Abstract
The delay interval between encoding a future intention and detection of the retrieval cue is an essential feature of prospective memory (PM). McDaniel and Einstein’s (2000) multi-process theory posits that greater demands are placed on strategic monitoring processes as the delay interval lengthens. This hypothesis was examined in HIV-associated neurocognitive disorders (HAND), which are associated with strategic dyscontrol of PM likely secondary to prefrontostriatal circuit pathology. Seventy-eight seronegative adults and 49 individuals with HAND comprised the study groups, which were comparable with regard to demographic, psychiatric, and substance use factors. As part of a comprehensive neuropsychological evaluation, participants were administered a well-validated PM measure that included short (2-minute) and long- (15-min) task delay interval scales that utilized a standardized word search as the ongoing task. Results revealed a significant interaction of group and delay interval, with significant effects of HAND on PM at long, but not short delay. The long delay PM effect in HAND was driven primarily by deficits in time-based PM and was most strongly associated with markers of executive dysfunction. In concordance with the multi-process theory, individuals with HAND were disproportionately vulnerable to PM deficits at longer ongoing task delay intervals, which appear to be driven by strategic dyscontrol of PM that is consistent with the preferential disruption of prefrontal systems in neuroAIDS. Difficulty with successfully completing PM tasks following a longer delay could manifest in real-world problems, such as medication nonadherence and unemployment, and characterizing this specific deficit may inform remediation strategies.
Keywords: Prospective memory, HIV/AIDS, episodic memory, executive functions, time perception, AIDS Dementia Complex
Introduction
Prospective memory (PM) is a form of episodic memory characterized by the capacity to form and maintain an intention executed in response to a specific future cue (i.e., following a delay). Arguably the most influential PM theory, the multi-process model (McDaniel & Einstein, 2000) suggests that PM is a complex, multifaceted cognitive function that has varying automatic and strategic components at multiple levels. A range of component processes have been identified (e.g., Kliegel et al., 2008), including traditional memory processes such as encoding (i.e., intention and cue), retention of novel information (i.e., intention-cue pairing) during a delay interval, and upon cue detection, retrieval of the encoded intention from retrospective memory, and successful execution of the intention. One of the most widely studied aspects of the automatic and strategic components of PM is whether the nature of the retrieval cue is time-based (TB) or event-based (EB). That is, PM cues may take the form of an event, such as placing a letter in a mailbox as you pass it on your way home from work (i.e., EB), or the passage of time, such as taking a medication at 12-hour intervals (i.e., TB). Whereas successful EB PM performance is hypothesized to be relatively automatic because cue detection is more involuntary upon encountering the target, TB tasks require greater voluntary, strategic monitoring processes that are self-initiated (McDaniel & Einstein, 2000). Accordingly, TB PM is believed to be more reliant on cognitive control, which is supported by frontostriatal pathways, and therefore performance of TB tasks suffers with dysregulation of prefrontal systems (e.g., Raskin et al., 2011),
One understudied, but critical component of PM is the cognitive architecture of the delay interval. During the delay interval in which the intention-cue pairing is being retained, ongoing tasks are thought to place additional demands on attentional resources (McDaniel & Einstein, 2000), therefore requiring an individual to independently detect cues in the environment and then initiate retrieval of the paired intention without an explicit prompt (Einstein & McDaniel, 1990). According to the multi-process model, the length of time between intention formation and execution of the intention may influence PM performance. Longer delays may necessitate more strategic control by placing greater demands on limited executive resources supporting cue detection and monitoring; therefore, performance suffers as delay length increases and strategic processes may fail (McDaniel & Einstein, 2000). The dynamics of the delay interval are poorly understood, despite the fact that the delay itself is a defining feature of PM, but a handful of laboratory studies in healthy adults have produced some confirmatory results. Among healthy adults, increased task interval delays of 6, 21, and 36 minutes have been associated with worse PM performance (Martin, Brown & Hicks, 2011) and this effect may be exacerbated by increasing the strategic demands of the retrieval cue (Einstein et al, 2005). A recent study of ecstacy users, who have been shown to have deficient self-initiated strategy use (e.g., Brown et al., 2010), revealed disproportionately worse PM at longer (i.e., 15-min), but not shorter (i.e., 2-min) ongoing task delay intervals as compared to non-users (Weinborn et al., 2011).. The PM delay deficits among ecstasy users were particularly pronounced for time- versus event-based cues and were associated with executive dysfunction (Weinborn et al., 2011).
