Abstract
Background/Aims
Cross-sectional studies have documented that 2-10% of patients who are chronically infected with hepatitis C virus (HCV) are also positive for hepatitis B virus (HBV) surface antigen (HBsAg). Data related to HCV-HBV coinfection are lacking in Korea. This study evaluated the clinical characteristics, the treatment efficacy of peginterferon alfa plus ribavirin, and the changes induced by such treatment in HBV status in chronic hepatitis C (CHC) patients coinfected with HBV.
Methods
Eighteen (2.37%) HBsAg-positive CHC patients were selected from among the 758 subjects from the K(G)yeonggi-Incheon Peginterferon alfa and ribavirin in chronic hepatitis C Treatment (KIPECT) study, which evaluated the treatment efficacy and safety of peginterferon alfa plus ribavirin in CHC patients. Data on changes in the status of HBV infections were obtained.
Results
HCV genotype 1b was the most common (44%). The overall sustained virologic response rate was 72% in all patients, and 60% and 87.5% in genotypes 1 and 2, respectively. Two of the 18 patients were positive for HBeAg, and 15 had baseline HBV DNA level of less than 2,000 IU/mL. Two of the three whose levels exceeded this threshold showed no detectable DNA after treatment. After the completion of treatment, serum HBV DNA levels were increased in the two patients whose baseline HBV DNA levels were less than 2,000 IU/mL.
Conclusions
The prevalence of HBV coinfection in CHC patients was 2.37% and most of the patients were inactive carriers. The treatment efficacy was similar to that of HCV mono-infection. Reactivation of HBV replication was observed in some patients after CHC treatment.
Keywords: Hepatitis B virus, Hepatitis C virus, Coinfection
INTRODUCTION
Hepatitis B virus (HBV) and hepatitis C virus (HCV) infection are the major causes of chronic liver disease worldwide and can lead to cirrhosis and hepatocellular carcinoma (HCC).1,2 Coinfection of these two hepatotropic virus is reported not to be rare. Studies from outside Korea reported that approximately 5-7% of HBV-infected patients also were positive for anti-HCV and 2-10% of chronic hepatitis C (CHC) patients were positive for hepatitis B surface antigen (HBsAg).3,4 In non-endemic areas, HBV and HCV coinfection is predominantly found in several high risk populations, such as intravenous drug users, patients on hemodialysis, recipients of organ transplantations, and human immunodeficiency virus positive patients.4 However, in endemic areas including Korea, the frequency of HBV infection provides the basis for an appreciable rate of HBV and HCV coinfection in the general population.3
Some cross-sectional studies reported that in comparison with monoinfection, HBV and HCV coinfection was associated with higher prevalence of liver cirrhosis and hepatic decompensation.5-7 Several studies also revealed that HBV and HCV coinfection increased the risk of developing HCC.8-10 With respect to the treatment response, there was a report suggesting that HBV coinfected CHC patients responded poorly to the treatment.11
There has been no research on coinfection of HBV and HCV in Korea, except for a report of 0.1% of anti-HCV seropositivity in HBsAg positive subjects in 2005.12 Therefore, no sufficient recommendation for the patients with HBV and HCV coinfection was provided by the current guideline.13
This retrospective, multicenter study aimed to investigate the prevalence of HBV and HCV coinfection in Korea, clinical and virologic characteristics, treatment efficacy of peginterferon and ribavirin combination therapy, and the change in the status of HBV infection following the treatment of CHC patients.
PATIENTS AND METHODS
Patients
HBsAg positive subjects were selected from the K(G)yeonggi-Incheon Peginterferon alfa and ribavirin Effect in Chronic hepatitis C Treatment (KIPECT) study which evaluated the treatment efficacy and safety of peginterferon plus ribavirin therapy in 758 CHC patients.14 A total of 18 HBsAg positive patients among the 758 subjects were retrospectively included from eight university hospitals. In KIPECT study, CHC patients with detectable serum HCV RNA and/or elevated serum alanine aminotransferase levels for more than 6 months, age ≥18 years, and treated with peginterferon alfa plus ribavirin from January 2000 to September 2008 were included. Exclusion criteria were acute hepatitis C patients, history of prior exposure to interferon or peginterferon, and no available data on genotype of HCV. The study protocol was approved by the Institutional Review Board of each hospital and was conducted in accordance with the principles of the Declaration of Helsinki.
