Abstract
The increasing prevalence of obesity has become one of the most challenging problems facing healthcare providers. Despite recommendations from the U.S. Preventive Services Task Force many health professionals fail to discuss obesity with their patients. This study sought to identify terms that individuals with obesity and being treated in primary care find the most and least acceptable for describing their excess weight. Three-hundred ninety obese adult primary care patients in the Philadelphia area were administered the Weight Preferences Questionnaire from January 2008 through February 2009. Ratings of 11 terms used to describe excess weight were transformed to a five-point scale, ranging from “very desirable” (+2) to neutral (0) to “very undesirable” (-2). The term “fatness” (mean score -1.1 ± 1.3) was rated as significantly more undesirable than all other descriptors (p < 0.001). The terms “excess fat” (-0.6 ± 1.3), “large size” (-0.6 ± 1.3), “obesity” (-0.5 ± 1.4), and “heaviness” (-0.4 ± 1.2) were rated as significantly more undesirable then the remaining terms, which included weight problem, body mass index (BMI), and excess weight (p<0.001). In contrast, the term “weight” was viewed as the most desirable term for characterizing excess weight. Patients' preferences for terms were not significantly influenced by gender, race/ethnicity, or a BMI ≥ 40 kg/m2. Practitioners who treat obesity are encouraged to avoid undesirable terms when discussing this condition with their patients. Instead practitioners may want to consider broaching the topic using more patient-friendly term such as “weight,” “BMI,” “weight problem,” or excess weight.”
Keywords: obesity, preferred terms
Introduction
Broaching the topic of obesity can be difficult for health care providers, because weight is a sensitive issue. When used by the public, terms such as “obese” and “fat” often carry negative, demeaning social connotations (1,2). The term “obesity” also is perceived to have negative connotations when used by health care providers to discuss patients' excess weight (3,4). Obese individuals' dislike of terms including “obesity,” “fatness,” and “heaviness” was revealed by a pilot study conducted at a tertiary academic medical center that specialized in weight management (5).
The present study assessed attitudes towards terms to describe excess weight in obese individuals in primary care practice, prior to their participating in a weight loss research study, conducted by their own primary care providers (PCPs). We predicted that these individuals would rate the terms “obesity” and “fatness” as undesirable for describing their excess weight, similar to the patients surveyed in our obesity-specialty clinic, and that they would prefer descriptors such as “weight” or “body mass index.” In addition, we hypothesized that patients with a BMI ≥ 40 kg/m2, who potentially would be more ready to acknowledge their excess weight, would not rate the terms “obesity” and “fatness” as undesirable as individuals with a BMI < 40 kg/m2. We also evaluated whether preferred terms for describing weight would vary based on gender or race/ethnicity. We predicted that men would not rate the terms “obesity” and “fatness” as undesirable as women would. No predictions were made about the effects of race/ethnicity.
Methods
Participants
Study participants were enrolled in the Practice-Based Opportunities for Weight Reduction (POWER) trial, the goals of which have been described previously (6,7). Briefly, this 2-year, randomized controlled trial was designed to enlist both PCPs and auxiliary healthcare staff to improve weight loss in primary care practice. The 390 study participants were patients at six primary care practices in the Philadelphia area that are owned by the University of Pennsylvania Health System. Persons were eligible to participate if they were ≥ 21 yr and had a BMI of 30-50 kg/m², an increased waist circumference (≥ 40 in for men and > 35 in for women), and at least one of the four other criteria for metabolic syndrome (8).
Procedures
Participants at each of the six sites were referred to study coordinators by PCPs but also could refer themselves in response to brochures distributed in the practices. Baseline data, including physical measures and information about participants' preferred terms for describing excess weight, were collected at the randomization visit. Recruitment began in January 2008 and concluded in February 2009. The study's protocol was approved by the Institutional Review Board at the University of Pennsylvania, and all participants provided written informed consent.
Outcome Measures
Weight, height, and demographic information
Weight was measured on a digital scale (Tanita BWB 800, Tanita Corp, Tokyo, Japan), with participants dressed in light clothing, without shoes. Height was measured using a mounted stadiometer (Seca Stadiometer 202, Seca, Hamburg, Germany). Participants self-reported their age, race/ethnicity, and education.