The present study aimed to examine this critical feature of PM in individuals with cognitive complications of human immunodeficiency virus (HIV), which are known as HIV-associated neurocognitive disorders (HAND) and are the neurobehavioral hallmark of neuroAIDS. Specifically, early in the course of infection the HIV lentivirus most commonly enters the central nervous system (CNS; Davis et al., 1992) by infecting perivascular macrophages, which cross the blood brain barrier and differentiate into microglia (Gonzalez-Scarano & Martin-Garcia, 2005). These cells are productively infected (e.g., Budka, 1990), meaning that they perpetuate viral replication and release viral proteins (e.g., gp120), which are by themselves neurotoxic, and infection also triggers an inflammatory response in the CNS involving chronic microglial activation and the release of a cascade of neurotoxic molecular events (e.g., upregulation of certain chemokines) (Gonzalez-Scarano & Martin-Garcia, 2005). Neurons are not known to be infected, but they are affected through this indirect pathway via neuronal apoptosis and/or synaptodendritic injury (e.g., axonal degeneration) (Ellis, Langford & Masliah, 2007). Although the resultant HIV-associated neuropathologies are evident throughout the CNS (DiStephano, Sabri, & Chiodi, 2005), evidence that the prefrontostriatal pathways are particularly susceptible to HIV arises from neuropathological (Everall et al., 2009) and neurobehavioral (Wilkie et al., 2000) findings, as well as structural (Kuper et al., 2011), functional (Chang et al., 2000), and metabolic (e.g., Chang et al., 2005) neuroimaging studies. These patterns of neuropathology eventually result in neurocognitive impairment, or HAND, in up to 50% of infected individuals despite treatment advances that have resulted in better-controlled physical disease (e.g., Heaton et al., 2010). Using a rigorous nosology to define and diagnose HAND, it serves as an important feature of neuroAIDS that helps to delineate the effects of HIV on the brain (Antinori et al., 2007). The typical neuropsychological profile of HAND involves executive dysfunction, bradyphrenia, bradykinesia, and episodic memory deficits characterized by deficient strategic monitoring and retrieval processes (e.g., Reger et al., 2002; Woods et al., 2005). Given the CNS effects of HIV on a broad neural network involving prefrontostriatal systems, similar to those involved in PM (e.g., Burgess et al., in press), it is not surprising that individuals with HAND report more subjective PM failures in their daily lives than healthy comparisons (Woods et al., 2007), and there is also objective evidence of poorer PM performance among HIV-seropositive individuals in the laboratory (e.g., Carey et al., 2006; Martin et al., 2007). Consistent with its preferential impact on prefronto-striato-thalamo-cortical circuits (see Ellis et al., 2009), the pattern of HIV-associated PM deficits appears to be driven by dysfunction of strategic encoding, monitoring, and cue detection and retrieval. At the level of encoding, the strategic hypothesis of HAND-associated PM deficits is supported by findings of lower performance when the EB cue was semantically unrelated to the intention, which correlates with executive dysfunction (Woods et al., 2010). Notably, normal recognition performance is typically demonstrated across PM studies in HIV infection (e.g. Carey et al., 2006), suggesting that poorer PM performance reflects difficulty with utilizing strategic monitoring and retrieval processes. Regarding dysregulation of the strategic aspects of monitoring for cue detection and retrieval, evidence in HIV infection has shown a significantly larger effect size for TB versus focal EB PM (Martin et al., 2007), and a slightly larger effect size for TB tasks compared to non-focal EB tasks (Zogg et al., 2011). These findings are consistent with the multi-process theory in that response cue characteristics are purportedly key to the success of switching attention from the ongoing distractors that intervene during the delay interval to detection of the appropriate cue, requiring more deliberate internal, self-initiated, strategic monitoring for detecting and retrieving a TB cue rather than the occurrence of an event, or an EB cue, which likely involves more external and automatic processes (McDaniel & Einstein, 2000). Therefore, the poorer performance on TB tasks among HIV-seropositive individuals relative to their seronegative counterparts is consistent with HIV-associated disruption of the frontostriatal pathways that subserve the greater complexity of monitoring and retrieval processes associated with TB tasks (e.g., Raskin et al., 2011). Studies have also consistently demonstrated that PM deficits in HIV are associated with executive dysfunction (e.g., Zogg, et al, 2011). Moreover, HIV-associated PM deficits negatively impact everyday functioning, as demonstrated by associations with increased risk of dependence in managing instrumental daily activities (e.g., managing finances; Woods et al., 2008), medication nonadherence (specifically TB cues; Woods et al., 2009), general healthcare noncompliance (Zogg et al., 2010), unemployment (Woods et al., 2011), lower health-related quality of life (Doyle et al., in press), and engagement in HIV transmission risk behaviors (Martin et al., 2007). Of particular clinical relevance, the associations between PM and these functional outcomes in HIV appear to be largely independent of other established risk factors, including demographics, psychiatric comorbidity, disease severity, and general cognitive deficits (e.g., Woods et al., 2009).
Given this combined evidence, the present study aimed to evaluate the possible differential effect of delay interval on PM performance among individuals with HAND. In so doing, the current study utilized a cognitive neuropsychology approach to the study of prospective memory in neuroAIDS through application of a theoretical model to test specific hypotheses that were based on current understanding of the neural systems and cognitive mechanisms of HAND. Consistent with the predictions of the multi-process theory and the pattern of frontal systems dysregulation evident both neuropathologically and neurobehaviorally in HAND, it was hypothesized that individuals with HAND would show disproportionately poorer PM performance during long-delay PM tasks relative to short-delay, particularly for TB versus EB tasks, as compared to a seronegative comparison group. It was also predicted that individuals with HAND would report more subjective long-delay PM failures than short-delay from their daily lives. Furthermore, given that the cognitive mechanism of the difference in performance between the HIV-seropositive and comparison groups at long-delay would be strategic dyscontrol according to the multi-process theory, long-delay performance was hypothesized to be associated with executive dysfunction.
