch-up vaccination for the persons aged 10-29 years with a low antibody positive rate needs to be considered. The outstanding increase of vaccines for adults as well as those for children during recent years seems to be closely related with the decreased incidences of hepatitis A since 2010. Saab et al. insisted that if hepatitis A antibody positive rate was over 35% and anti-HAV test cost less than 25 U.S. dollars, vaccination without testing the antibody was cost-effective than vaccination after testing.18 Therefore, it is reasonable that persons aged less than 30 years undergo HAV vaccination without the antibody test while those aged over 30 years do after the test, but there have not been sufficient studies on the cost-effectiveness. Moreover, as this study found that the antibody positive rates were different by area and the seroprevalence rates of the persons in their 30s varied by area from 39% to 69%, the vaccination and the test should be conducted by considering the regional difference.
In conclusion, the hepatitis A antibody positive rate has changed rapidly in Korea for the last five years, and to prevent the nationwide spread of the hepatitis A, universal vaccination for children should be adapted and continuous monitoring and epidemiological studies are necessary.
Abbreviations
- HAV
hepatitis A virus
- M
male
- F
female
- SCL
Seoul Clinical Laboratories
- SMSI
Seoul Medical Science Institute
- ECLIA
electrochemiluminescence immunoassay
References
- 1.Kang CI, Choi CM, Park TS, Lee DJ, Oh MD, Choe KW. Incidence and seroprevalence of hepatitis A virus infections among young Korean soldiers. J Korean Med Sci. 2007;22:546–548. doi: 10.3346/jkms.2007.22.3.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim YJ, Lee HS. Increasing incidence of hepatitis A in Korean adults. Intervirology. 2010;53:10–14. doi: 10.1159/000252778. [DOI] [PubMed] [Google Scholar]
- 3.Lee TH, Kim SM, Lee GS, Im EH, Huh KC, Choi YW, et al. Clinical features of acute hepatitis A in the Western part of Daejeon and Chungnam province: single center experience. Korean J Gastroenterol. 2006;47:136–143. [PubMed] [Google Scholar]
- 4.Yeon JE, Kwon OS, Park SH, Byeon GS, Jo GH, An HS, et al. Seroepidemiologic study of hepatitis A virus infection in Korea [Abstract] Korean J Hepatol. 1999;5(Suppl 1):S4. [Google Scholar]
- 5.Song YB, Lee JH, Choi MS, Koh KC, Paik SW, Yoo BC, et al. The age-specific seroprevalence of hepatitis A virus antibody in Korea. Korean J Hepatol. 2007;13:27–33. [PubMed] [Google Scholar]
- 6.Hong WS, Kim CY. Seroepilemiology of type A and type B hepatitis in Seoul area. Korean J Intern Med. 1982;25:19–26. [Google Scholar]
- 7.Kim TY, Sohn JH, Ahn SB, Son BK, Lee HL, Eun CS, et al. Comparison of recent IgG anti-HAV prevalence between two hospitals in Seoul and Gyeonggi area. Korean J Hepatol. 2007;13:363–369. doi: 10.3350/kjhep.2007.13.3.363. [DOI] [PubMed] [Google Scholar]
- 8.Amela C, Pachón I, Bueno R, de Miguel C, Martinez-Navarro F. Trends in hepatitis A virus infection with reference to the process of urbanization in the greater Madrid area (Spain) Eur J Epidemiol. 1995;11:569–573. doi: 10.1007/BF01719310. [DOI] [PubMed] [Google Scholar]
- 9.Kremastinou J, Kalapothaki V, Trichopoulos D. The changing epidemiologic pattern of hepatitis A infection in urban Greece. Am J Epidemiol. 1984;120:703–706. doi: 10.1093/oxfordjournals.aje.a113937. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz E, Raveh D. The prevalence of hepatitis A antibodies among Israeli travellers and the economic feasibility of screening before vaccination. Int J Epidemiol. 1998;27:118–120. doi: 10.1093/ije/27.1.118. [DOI] [PubMed] [Google Scholar]
- 11.Barzaga BN. Hepatitis A shifting epidemiology in South-East Asia and China. Vaccine. 2000;18(Suppl 1):S61–S64. doi: 10.1016/s0264-410x(99)00467-3. [DOI] [PubMed] [Google Scholar]
- 12.Tufenkeji H. Hepatitis A shifting epidemiology in the Middle East and Africa. Vaccine. 2000;18(Suppl 1):S65–S67. doi: 10.1016/s0264-410x(99)00468-5. [DOI] [PubMed] [Google Scholar]
- 13.Tanaka J. Hepatitis A shifting epidemiology in Latin America. Vaccine. 2000;18(Suppl 1):S57–S60. doi: 10.1016/s0264-410x(99)00466-1. [DOI] [PubMed] [Google Scholar]
- 14.Saha SK, Saha S, Shakur S, Hanif M, Habib MA, Datta SK, et al. Community-based cross-sectional seroprevalence study of hepatitis A in Bangladesh. World J Gastroenterol. 2009;15:4932–4937. doi: 10.3748/wjg.15.4932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ki MR. Economic analysis of vaccination and development of guidelines for control of hepatitis A virus infection, and epidemiologic analysis and development of control strategy of hepatitis C virus infection. 2009. (Personal Communication)
- 16.Kim JI, Kim YS, Jung YK, Kwon OS, Kim YS, Ku YS, et al. Factors influencing the severity of acute viral hepatitis A. Korean J Hepatol. 2010;16:295–300. doi: 10.3350/kjhep.2010.16.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daniels D, Grytdal S, Wasley A. Centers for Disease Control and Prevention (CDC). Surveillance for acute viral hepatitis - United States, 2007. MMWR Surveill Summ. 2009;58:1–27. [PubMed] [Google Scholar]
- 18.Saab S, Martin P, Yee HF., Jr A simple cost-decision analysis model comparing two strategies for hepatitis A vaccination. Am J Med. 2000;109:241–244. doi: 10.1016/s0002-9343(00)00469-1. [DOI] [PubMed] [Google Scholar]