Weight Preferences Questionnaire
Prior to treatment, participants completed the Weight Preferences Questionnaire (5), which instructed them to: “Imagine that you are visiting your doctor for a check-up. The nurse has measured your weight and found that you are at least 50 lb over your recommended weight. The doctor will be in shortly to speak with you. Doctors can use different terms to describe weight. Please indicate how desirable or undesirable you would find each of the following terms if your doctor used it.”
Participants used a 5-point, Likert-type scale (i.e., 1 = very desirable, 2 = desirable, 3 = neutral, 4 = undesirable and 5 = very undesirable) to rate each of 11 terms that was introduced by the phrase: “Good morning. I want to talk with you about your:” 1) weight; 2) heaviness; 3) obesity; 4) BMI; 5) excess weight; 6) fatness; 7) excess fat; 8) large size; 9) unhealthy body weight; 10) weight problem; and 11) unhealthy BMI. As described previously (5), the terms were generated from discussions with several obese patients in our clinic, in response to open-ended questions. These terms were reviewed for content validity by the authors. Same-day test-retest reliability coefficients for the 11 items, as assessed in 30 obese volunteers, ranged from .70 (“weight problem”) to .93 (“fatness”), with five coefficients > .80.
In the present study, the terms were presented to half the participants in the order listed above and in reverse order to the other half. Two supplementary open-ended questions also were added. They read: “Please indicate the two terms you would most want your doctor to use,” and “the two terms you would least want your doctor to use.” Participants were instructed that their response to the open-ended questions was not limited to the terms listed and they were free to write in desirable or undesirable terms for describing excess weight.
Statistical Analysis
Summary statistics for continuous and categorical variables were examined for range and to assess plausibility of values. All data were assessed for normality prior to analysis. Ratings of terms to describe excess weight were transformed to a +2 (“very desirable”) to -2 (“very undesirable”) scale, with a score of 0 representing “neutral.” A single analysis of variance (ANOVA) incorporating all participants was used to determine whether the ratings of any of the terms differed from each other. A post-hoc analysis was performed using Tukey's studentized range test to identify statistically significant differences between pairs of terms. The criterion for significance between terms was set at p = 0.05. A multivariate analysis of variance (MANOVA) was performed to determine whether ratings of terms differed by BMI group (≥ 40 vs < 40 kg/m2), gender, or race/ethnicity (non-Hispanic white vs African American). Preliminary analyses showed that the ratings of preferred terms were not significantly affected by the order of presentation (i.e., when the choice of terms was listed in reverse order) and, thus, the data were collapsed together. All analyses were conducted using SPSS (version 15.0, 2006, SPSS Inc, Chicago, IL).
Results
Participants' Characteristics
Participants had a mean age of 51.5 ± 11.5 yr, weight of 107.7 ± 18.3 kg, and body mass index of 38.5 ± 4.7 kg/m2. Eighty percent of participants were women; 59% were non-Hispanic white, 38.5% African-American, and 4.6% were Hispanic-American (see Table 1). Nearly 95% had the equivalent of a high school degree, and 38% had a bachelor's degree or higher.
Table 1. Participants' baseline characteristics.
| N=390 | Female (n=311) |
Male (n=79) |
|
|---|---|---|---|
| Age, years | 51.5 (11.5) | 51.4 (11.8) | 51.9 (10.5) |
| Weight, kg | 107.7 (18.3) | 102.9 (15.2) | 126.5 (17.5) |
| BMI, kg/m2 | 38.5 (4.7) | 38.1 (4.6) | 39.8 (5.1) |
| BMI <40, N (%) | 245 (62.8%) | 204 (65.6%) | 41 (51.9%) |
| BMI ≥ 40, N (%) | 145 (37.2%) | 107 (34.4%) | 38 (48.1%) |
| Race | |||
| Asian, N (%) | 4 (1.0) | 4 (1.3%) | 0 (0.0%) |
| Black or African American, N (%) | 150 (38.5) | 132 (42.4%) | 19 (24.1%) |
| White, N (%) | 230 (59.0) | 170 (54.7%) | 60 (75.9%) |
| More than one race, N (%) | 6 (1.5) | 6 (1.9) | 0 (0.0%) |
| Hispanic, N (%) | 18 (4.6) | 13 (4.2%) | 5 (6.3%) |
Values are mean ± standard deviation, except as otherwise noted.