Method
Participants
The study sample included 49 individuals with HAND and 78 seronegative comparison subjects who were recruited from the San Diego community or local HIV clinics. HAND was diagnosed via multidisciplinary case conference according to the recently updated Frascati criteria (Antinori et al., 2007). The diagnosis was based on the results of a comprehensive neuropsychological (excluding PM performance or complaints to avoid criterion contamination), psychiatric, and neuromedical assessment (see Woods, Iudicello, et al., 2008). Seventy-eight percent of the HAND participants were classified as “Asymptomatic Neurocognitive Impairment” (ANI; i.e., global neurocognitive impairment without evidence of major functional disability), 22% met criteria for either Mild Neurocognitive Disorder (MND; global neurocognitive impairment with mild-to-moderate functional disability) or HIV-associated dementia (HAD; i.e., moderate-to-severe global neurocognitive impairment with at least moderate functional disability). Individuals with histories of severe psychiatric (e.g., psychosis), medical (e.g., hepatitis C), or neurological (e.g., stroke, traumatic brain injury, seizure disorders) conditions were excluded. We also excluded individuals with verbal IQ scores <70 (based on Wechsler Test of Adult Reading [WTAR]; Psychological Corporation, 2001) or diagnoses of substance use disorders (SUD) within six months of evaluation as determined by the Composite International Diagnostic Interview (CIDI version 2.1; World Health Organization, 1998), a computer-assisted diagnostic instrument with a structured interview format. All participants underwent a urine toxicology test to screen for illicit substance use on the day of testing. CIDI modules were also administered to assess for the most prevalent psychiatric disorders in HIV infection (Atkinson, Person, Young, Deitch, & Treisman, 2005), including current (i.e., past 30 days) and lifetime diagnoses of Major Depressive disorder (MDD), Generalized Anxiety disorder (GAD) and substance dependence (lifetime diagnosis only per exclusion of individuals with current SUD diagnosis). Additionally, the Profile of Mood States (POMS; McNair, Lorr, & Droppelman, 1981) was administered to measure self-reported symptoms of current affective distress. HIV status was determined by enzyme linked immunosorbent assays and confirmed by a Western Blot test. Table 1 displays the demographic, HIV disease, and psychiatric characteristics of the study samples. The study groups were well balanced in terms of demographics, psychiatric diagnoses and current affective distress, and histories of substance use disorders (ps > .10). The HAND sample had relatively well controlled HIV disease (e.g., 74% undetectable viral load) and 86% were prescribed antiretroviral therapy.
Table 1.
Demographic, Psychiatric, and Medical Characteristics of the Study Participants
| Characteristics | HIV− (n=78) | HIV+ (n=49) | p |
|---|---|---|---|
| Demographic | |||
| Age (years) | 42.7 (14.5) | 44.7 (12.1) | .41 |
| Education (years) | 14.3 (2.2) | 13.7 (2.7) | .17 |
| Sex (% female) | 9.0 | 12.2 | .55 |
| Ethnicity (% Caucasian) | 62.8 | 49.0 | .13 |
| Psychiatric | |||
| Major depressive disorder a (%) | 28.2 | 42.9 | .09 |
| Generalized anxiety disorder a (%) | 2.6 | 8.2 | .20 |
| Substance dependence a (%) | 62.8 | 59.2 | .68 |
| POMS total | 40.4 (26.9) | 47.4 (18.3) | .11 |
| HIV disease | |||
| AIDS (%) | - | 49.0 | |
| cART (%) | - | 81.6 | |
| Nadir CD4b (cells/µl) | - | 200 (55, 382.5) | |
| Current CD4b, c (cells/µl) | - | 637 (364.3, 935.5) | |
| HIV RNAb, c log10 (% detectable) | - | 25.0 |
Note. WTAR = Wechsler Test of Adult Reading. POMS = Profile of Mood States. cART = combination antiretroviral therapy.
lifetime diagnoses.
Median (interquartile range).
N = 48
Procedure
Prospective memory
All participants received the research version (Woods, Moran, Dawson, Carey, & Grant, 2008) of the Memory for Intentions Screening Test (MIST; Raskin et al., 2010). This laboratory-based measure of PM includes four short (i.e., 2-min) delay and four long (i.e., 15-min) delay trials, during which participants are engaged in a standardized ongoing task (i.e., a word search). The 2- and 15-min delay scales are balanced on time- and event-based cues and action versus verbal responses. Responses are coded from 0–2 for each item, such that each of the 2-min and 15-min delay scale total scores range from 0 to 8, with higher scores indicating better performance. In addition, we generated separate error type totals for the 2-min and 15-min delay scales (range = 0 to 1), including omission (i.e., no response), loss of time (i.e., executing a correct intention ≥ 15% of the target time), task substitution (e.g., an intrusion error, such as responding verbally to an action-based intention or vice versa), and loss of content (i.e., awareness that a response is required but failure to recall the content) errors. Finally, participants were administered an eight-item, three-choice post-test recognition task, from which we generated separate error totals for recognition of 2-min (range = 0 to 4) and 15-min (range = 0 to 4) delay cues. MIST data were non-normally distributed (Shapiro-Wilk W < .01), but given the nature of the study design (i.e., involving both between-subjects and within-subjects factors) and the relative robustness of ANOVA procedures, a parametric approach was used. Of note, all findings regarding group differences were consistent when verified with Wilcoxon Ranked Sum Tests.