Treatment of chronic hepatitis C
The study patients were treated with either pegylated interferon alfa-2a plus ribavirin or pegylated interferon alfa-2b plus ribavirin. Initial dosage and dose modification of the treatment drug was determined based on the current guideline suggested by the Korean Association for the Study of the Liver.15 Duration of the treatment was planned as 24 weeks for genotype 2/3 infection and 48 weeks for non genotype 2/3 infection.15
Data collection
Baseline clinical and virologic characteristics were obtained by retrospective review of medical records, and when available, histologic data before the treatment were also recorded. HCV RNA values measured in copies/mL were converted into IU/mL using conversion factor according to the used assay in each hospital.2 Serum HCV RNA levels were determined using the COBAS TaqMan HCV test (Roche Molecular System Inc., Branchburg, NJ, USA) in five institutes, Cobas Amplicor HCV Monitor V2.0 (Roche Molecular System Inc., Branchburg, NJ, USA), Abbott RealTime (Abott Diagnostics, Abbott Park, Illinois, USA), and Artus HCV RG RT-PCR Kit (Qiagen, Valencia, CA, USA) in one institute, respectively. Pre-and post-treatment hepatitis B e antigen (HBeAg), anti-hepatitis e antibody, HBV DNA values, and history of other treatment modalities used for HBV infection were recorded. Baseline histologic data concerning steatosis and fibrosis were collected. Hepatic steatosis was assessed as either presence or none, and the degree of hepatic fibrosis was classified as recommended by Korean Study Group for the Pathology of Digestive Disease: grade 0, no fibrosis; grade 1, portal fibrosis; grade 2, periportal fibrosis; grade 3, septal fibrosis; grade 4, cirrhosis.16 Data collection was performed using an case record form in the charge of doctors in the individual hospital from April 2009 to December 2009.
Definition and evaluation of the treatment response of CHC
The early virologic response (EVR), end of treatment response (ETR) and sustained virologic response (SVR) were used to investigate the treatment response of CHC proposed by The Korean association for the study of the liver.15 Quantitative HCV RNA values were recorded which were determined at baseline, at 12 week after the treatment, and at the time of the treatment termination for HCV of genotype 1. Based on the level of HCV RNA value at 12 week, the presence of EVR was judged as either complete (HCV RNA negative) or partial (reduction in HCV RNA level more than 2 log compared to baseline HCV RNA level). For CHC patients infected with genotype 2/3 HCV, quantitative HCV RNA levels of baseline and at the time of treatment termination were recorded. Regardless of genotype, ETR was defined as HCV RNA negativity at the end of treatment. SVR was defined as HCV RNA negativity measured at 24 weeks after cessation of treatment in all genotype.
Statistical analysis
The mean±standard deviation (SD) was used to describe continuous variables and categorical variables were presented as the number with a percent. Comparison of continuous variables was performed with a student's t-test and Fisher's exact test was used to compare categorical variables. P-values less than 0.05 were considered to be statistically significant. All data were analyzed using SPSS (version 15.0; Chicago, IL, USA).
RESULTS
Demographics and baseline characteristics
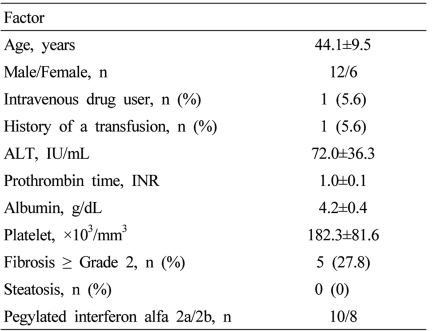
Eighteen out of 758 CHC patients in the KIPECT study were positive for HBsAg. The prevalence of HBV-HCV coinfection was 2.37%. The mean age of the subjects was 44.1 years and males constituted 66% of the total. When categorized by the age in detail, 1 patient (5.6%) was younger than 30 years, 5 patients (27.8%) were between 30 and 40 years, 8 patients (44.4%) were between 40 and 50 years, and 4 patients (22.2%) were older than 50 years. One patient had a history of intravenous drug use and another patient had a history of transfusion. None were coinfected with human immunodeficiency virus. Histologic data was available in 5 patients and all had fibrosis of stage 2 and no steatosis. There was no patient with clinical or histologic evidences of liver cirrhosis. Other detailed baseline characteristics of the study subjects are presented in Table 1.