Ratings of Terms for Excess Weight
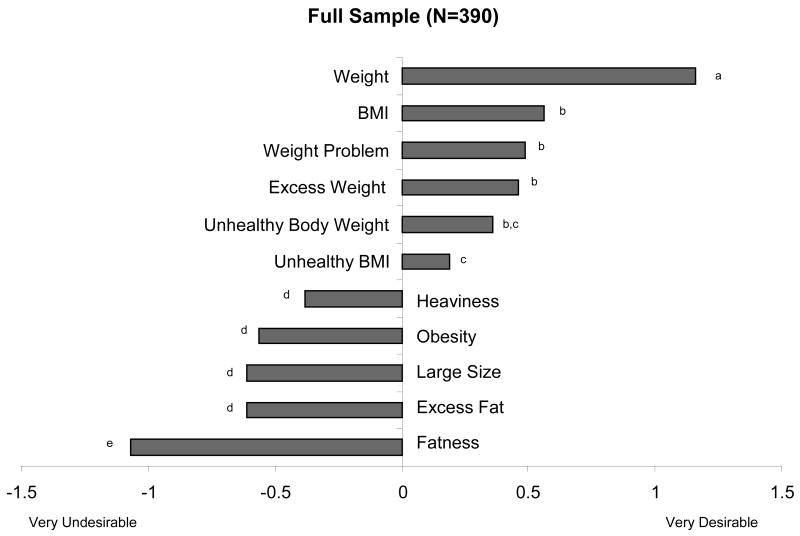
Figure 1 presents mean ratings of the 11 terms to describe excess weight, as determined for the full sample (N = 390). The term “fatness” received a mean rating of –1.1 ± 1.3, which was viewed as significantly (p < 0.001) more undesirable for practitioners to use than were all other terms. The four terms, “excess fat” (-0.6 ± 1.3), “large size” (-0.61 ± 1.3), “obesity” (-0.5 ± 1.4), and “heaviness” (-0.4 ± 1.2) were rated as significantly (p < 0.001) more undesirable then the remaining terms (but not from each other).
Figure 1.
Mean ratings of the 11 terms to describe excess weight, as determined for the full sample of participants. Terms with different letters differ significantly from each other (p < 0.05).
In contrast, the term “weight” received a mean rating of +1.2 ± 1.1, which was viewed as significantly (p < 0.001) more desirable than all other descriptors for characterizing excess weight. The terms “BMI,” “weight problem,” and “excess weight” also were viewed as generally desirable to participants, with all ratings in the range of 0.5 to 0.6. (Values for these terms did not differ significantly from each other.) The term “unhealthy body weight” (0.2 ± 1.3) did not differ significantly from the previously mentioned terms (p < 0.500). The term “unhealthy BMI” (0.2 ± 1.3) was rated as significantly (p < 0.034) less desirable than the terms “BMI,” “weight problem,” and “excess weight” but was still viewed as neutral to desirable.
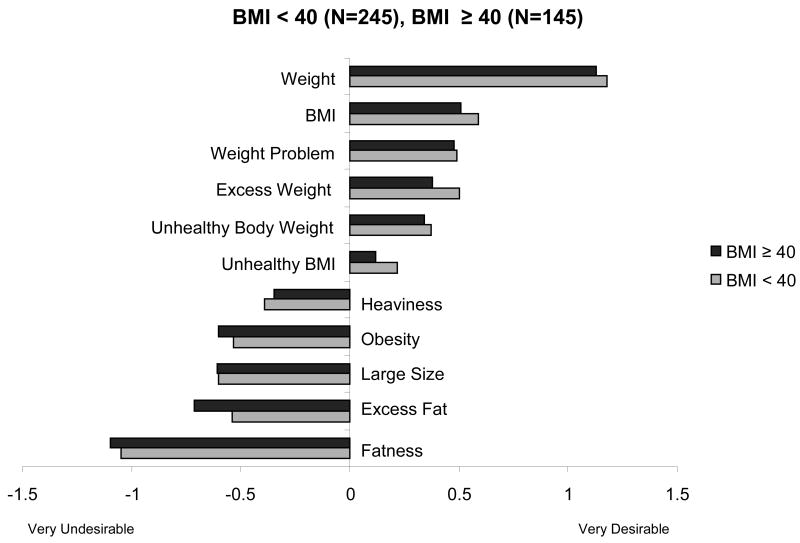
Ratings According to Participants' BMI
Figure 2 shows that participants with a BMI ≥ 40 kg/m2 did not differ significantly from persons with a lower BMI in their ratings of the desirability of any of the terms. This included the terms “obesity” and “fatness.”
Figure 2.