Self-reported PM complaints were assessed with the Long- and Short-term PM scales of the Prospective and Retrospective Memory Questionnaire (PRMQ; Smith et al. 2000). The PRMQ includes eight PM complaints that measures the frequency with which perceived PM difficulties occur in everyday life on a 5-point Likert-type scale that ranges from 1 (“never”) to 5 (“very often”). The 8 items on the PRMQ PM scale comprise four Short-term items, two of which are self-cued (e.g., “Do you decide to do something in a few minutes’ time and then forget to do it?”) and two of which are environmentally-cued (e.g., “Do you intend to take something with you before leaving a room or going out, but minutes later leave it behind, even though it’s there in front of you?”), as well as four Long-term items, also consisting of two self-cued (“Do you forget appointments if you are not prompted by someone else or by a reminder such as a calendar or diary?”) and two environmentally-cued (e.g., “Do you forget to buy something you planned to buy, like a birthday card, even when you see the shop?”) complaints. The Short-tem and Long-term PM subscales each have a range of scores from 4 to 20, and therefore the PRMQ PM scale total score has a minimum score of 8 and a maximum of 40.
Participants also completed an experimental measure of time estimation (Mimura et al., 2000) in which they were required to estimate the duration of elapsed time during four brief intervals (i.e., 15, 30, 45, and 90 sec in a randomized order), without the aid of a clock. The discrepancy between the actual time elapsed and the participants’ response was used as the primary outcome (see Woods et al., 2009).
Clinical Neurocognitive Battery
The specific domains assessed were: 1) retrospective memory, which included the long delayed free recall trials of the California Verbal Learning Test – Second edition (CVLT-II; Delis, Kramer, Kaplan, & Ober, 2000) and the Logical Memory subtest of the Wechsler Memory Scale-III (Psychological Corporation, 1997); 2) executive functions (Trail Making Test, Part B minus part A (TMT; Reitan & Wolfson, 1985), action (verb) fluency (Woods et al., 2005), and total move score from the Tower of London – Drexel (ToL-DX; Culbertson & Zillmer, 2001); 3) attention (Digit Span subtest from the Wechsler Adult Intelligence Scale – Third Edition (Psychological Corporation, 1997)) and CVLT-II trial 1; and 4) motor (grooved pegboard, KlØve, 1963). Raw scores were converted to population-based z scores derived from both study groups combined and then averaged across the tests in each domain to create composite z scores for each ability area. In all instances, scores were converted so that higher z values reflect better performance.
Results
A repeated-measures mixed-model ANOVA with group (i.e., HAND vs seronegative comparison) as the between-subjects variable and delay interval (i.e., 2-min vs. 15-min) as the within-subjects factor revealed a trend-level main effect of group [F (1, 125) = 3.5, p = .07, ηp2= 0.027] and a significant main effect of delay interval [F (1, 125) = 169.6, p < .0001, ηp2= 0.576]. Notably, there was a significant group by delay interval interaction [F (1, 125) = 7.6, p = .007, ηp2= 0.058]. In a model including current affective distress (i.e., POMS Total) as a covariate, the pattern of results was similar; that is, the significant main effect of delay interval and the significant interaction between group and delay interval remained (ps < .05), whereas the main effect of group was nonsignificant (p > .05). Furthermore, POMS Total was not correlated with either the MIST 2min or 15 min delay scales in the HAND group (ps > .10).
Planned follow-up group comparisons revealed no effect of group on the 2-min delay PM tasks (p = .80, Cohen’s d = 0.05], but a significant group effect on the 15-min delay PM tasks was observed such that individuals with HAND (M = 4.69, SD = 1.85) performed significantly worse than the seronegative comparison group (M = 5.58, SD = 1.85; p = .01, Cohen’s d = 0.48).