Table 1.
Baseline demographics and clinical characteristics
Data represent mean±SD or number (%).
ALT, alanine aminotransferase.
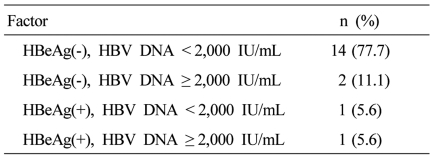
Baseline status of coinfection with HBV and HCV
Genotype 1b was found in eight patients (44%) and was the most common HCV genotype. Genotype 2a/c was present in 5 (28%) and was the second most common. Genotype 2 unclassified and 1a was seen in 3 (17%) and 2 (11%) patients, respectively. Mean value of baseline HCV RNA was 8.79×106±1.45×107 IU/mL and 11 patients (61.1%) had HCV RNA level more than 600,000 IU/mL. Sixteen of the 18 patients (88.8%) were negative for HBeAg and 15 (83.3%) patients had HBV DNA level less than 2,000 IU/mL. Other data concerning HBV infection are detailed in Table 2. Serum HCV RNA levels were compared between patients with and without detectable serum HBV DNA. HCV RNA level was 4.9×106±6.7×106 IU/mL in patients with detectable HBV DNA and 1.6×107±2.1×107 IU/mL in patients without detectable DNA, although there was no statistical significance (P=0.257). HCV RNA levels were also compared according to HBeAg status. It was 2.4×107±2.7×107 IU/mL in HBeAg positive patients and 5.7×107±8.4×107 IU/mL in HBeAg negative patients (P=0.367). The proportion of CHC patients with high viral load (HCV RNA > 600,000 IU/mL) was not significantly different according to detectable serum HBV DNA (P=1.000) and HBeAg status (P=1.000).
Table 2.
Baseline data of HBV infection in the CHC patients
HBV, hepatitis B virus; CHC, chronic hepatitis C; HBeAg, hepatitis B virus e antigen; SD, standard deviation.
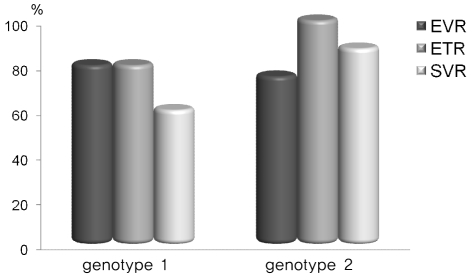
Treatment efficacy of peginterferon alfa plus ribavirin in chronic hepatitis C
Overall, fourteen out of the 18 patients (77.8%) showed EVR and 16 patients (88.9%) had ETR. Thirteen patients showed SVR (72.2%) regardless of the genotype. Treatment responses according to HCV genotype are presented in Figure 1. The SVR rate was 60% in genotype 1 and 87.5% in genotype 2 (Fig. 1).
Figure 1.
Treatment responses according to HCV genotype. In genotype 1 (n=10), the rates of EVR (early virologic response), ETR (end of treatment response), and SVR (sustained virologic response) were 80%, 80%, and 60%, respectively; the corresponding rates in genotype 2 (n=8), were 75%, 100%, and 87.5%.