Ratings of 11 terms to describe excess weight as provided by participants with a BMI < 40 or BMI ≥ 40. None of the differences between BMI groups were statistically significant.
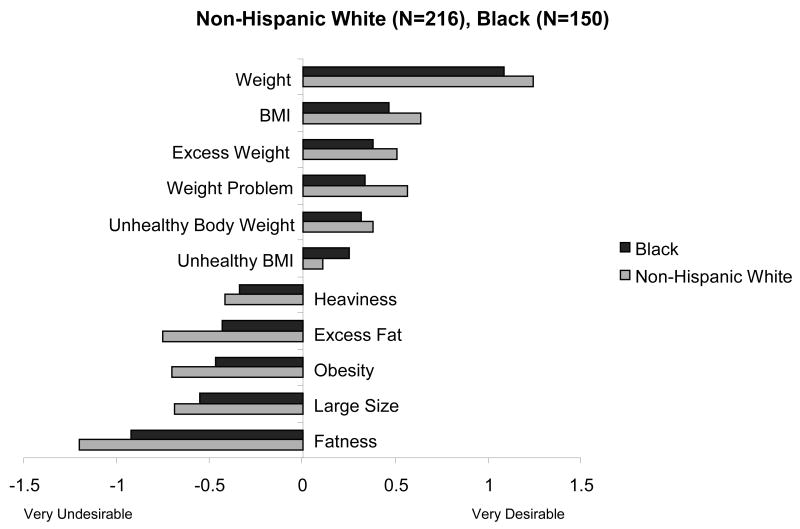
Ratings According to Gender and Race/Ethnicity
Men and women did not differ significantly in their ratings of any of the 11 terms (data not shown). The same conclusion was obtained in comparing the ratings of non-Hispanic white and African-Americans. Both groups rated “weight” as the most desirable term and agreed that “obesity,” “large size,” and “fatness” were undesirable descriptors (see Figure 3).
Figure 3.
Ratings of 11 terms to describe excess weight as provided by non-Hispanic White and African American participants. None of the differences between groups were statistically significant.
Ratings According to Open-Ended Questions
In response to open-ended questions, participants offered the term “weight” as their most preferred term for describing excess weight, followed by the term “weight problem.” Participants identified “fatness” as their least preferred term, followed by “obesity” (data not shown). Other desirable responses to the open-ended question (not listed in the questionnaire) included: “body weight,” “overweight,” “unhealthy weight,” “size,” and “health.” Undesirable descriptors (not in the questionnaire) included: “body fat,” “you are way too fat,” and “you are lazy.”
Discussion
Obese patients from six diverse primary care practices rated the terms “fatness,” “excess fat,” “large size,” and “heaviness” as undesirable for describing excess weight. These findings were observed in both men and women, in whites and African-Americans, and in participants with a BMI < or ≥ 40 kg/m2. Such terms may be perceived as derogatory and may reinforce negative weight-related attitudes towards obese individuals (5). The term “obesity” also elicited an undesirable rating. This finding is particularly important because obesity is a standard medical term that is used to describe excess body weight. Patients may have very different perceptions of the meaning of obesity compared to their health providers (3), and may associate the term with society's disapproval or stigmatization of overweight individuals (9,10).
By contrast, participants rated “weight” as the most desirable descriptor. This term elicited positive ratings from both genders, as well as from African-Americans and whites. The term “weight” may be preferable because it is both neutral and nonjudgmental -- it does not imply any negative attributes or impose any personal blame. Other descriptors that included the word “weight” were also rated as desirable, including the terms “weight problem,” “excess weight,” and “unhealthy body weight.” The term “BMI,” which is commonly used in clinical settings to describe body weight in relation to height, was also rated as desirable.
Results from the present investigation replicate those from our prior study published in 2003 (5) and show that the negative attitudes toward the term obesity and fatness are not limited to patients treated in an obesity-specialty clinic. While results from the two patient samples are similar, we note that participants in the present study did not rate “obesity” or “fatness” as negatively as respondents in the prior study. Obese female participants in the prior study gave the term “obesity” a mean rating of -1.4 and “fatness” a rating of -1.8, compared to ratings of -0.6 and -1.1, respectively, in the current study. Similar changes were found with men. We do not know whether the modest improvements in these ratings reflect the current participants' greater awareness of the obesity epidemic or are simply attributable to a difference in the two populations surveyed.