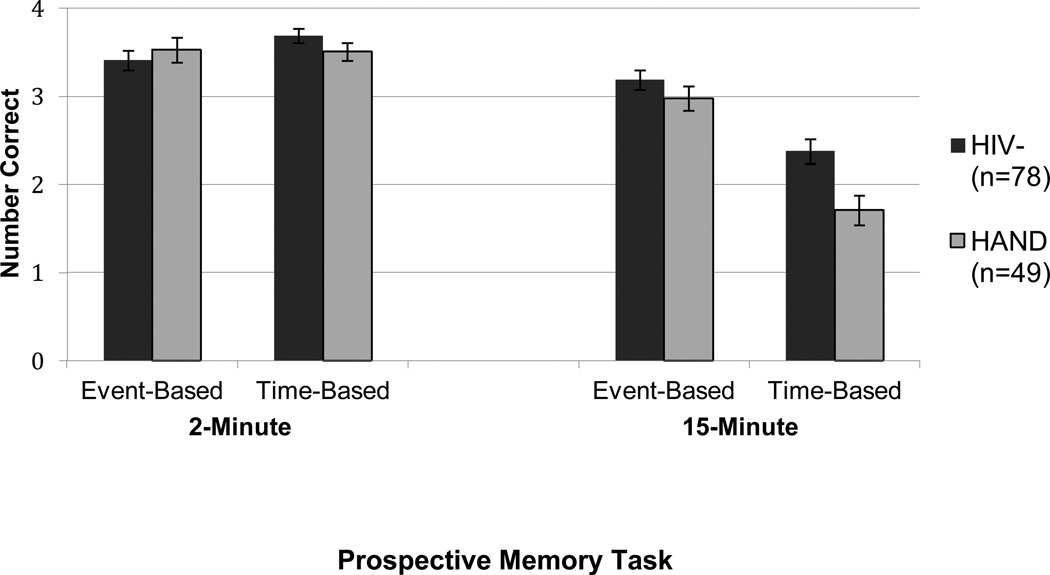
To examine whether the HIV effect on the 15-min delay PM tasks varied by cue type (i.e., time- vs. event-based cues), a follow-up repeated measures mixed-model ANOVA was conducted with group (i.e., between-subjects) and cue type (i.e., within-subjects; TB vs. EB) on the 15-min scale. A significant main effect of group was observed [F(1, 125) = 6.9, p = .01, ηp2= 0.052], as well as a main effect of cue type [F(1, 125) = 96.4, p < .0001, ηp2= 0.435]. Importantly, a significant group by cue type interaction was observed [F (1, 125) = 4.7, p = .03, ηp2= 0.036]. As shown in Figure 1, planned group comparisons conducted to follow-up the interaction showed that there was no difference between the groups for the 15-minute EB scale (p = .22, Cohen’s d = 0.21), but the HAND group performed significantly more poorly on the 15-minute TB trials (M = 1.71, SD = 1.15) than the seronegative comparison group (M = 2.38, SD = 1.25; p = .003, Cohen’s d = 0.56]. With regard to the error types observed on the 15-minute TB scale, Table 2 shows that significant group differences were observed for omissions (p = .02, Cohen’s d = 0.37) and loss of time errors (p < .001, Cohen’s d = 0.50), whereas no differences were found for the other error types (ps > .05).
Figure 1.
Bar graph displaying the effects of HIV-associated Neurocognitive Disorders (HAND) on short (2-min) and long (15-min) PM ongoing task delays by time- and event-based cue type
Table 2.
Time- and Event-based Prospective Memory Performance on the 15-minute Trials by Group
| PM Score | HIV− (n=78) | HAND (n=49) | p | Cohen’s d (95% CI) |
|---|---|---|---|---|
| 15-min Time-based | 2 (1, 3.3) | 2 (1, 2.5) | .003 | 0.56 (−.83, −.11) |
| Omissions | 0 (0, 1) | 0 (0, 1) | .02 | 0.37 (.01, .73) |
| Task substitutions | 0 (0, 1) | 0 (0, 1) | .95 | 0.04 (−.32, .39) |
| Loss of time | 0 (0, 0) | 0 (0, 1) | <.001 | 0.50 (.14, .86) |
| Loss of content | 0 (0, 1) | 0 (0, 1) | .58 | 0.12 (.48, .23) |
| Recognition (total) | 2 (2, 2) | 2 (2, 2) | .95 | 0.00 (−.36, .36) |
| 15-min Event-based | 3 (2.8, 4) | 3 (2, 4) | .24 | 0.22 (−.78, −.06) |
Note. Data represent medians with interquartile ranges in parentheses.
As noted previously, the pattern of findings was confirmed when a non-parametric approach was used (i.e., a series of Wilcoxon Ranked Sums Tests). That is, a significant HAND effect was observed for the 15-minute (p < .05) but not the 2-minute delay (p > .05). Moreover, and there was a significant group effect on the difference score between the 2-minute and 15-minute delay trials (p < .05), supporting the significant interaction between group and delay interval observed in the parametric analyses. Similarly, there was a significant between-groups effect on the time-based (p < .05) but not the event-based (p > .05) cues within the 15-minute scale. The group effect was significant for the difference score between the 15-minute EB and TB cue trials (p < .05), consistent with the significant interaction. Given this confirmation, the parametric approach was retained because it was more readily interpretable given our study design and the robustness of the analytic procedures.