Changes in hepatitis B virus after treatment of chronic hepatitis C
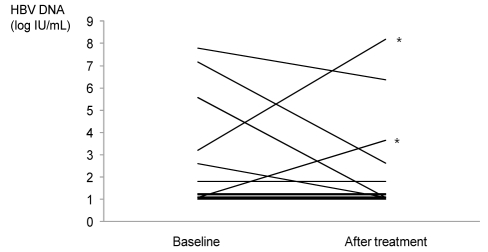
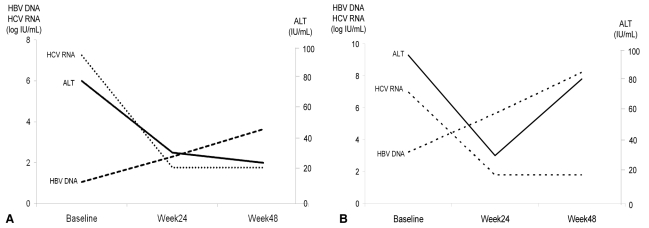
Peginterferon alfa is also approved for the treatment of CHB.13 In this study, no one developed seroclearance or seroconversion of HBsAg or HBeAg after the completion of treatment. Post-treatment HBV DNA values were available in 16 patients. The change of serum HBV DNA levels before and after treatment of CHC is presented in Figure 2. Three patients had a baseline HBV DNA value exceeding 2,000 IU/mL and HBV DNA was undetectable in 2 of these 3 patients after the treatment. Two of the 3 patients with a baseline HBV DNA level under 2,000 IU/mL exhibited increase of HBV DNA level more than 1 log from the baseline. A 44-year-old male patient with genotype 1b infection had undetectable baseline HBV DNA (limit of detection 12 IU/mL) and was negative for HBeAg before treatment of CHC. Serum HCV RNA level was 9,340,000 IU/mL at baseline. He achieved ETR and subsequently showed SVR after the treatment with peginterferon plus ribavirin for 48 weeks, however, serum HBV DNA was increased to 4,444 IU/mL. Biochemical breakthrough or reversion of HBeAg was not observed and no additional therapy for HBV infection was administered. The clinical course of another patient who developed flare-up of CHB is presented in detail (Fig. 3A). A 38-year-old man infected with HCV genotype 1b additionally received entecavir for HBV infection after treatment of CHC. Baseline HBeAg was positive and serum HBV DNA was 1,552 IU/mL. After the 48 week treatment of peginterferon plus ribavirin, serum aspartate aminotransferase and alanine aminotransferase levels were elevated with achievement of the ETR. When other potential etiologies of acute hepatitis were surveyed, it was absent. Serum HBV DNA level increased to 153,844,063 IU/mL and 0.5 mg/day of entecavir was prescribed to manage flare-up of CHB. HCV RNA was positive at 24 weeks after the treatment and SVR was not observed in this patient (Fig. 3B).
Figure 2.
Changes in HBV DNA level after CHC treatment. Two of the 13 patients whose baseline HBV DNA was <2,000 IU/mL developed viral replication after HCV treatment (marked as*), while the HBV DNA levels of the other patients remained stable. Two of the three patients with baseline HBV DNA levels >2,000 IU/mL had no detectable HBV DNA at the end of treatment.
Figure 3.
Clinical courses of the patients who developed flare-up of CHB after CHC treatment. (A) Serum HBV DNA level was increased after treatment of HCV infection in a 44-year-old man without breakthrough hepatitis. (B) The serum HBV DNA level was increased in a 38-year-old man after treatment with accompanying flare-up hepatitis.
DISCUSSION
HBV and HCV share many risk factors for infection, thus coinfection with both viruses is not uncommon.3 However, the worldwide prevalence of coinfection with HBV and HCV is unknown due to lack of large-scale population-based studies.4 Furthermore, since is scant information on the treatment of HBV and HCV coinfection, the current guidelines cannot suggest specific approved treatment for this patient group.1,13
Data from outside of Korea reported that 2-10% of CHC patients are also HBsAg positive.4 In areas where HBV infection is endemic, like in Korea, a substantial number of patients are infected with both viruses.17-19 Even though Korea is a representative endemic area of HBV infection, there has hitherto been no systemic study about HBV and HCV coinfection. A study that surveyed serologic markers of various viral hepatitis and reviewed the prevalence of concurrent infection reported that seven of 5131 HBsAg positive subjects (approximately 0.1%) were also positive for anti-HCV in 2005.12 To date, this was the only study that investigated HBV and HCV coinfection in Korea. This study was hampered by the lack of detailed clinical or virologic information. It is remarkable that this current study is the first report of HBV and HCV coinfection in the Korean population and the prevalence of HBV coinfection in CHC patients was 2.37%.