We found no support for our hypothesis that patients with severe obesity (≥ 40 kg/m2) would be more accepting of the terms “obesity” and “fatness.” This finding is consistent with results reported by Puhl et al. who examined experiences of weight bias in 318 overweight and obese adults (11). They found that participants reported similar experiences, perceptions, and stereotypes about obesity, regardless of BMI. We also failed to find differences in ratings provided by men and women.
Strengths of the present study include a large (N = 390) and diverse sample recruited from six primary care practices. This is in contrast to the more homogeneous cohort of participants recruited from a specialty clinic in our previous study (5). The addition of two open-ended questions to the Weight Preference Questionnaire allowed participants to share their suggestions for desirable terms to describe excess weight (which can be assessed in future studies).
This study also has several limitations. If the topics of weight and obesity had been framed (or worded) in a different manner, we may have obtained different (potentially more desirable) ratings of “obesity” and some of the other descriptors. Similarly, the questionnaire format, with the open ended questions following the 11 listed terms, may have encouraged participants to refer back to the listed terms and, thus, influenced their responses. All participants in the present study were recruited to participate in a weight loss trial and may have been more sensitive to weight-related terminology than obese persons who do not seek weight reduction. Thus, the present study needs to be replicated in a randomly-selected sample of persons who do not seek weight loss. Finally, this study also did not assess the desirability of preferred terms in an overweight population (BMI 25 to 29.9) or evaluate the acceptability of several other descriptors, including “overweight,” which was proposed in response to the open-ended questions.
The present results have important clinical implications for all health care professionals who treat obese individuals. In broaching a discussion of excess body fat and its associated health complications practitioners are encouraged to avoid using undesirable terms -- such as “obesity” or “fatness.” Use of such terms may offend or distress some patients and prevent them from continuing to discuss their weight. We encourage health care providers to use patient-friendly terms, such as “weight,” “weight problem,” or “BMI,” when broaching the topic of weight with their obese patients.
Acknowledgments
This study was funded by NIH grant U01-HL087072.
Footnotes
Disclosure: Dr. David Sarwer serves as a consultant for Allergan, Baronova, Enteromedics, and Ethicon Endo-Surgery and sits on the Board of Directors for the Surgical Review Corporation.
ClinicalTrial.gov Identifier: NCT00826774
References
- 1.Johnson C. Obesity, weight management, and self-esteem. In: Wadden TA, Stunkard AJ, editors. Handbook of Obesity Treatment. New York, NY: Guilford Press; 2002. pp. 480–493. [Google Scholar]
- 2.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 3.Ward SH, Gray AM, Paranjape A. African American perceptions of physician attempts to address obesity in the primary care setting. J Gen Int Med. 2009;24:579–84. doi: 10.1007/s11606-009-0922-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tailor A, Ogden J. Avoiding the term obesity: an experimental study of the impact of doctors' language on patients' beliefs. Patient Educ Couns. 2009;76:260–64. doi: 10.1016/j.pec.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 5.Wadden TA, Didie E. What's in a name? Patients' preferred terms for describing obesity. Obesity. 2003;11:1140–46. doi: 10.1038/oby.2003.155. [DOI] [PubMed] [Google Scholar]
- 6.Yeh HC, Clark JM, Emmons KE, et al. Independent but coordinated trials: insights from the practice-based Opportunities for Weight Reduction Trials Collaborative Research Group. Clin Trials. 2010;7:322–32. doi: 10.1177/1740774510374213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Derbas J, Vetter M, Volger S, et al. Improving weight management in primary care practice: a possible role for auxiliary health professionals collaborating with primary care physicians. Obesity and Weight Management. 2009;5:210–215. [Google Scholar]
- 8.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 9.Thomas SL, Hyde J, Karunaratne A, Herbert D, Komesaroff PA. Being ‘fat’ in today's world: a qualitative study of the lived experiences of people with obesity in Australia. Health Expect. 2008;11:321–30. doi: 10.1111/j.1369-7625.2008.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blixen CE, Singh A, Thacker H. Values and beliefs About obesity and weight reduction among African American and Caucasian women. J Transcult Nurs. 2006;17:290–97. doi: 10.1177/1043659606288375. [DOI] [PubMed] [Google Scholar]
- 11.Puhl RM, Moss-Racusin CA, Schwartz MB, Brownell KD. Weight stigmatization and bias reduction: perspectives of overweight and obese adults. Health Educ Res. 2008;23:347–58. doi: 10.1093/her/cym052. [DOI] [PubMed] [Google Scholar]