Given these findings, post hoc analyses were conducted to investigate differences on the 15-minute delay task overall and the 15-minute TB cue scale as a function of HAND diagnostic subgroups. Given the relatively small number of participants with MND and HAD, we grouped these individuals together into a single “syndromic HAND” group. Individuals with ANI were classified in a separate “subsyndromic” group. The syndromic and subsyndromic HAND groups were then compared to the HIV- group using a one-way ANOVA. Significant omnibus group differences were observed on the 15-minute task [F(2, 124) = 4.0, p = .02]; the syndromic HAND group (M = 4.2, SD = 1.9) performed significantly worse than the HIV- group (M = 5.6, SD = 1.8; p = .02, Cohen’s d = −0.65), as did the ANI group (M = 4.8, SD = 1.8, p = .05, Cohen’s d = −0.37). The two HAND groups did not differ statistically from each other (p = .30, Cohen’s d = 0.29). Significant group differences were also observed on the 15-minute TB cue [F(2, 124) = 4.9, p = .01]; the syndromic HAND group (M = 1.5, SD = 1.3) performed significantly worse than the HIV- group (M = 2.4, SD = 1.3; p = .02, Cohen’s d = −0.58), as did the ANI group (M = 1.8, SD = 1.1, p = .01, Cohen’s d = −0.41). Once again, the two HAND groups did not differ statistically from each other (p = .42, Cohen’s d = 0.22).
Investigation of the cognitive correlates of the 15-minute scale revealed significant associations with several cognitive domain-based z-scores in each group, as shown in Table 3, including Attention, Retrospective Memory, Executive Functions, and Motor ability domains (ps < .05). Therefore, all domains were included in a multivariate regression analysis, and the cognitive z-scores accounted for a significant amount of variance in the seronegative [F(4, 71) = 8.09, R2 adjusted = 0.27, p < .0001] and HAND [F(4, 43) = 3.16, R2 adjusted = 0.16, p = .02] groups, with only the executive functions domain z-score emerging as a significant predictor in the HAND model (β = 0.36, p = .02), and both Retrospective Memory (β = 0.28, p = .01) and Executive Functions (β = 0.29, p = .007) were significant predictors in the HIV- model. All other domain z-scores were non-significant across both models (ps > .05). Notably, time estimation was not correlated with 15-min delay PM in either the HIV- sample (rho = 0.05, p = .69) or the HAND sample (rho = −0.17, p = .23).
Table 3.
Correlations between 15-minute PM Score and Neurocognitive Functions by Group
| Domain (z-score) | Spearman’s rho | p |
|---|---|---|
| HIV− | ||
| Attention | .37 | <.001 |
| Retrospective Memory | .40 | <.001 |
| Executive Functions | .35 | .002 |
| Motor | .20 | .09 |
| HAND+ | ||
| Attention | .26 | .07 |
| Retrospective Memory | .33 | .02 |
| Executive Functions | .39 | .006 |
| Motor | .33 | .02 |
Regarding PM complaints related to short and long-delay tasks on the PRMQ, there was a trend-level main effect of group [F(1, 125) = 0.03, p = .05], and there was a significant effect of delay interval [F(1, 125) = 0.25, p < .0001]. There was no significant group by delay interval interaction [F(1, 125 = 0.009, p = .30], but planned comparisons showed that there was no difference between the groups with regard to level of short-delay PM complaints (HIV− M = 8.92, SD = 2.67; HIV+ M = 9.67, SD = 3.11; p = .15, Cohen’s d = 0.26) but the HIV-seropositive group did report significantly more long-delay PM complaints (M = 8.88, SD = 3.30) compared to the seronegative comparison group (M = 7.76, SD = 2.41; p = .03, Cohen’s d = 0.39).
Discussion
The findings of the present study are consistent with the predictions of multi-process theory (McDaniel & Einstein, 2000). That is, for individuals with HIV-associated neurocognitive disorders (HAND), as the delay interval increases and other tasks intervene (i.e., distractors), it becomes more difficult to maintain higher-level strategies for surveilling the environment for cues for a protracted period of time. Specifically, there was a significant interaction whereby we observed effects of HAND on PM at longer, 15-minute delay intervals, but not at the shorter 2-minute delays. It is unlikely that the observed findings can be exclusively attributed to outliers with more severe forms of HAND. Specifically, while the syndromic (i.e., MND and HAD) and subsyndromic (i.e., ANI) groups significantly differed from the HIV- group on longer PM delays, they did not differ from each other. Nevertheless, it is important to acknowledge that the effect size for the syndromic HAND group versus seronegatives was somewhat larger than that which was observed for the subsyndromic HAND sample. This moderate effect size discrepancy as a function of syndromic HAND is commensurate with previous studies showing that HIV-infected individuals with everyday functioning problems commonly experience PM deficits (e.g., Woods et al., 2009). Overall, the use of the multi-process theoretical model to delineate HAND effects on shorter and longer delay intervals expanded our understanding of the component processes of prospective memory in neuroAIDS.