Certain high risk patients, such as intravenous drug users, patients on hemodialysis, patients with human immunodeficiency virus infection, and recipients of organ transplants are frequently coinfected with HBV and HCV.4 In areas of high prevalence of HBV infection, HCV superinfection in individuals with CHB is the most common scenario of HBV and HCV coinfection.20 In this study, only one CHC patient had a history of intravenous drug use, which may reflect some difference in the epidemiology between other countries. However, due to the retrospective nature of this study, there is a possibility of underestimation of such risk factors for coinfection.
Dual or triple hepatitis virus infections are associated with viral interference.18 Clinical and laboratory studies have shown that HBV and HCV interact with each other and that generally HCV exerts a suppressive effect on HBV.4,18 This has been corroborated by reports that described the occurrence of HBeAg seroconversion and HBsAg seroclearance in HCV superinfected CHB patients.20,21 In our study, 88% of the study subjects were negative for HBeAg, and 83% had HBV DNA <2,000 IU/mL, which provides additional evidence for the suppression of HBV replication by HCV. Although no statistical significances were observed, HCV RNA was measured to be higher in HBeAg positive patients than that of negative patients. HCV RNA was also higher and in patients without detectable serum HBV DNA. These finding can be another evidence of suppressive effect of HCV on HBV. While the inhibitory effect of HCV was observed only in genotype 1 HCV infection in one study,4 it was impossible to prove this association in our study because of the small number of patients.
Combination of peginterferon alfa and ribavirin is now recommended as the standard treatment for chronic HCV monoinfection.2 Since very limited data regarding therapy of HBV and HCV coinfected patients are available, there are currently no established treatment guidelines for these patients.4 Although one small study reported that neither peginterferon nor conventional interferon based regimens were effective for HBV coinfected CHC,11 a recent large randomized prospective trial from Taiwan showed that the combination therapy with peginterferon plus ribavirin was equally effective in patients with HCV monoinfection and in those with HBV and HCV coinfection.22 Another study from China concluded that, when compared with HCV monoinfected patients, the SVR rate was similar, but relapse rate of patients with HCV genotype 1 infection in the coinfection group was high.23 In our study, the overall SVR rate regardless of HCV genotype was 72.2%, and patients with HCV genotype 1 and 2 showed a SVR rate of 60% and 87.5%, respectively. When considering the reported treatment outcomes in Korea, an overall SVR rate of 59.6-82.8%, SVR rate of 53.6% to 69.6% in genotype 1 and genotype 4, and SVR rate of 71.4% to 90.2% in genotype 2 and 3,14,24-27 it seems to be indicative of similar treatment response rates in HBV coinfected CHC patients compared to patients with HCV monoinfection.
Previous studies have indicated that successful clearance of HCV may lead to reactivation of HBV in approximately one-third of patients.22-24 In this study, HBV DNA levels were increased after treatment of CHC in two of 13 patients (15%) whose baseline HBV DNA was <2,000 IU/mL. Although increase of HBV DNA did not result in flare-up hepatitis in one patient, biochemical breakthrough occurred in another patient and antiviral therapy against HBV was subsequently administered to manage CHB. So, while treating HBV coinfected CHC patients, the possibility of HBV reactivation should be considered even in the inactive carrier of HBV, and HBV DNA level should be carefully followed up.