This line of research is important in the context of the demonstrated sensitivity of PM to daily functioning changes in HIV infection (e.g., Woods, Iudicello, et al., 2008), and the potential for evaluation of a wider range of delay intervals to enhance the ecological validity of the delay effect of the PM construct. Overall, PM has also shown incremental ecological validity in detection of everyday functioning impairment in HIV, ranging from unemployment (Woods, et al., 2011) to medication nonadherence (e.g., Woods, Moran, Carey, et al., 2008; Woods et al., 2009). For example, Woods et al. (2009) reported that HIV-infected persons with baseline deficits in TB PM had a sixfold risk of antiretroviral non-adherence at 30-day follow-up as measured by an electronic medication tracking system. Importantly, direct evaluation of the association between long-delay PM deficits and instrumental activities of daily living (IADL) could prove clinically useful in identifying individuals at risk for functional impairment. Medication adherence is a type of IADL that likely involves longer delay intervals, as well as commonly demands a TB cue. HAND effects on long-delay PM may negatively impact adherence, which is especially consequential given the importance of strict adherence to antiretroviral therapy. Accordingly, future studies may seek to demonstrate a possible association between poor long-delay PM performance and difficulty with adherence to a medication regimen. Furthermore, employment status may also be impacted by a long-delay PM deficit, especially for individuals who work fairly independently and for whom there would be a longer interval between being assigned a task and the time at which it is executed, with the added potential for multiple intervening tasks occurring in the interval. Given that many individuals with HIV may still be working or returning to work in the cART era due to improved physical disease outcomes, deficits such as long-delay PM might have a greater impact due to the higher demands of sustaining a job, whereas these effects could otherwise be more subtle in a simpler daily routine. Predictors of employment status and return to work are highly relevant due to the public health importance of unemployment in HIV infection, and therefore further investigation of delay effects in HAND may be warranted based on the present findings.
Another clinical implication of identifying a long-delay PM deficit in HIV infection is the potential for remediation based on evidence from a PM intervention delivered to individuals with traumatic brain injury in which targeted training for completion of designated tasks at specific times was provided, and the findings suggested that individuals can improve their prospective memory “span” such that they can successful execute an intention following increasingly longer delays between intention formation and cue detection (Raskin & Sohlberg, 1996). The study also demonstrated that the improvement appeared to generalize from the training session to the natural “daily life” environment, and therefore individuals with HIV who evidence a PM delay deficit may also improve with this training, which might also carry a potential positive impact on medication adherence and job performance.
Interestingly, this effect of HAND on longer delay PM performance was pronounced for time-based (TB) tasks as compared to event-based (EB) tasks in the current study, supporting the suggestion that the differential effect of HAND on PM at longer delay intervals may be related to strategic dyscontrol. This result extends the findings of a previous study that reported a greater effect size of HIV on TB versus EB tasks overall (Zogg et al., 2011) and is also consistent with the multi-process theory in that TB cues are believed to be reliant upon executive control of strategic processes that are effortful and self-initiated. Therefore the known executive dyscontrol due to HIV infection could reasonably result in poorer performance on TB tasks at the 15-minute delay due to the increased strategic load of both the nature of the task type and the longer duration of the delay. This specific result was previously demonstrated in ecstacy users, for whom inefficient use of monitoring and cue detection strategies also purportedly explained the long-delay PM deficit (Weinborn et al., 2011). Notably, the lack of an association between a measure of time estimation and 15-minute TB PM performance in the present study, consistent with the findings of Weinborn and colleagues (2011), suggests these results are not simply due to inability to correctly estimate elapsed time.
An analysis of the error types on the long-delay scale revealed that the longer delay effect was driven by failure to respond to a cue (i.e., omissions) and responding to a time-based cue at the incorrect time (i.e., loss of time). Demonstration of these error types is conceptually consistent with the effect of greater strategic load of the task on two levels, including its TB-nature and longer delay interval, especially given that these errors occur in the context of intact recognition performance for TB tasks from the 15-minute scale. Such a finding also argues against the alternative hypothesis that the longer delay results in poorer PM performance due to failure of RM, since normal recognition memory performance indicates that RM was preserved over the delay. The further-refined clarification that this discordance between normal recognition and elevated errors of omission and loss of time does not provide is the extent to which the greater strategic load of long-delay time based tasks taxes monitoring versus retrieval processes, resulting in PM failures. Elucidation of this distinction may be useful in studying longer delay interval of hours, or even days, which may be more ecologically valid than the brief laboratory testing evaluated in the present study. The multi-process theory predicts that as the delay interval lengthens into this range, the processes involved in monitoring the environment may be more automatic since strategic control could not be sustained for such a duration (e.g., McDaniel & Einstein, 2000). Furthermore, a negative effect of another type of delay interval that occurs between detection of the cue and accurate execution of the intention has been demonstrated among older adults following very brief delays (i.e., up to 30 seconds), and it is possible that self-initiated, strategic processes must be engaged during that interval to avoid a PM failure despite successful cue detection (McDaniel et al., 2003). Given this potentially similar mechanism to the delay between intention formation and cue detection (i.e., strategic control) and the possible real world significance of this “do it or lose it” effect of delayed execution (McDaniel et al., 2003) for individuals with HAND, such as postponing administration of a medication despite detection of the cue resulting in a missed dose, this delay interval also warrants investigation among individuals with HAND.