Several studies have compared the histologic findings between HBV and HCV coinfection with HCV monoinfection, and concluded that liver injury or fibrosis are more severe in coinfection.6,22,28 In this study, data on histology was available in only 5 patients and none of them had advanced fibrosis. Unfortunately, due to the small number of sample size, the severity of fibrosis in HBV and HCV coinfected patients could not be evaluated in this study. There have also been several case-control studies showing an increased risk of developing HCC in coinfected patients.5-8 A meta-analysis conducted to evaluate the impact of HBV and HCV coinfection on the development of HCC demonstrated the significantly higher relative risk of HCC in coinfected patients (odds ratio=165) than HBV (odds ratio=22.5) or HCV (odds ratio=17.3) monoinfection.29 In general, patients with HCC or decompensated cirrhosis are not considered as a candidate for interferon based therapy. Because this study only included CHC patients treated with peginterferon plus ribavirin, there is a possibility that most of the patients with history of HCC or advanced cirrhosis might have been excluded. Therefore, evaluation about development of HCC or advanced cirrhosis in HBV and HCV coinfected patients is considered to be impossible in this study subjects and it is an area of further research.
This study has some limitations. First, the prevalence rate of HBV and HCV coinfection of 2.37% was much lower than reported data of 2-10%,4 and there is a possibility of underestimation. We only included candidates of HCV treatment, patients with detectable HCV RNA in blood. Moreover, the proportion of CHC patients who do not require treatment due to various reasons are not considered in this study. Secondly, possible occult HBV infection was not considered. Occult HBV infection has frequently been identified in patients with HCV infection, and the prevalence has been recorded as high as 48.9%.30,31 The retrospective design involving a relatively small number of subjects is acknowledged drawback. Because the present study had a short follow-up period, the long-term consequence of coinfection including the development of cirrhosis or HCC could not be evaluated. Further prospective research for long-term prognosis of HBV and HCV coinfection is required. Nevertheless, it is meaningful in that this is the first study to survey HBV and HCV coinfection in Korea, and paves the way for more comprehensive studies. Further large, multicenter, prospective studies are necessary to investigate accurate epidemiology, viral characteristics, and long term prognosis of HBV and HCV coinfection regarding the development of viral relapse, cirrhosis, and HCC. It also will be helpful to Korean guideline by collecting data from Korean population. Also, more studies are necessary to determine the optimal treatment regimen, especially to prevent HBV reactivation or elucidate the possible additional role of potent oral nucleotide/nucleoside analogues in HBV and HCV coinfected patients.
In summary, the prevalence of HBV coinfection in CHC patients was 2.37%, most of the coinfected patients had low levels of HBV DNA, and were inactive carriers. Treatment efficacy of peginterferon alfa and ribavirin combination for the coinfected patients was quite similar to patients with HCV monoinfection. After treatment of CHC and viral suppression of HCV, some patients were prone to reactivation of HBV replication.
Acknowledgements
This study was supported by The Korean Association for the Study of the Liver in 2009.
Abbreviations
- CHB
chronic hepatitis B
- CHC
chronic hepatitis C
- ETR
end of treatment response
- EVR
early virological response
- HBeAg
hepatitis B e antigen
- HBsAg
hepatitis B surface antigen
- HBV
hepatitis B virus
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- KIPECT
K(G)yeonggi-Incheon Peginterferon alfa and ribavirin Effect in Chronic hepatitis C Treatment
- SVR
sustained virologic response
References
- 1.Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–662. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 2.Ghany MG, Strader DB, Thomas DL, Seeff LB American Association for the Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335–1374. doi: 10.1002/hep.22759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peters MG. Special populations with hepatitis B virus infection. Hepatology. 2009;49(5 Suppl):S146–S155. doi: 10.1002/hep.22965. [DOI] [PubMed] [Google Scholar]
- 4.Chu CJ, Lee SD. Hepatitis B virus/hepatitis C virus coinfection: epidemiology, clinical features, viral interactions and treatment. J Gastroenterol Hepatol. 2008;23:512–520. doi: 10.1111/j.1440-1746.2008.05384.x. [DOI] [PubMed] [Google Scholar]
- 5.Mohamed Ael S, al Karawi MA, Mesa GA. Dual infection with hepatitis C and B viruses: clinical and histological study in Saudi patients. Hepatogastroenterology. 1997;44:1404–1406. [PubMed] [Google Scholar]
- 6.Zarski JP, Bohn B, Bastie A, Pawlotsky JM, Baud M, Bost-Bezeaux F, et al. Characteristics of patients with dual infection by hepatitis B and C viruses. J Hepatol. 1998;28:27–33. doi: 10.1016/s0168-8278(98)80198-0. [DOI] [PubMed] [Google Scholar]
- 7.Fong TL, Di Bisceglie AM, Waggoner JG, Banks SM, Hoofnagle JH. The significance of antibody to hepatitis C virus in patients with chronic hepatitis B. Hepatology. 1991;14:64–67. doi: 10.1002/hep.1840140111. [DOI] [PubMed] [Google Scholar]
- 8.Kirk GD, Lesi OA, Mendy M, Akano AO, Sam O, Goedert JJ, et al. The Gambia Liver Cancer Study: Infection with hepatitis B and C and the risk of hepatocellular carcinoma in West Africa. Hepatology. 2004;39:211–219. doi: 10.1002/hep.20027. [DOI] [PubMed] [Google Scholar]
- 9.Benvegnù L, Fattovich G, Noventa F, Tremolada F, Chemello L, Cecchetto A, et al. Concurrent hepatitis B and C virus infection and risk of hepatocellular carcinoma in cirrhosis. A prospective study. Cancer. 1994;74:2442–2448. doi: 10.1002/1097-0142(19941101)74:9<2442::aid-cncr2820740909>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 10.Chiaramonte M, Stroffolini T, Vian A, Stazi MA, Floreani A, Lorenzoni U, et al. Rate of incidence of hepatocellular carcinoma in patients with compensated viral cirrhosis. Cancer. 1999;85:2132–2137. [PubMed] [Google Scholar]
- 11.Senturk H, Tahan V, Canbakan B, Uraz S, Ulger Y, Ozaras R, et al. Chronic hepatitis C responds poorly to combination therapy in chronic hepatis B carriers. Neth J Med. 2008;66:191–195. [PubMed] [Google Scholar]
- 12.Lee G, Kim KH, Kwon JA, Yoon SY, Cho Y, Lee CK, et al. Serologic markers of viral hepatitis of Korea University medical center patients. Korean J Lab Med. 2005;25:61–65. [Google Scholar]
- 13.Lee KS, Kim DJ Korean Association for the Study of the Liver Guideline Committee. Management of chronic hepatitis B. Korean J Hepatol. 2007;13:447–488. doi: 10.3350/kjhep.2007.13.4.447. [DOI] [PubMed] [Google Scholar]
- 14.Park SH, Park CK, Lee JW, Kim YS, Jeong SH, Kim YS, et al. Efficacy and tolerability of peginterferon alfa plus ribavirin in the routine daily treatment of chronic hepatitis C patients in Korea; a multi-center, retrospective, observational study. Korean J Hepatol. 2010;16(suppl 3):S58. [Abstract] [Google Scholar]
- 15.The Korean Association for The Study of The Liver. Treatment guidelines for chronic hepatitis C 2004. Korean J Hepatol. 2004;10(suppl 6):S101–S125. [Google Scholar]
- 16.Yu E Korean Study Group for the Pathology of Digestive Diseases. Histologic grading and staging of chronic hepatitis: on the basis of standardized guideline proposed by the Korean Study Group for the Pathology of Digestive Diseases. Korean J Hepatol. 2003;9:42–46. [PubMed] [Google Scholar]
- 17.Chen DS, Kuo GC, Sung JL, Lai MY, Sheu JC, Chen PJ, et al. Hepatitis C virus infection in an area hyperendemic for hepatitis B and chronic liver disease: the Taiwan experience. J Infect Dis. 1990;162:817–822. doi: 10.1093/infdis/162.4.817. [DOI] [PubMed] [Google Scholar]
- 18.Liaw YF. Role of hepatitis C virus in dual and triple hepatitis virus infection. Hepatology. 1995;22:1101–1108. doi: 10.1016/0270-9139(95)90615-0. [DOI] [PubMed] [Google Scholar]
- 19.Liu CJ, Liou JM, Chen DS, Chen PJ. Natural course and treatment of dual hepatitis B virus and hepatitis C virus infections. J Formos Med Assoc. 2005;104:783–791. [PubMed] [Google Scholar]
- 20.Liaw YF, Chen YC, Sheen IS, Chien RN, Yeh CT, Chu CM. Impact of acute hepatitis C virus superinfection in patients with chronic hepatitis B virus infection. Gastroenterology. 2004;126:1024–1029. doi: 10.1053/j.gastro.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Liaw YF, Lin SM, Sheen IS, Chu CM. Acute hepatitis C virus superinfection followed by spontaneous HBeAg seroconversion and HBsAg elimination. Infection. 1991;19:250–251. doi: 10.1007/BF01644957. [DOI] [PubMed] [Google Scholar]
- 22.Liu CJ, Chuang WL, Lee CM, Yu ML, Lu SN, Wu SS, et al. Peginterferon alfa-2a plus ribavirin for the treatment of dual chronic infection with hepatitis B and C viruses. Gastroenterology. 2009;136:496–504. doi: 10.1053/j.gastro.2008.10.049. [DOI] [PubMed] [Google Scholar]
- 23.Yu JW, Sun LJ, Zhao YH, Kang P, Gao J, Li SC. Analysis of the efficacy of treatment with peginterferon alpha-2a and ribavirin in patients coinfected with hepatitis B virus and hepatitis C virus. Liver Int. 2009;29:1485–1493. doi: 10.1111/j.1478-3231.2009.02080.x. [DOI] [PubMed] [Google Scholar]
- 24.Gordon SC, Sherman KE. Treatment of HBV/HCV coinfection: releasing the enemy within. Gastroenterology. 2009;136:393–396. doi: 10.1053/j.gastro.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 25.Kim KT, Han SY, Kim JH, Yoon HA, Baek YH, Kim MJ, et al. Clinical outcome of pegylated interferon and ribavirin therapy for chronic hepatitis C. Korean J Hepatol. 2008;14:36–45. doi: 10.3350/kjhep.2008.14.1.36. [DOI] [PubMed] [Google Scholar]
- 26.Lee H, Choi MS, Paik SW, Kim JH, Kim DY, Lee JH, et al. Peginterferon alfa-2a plus ribavirin for initial treatment of chronic hepatitis C in Korea. Korean J Hepatol. 2006;12:31–40. [PubMed] [Google Scholar]
- 27.Kang MJ, Jung EU, Park SW, Choi P, Kim JH, Park SJ, et al. Effects of pegylated interferon and ribavirin in Korean patients with chronic hepatitis C virus infection. Korean J Hepatol. 2008;14:318–330. doi: 10.3350/kjhep.2008.14.3.318. [DOI] [PubMed] [Google Scholar]
- 28.Lee LP, Dai CY, Chuang WL, Chang WY, Hou NJ, Hsieh MY, et al. Comparison of liver histopathology between chronic hepatitis C patients and chronic hepatitis B and C-coinfected patients. J Gastroenterol Hepatol. 2007;22:515–517. doi: 10.1111/j.1440-1746.2006.04547.x. [DOI] [PubMed] [Google Scholar]
- 29.Donato F, Boffetta P, Puoti M. A meta-analysis of epidemiological studies on the combined effect of hepatitis B and C virus infections in causing hepatocellular carcinoma. Int J Cancer. 1998;75:347–354. doi: 10.1002/(sici)1097-0215(19980130)75:3<347::aid-ijc4>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 30.Cacciola I, Pollicino T, Squadrito G, Cerenzia G, Orlando ME, Raimondo G. Occult hepatitis B virus infection in patients with chronic hepatitis C liver disease. N Engl J Med. 1999;341:22–26. doi: 10.1056/NEJM199907013410104. [DOI] [PubMed] [Google Scholar]
- 31.Fukuda R, Ishimura N, Hamamoto S, Moritani M, Uchida Y, Ishihara S, et al. Co-infection by serologically-silent hepatitis B virus may contribute to poor interferon response in patients with chronic hepatitis C by down-regulation of type-I interferon receptor gene expression in the liver. J Med Virol. 2001;63:220–227. doi: 10.1002/1096-9071(200103)63:3<220::aid-jmv1004>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]