A final result providing evidence from the current study that longer-delay PM deficits in HIV infection are related to strategic dyscontrol is the significant association between the 15-minute scale and an executive functions domain z-score. Based on correlational analyses, the 15-minute scale was associated with multiple domains in both the HIV-seropositive and seronegative comparison groups. However, once those domain z-scores were entered simultaneously in a multiple regression analysis, only executive functions emerged as a significant predictor of 15-minute scale performance in both groups, similar to the findings of Weinborn and colleagues (2011) among ecstacy users. The executive domain z-score comprised tasks measuring cognitive flexibility (i.e., Trail Making Test Part A – B), planning (i.e., Tower of London Total Moves), and semantic fluency (i.e., action words), which is a self-sustained behavior that benefits from strategy use. Combined, these tasks mirror the type of ability required for strategic control of monitoring during a long delay for successful cue detection. This association is also consistent with the previously demonstrated prominence of executive dysfunction in HIV infection, and provides further evidence of the demonstrated association between TB PM and measures of executive functions (e.g., Raskin, Woods, et al, 2011; Zogg, Woods, et al, 2011; Costa et al, 2008).
Although these data are inferential, the preferential prefronto-striato-thalamo-cortical circuit dysregulation in HIV infection could account for strategic dyscontrol predicted by the multi-process theory during the longer interval. resulting in the observed pattern of differential effects of HIV on PM performance at longer versus shorter delays. Supporting this systems level interpretation are the differential findings regarding TB tasks on long delay PM and the stronger correlations of long delay PM with executive functions. Moreover, significant effects on longer versus shorter delay intervals have been observed in other populations in which prefrontostriatal dysfunction is also evident, including Parkinson’s disease (Raskin et al., 2011). Nevertheless, we cannot exclude the possible role of the interconnection between prefronto-striato-thalamo-cortical circuits and the medial temporal lobe, which is also affected in HAND (Maki et al., 2009) and is a key component of neurocognitive models of PM, including delay. As such, an fMRI study of PM tasks at varying delays would help to delineate the neural correlates in both healthy and disease populations such as HAND.
The current findings showed that individuals with HIV infection report more subjective complaints regarding long-delay PM tasks in their daily lives than seronegative comparisons, and the level of complaints regarding short-delay PM tasks was comparable between the groups. This indirectly suggests that individuals with HIV may be aware of their impaired long-delay PM performance in everyday tasks, especially those with a TB cue. Importantly, the design of the PRMQ, which recorded PM complaints in the current study, does not specify the duration of the delay and therefore it is not entirely clear if it is an everyday expression of the long delay PM deficit observed in the present findings. However, it is an intriguing finding that could be further explored with a revised questionnaire that carefully delineates time intervals in order to add real-world significance to the HAND effect on long delay PM performance.
Given that the groups in our study were comparable with regard to demographic (i.e., age, education, gender, and ethnicity) and psychiatric factors (i.e., no current diagnoses, similar levels of current psychiatric distress), it is unlikely that any of these variables better accounted for our findings. Furthermore, the HAND group was relatively healthy with well-managed disease (i.e., a majority had undetectable HIV viral loads and were currently prescribed antiretroviral therapies). Nevertheless, there are some limitations to the current study. Notably, we cannot rule out the possibility that greater challenge of the longer delay task relative to the shorter delay task contributed to our findings given that the delay interval trials were not balanced on level of difficulty (e.g., Chapman & Chapman, 1973). Additionally, the design of the MIST involves overlapping delay (i.e., 2- and 15-min) and cue type (i.e., time- and event-based) trials embedded in a clinical measure. Future studies may design a test with randomized and separate trials of tasks across various delay intervals, and those tasks could also be matched psychometrically to account for level of difficulty. Such adjustments would not only serve to hone the delay effect signal and temper psychometric limitations, but also may lay the groundwork for extending the findings of the current study by evaluating even longer delay intervals and investigating the potential shift toward more automatic processes predicted by the multi-process theory as the delay interval becomes extended. In addition, future studies may examine the effect of syndromic HAND on longer delay PM intervals to fully characterize the role of these diagnoses with larger sample sizes.
Acknowledgments
The HIV Neurobehavioral Research Program (HNRP) Group is affiliated with the University of California, San Diego, the Naval Hospital, San Diego, and the Veterans Affairs San Diego Healthcare System, and includes: Director: Igor Grant, M.D.; Co-Directors: J. Hampton Atkinson, M.D., Ronald J. Ellis, M.D., Ph.D., and J. Allen McCutchan, M.D.; Center Manager: Thomas D. Marcotte, Ph.D.; Naval Hospital San Diego: Braden R. Hale, M.D., M.P.H. (P.I.); Neuromedical Component: Ronald J. Ellis, M.D., Ph.D. (P.I.), J. Allen McCutchan, M.D., Scott Letendre, M.D., Edmund Capparelli, Pharm.D., Rachel Schrier, Ph.D.; Neurobehavioral Component: Robert K. Heaton, Ph.D. (P.I.), Mariana Cherner, Ph.D., David J. Moore, Ph.D., Steven Paul Woods, Psy.D.; Neuroimaging Component: Terry Jernigan, Ph.D. (P.I.), Christine Fennema-Notestine, Ph.D., Sarah L., Archibald, M.A., John Hesselink, M.D., Jacopo Annese, Ph.D., Michael J. Taylor, Ph.D.; Neurobiology Component: Eliezer Masliah, M.D. (P.I.), Ian Everall, FRCPsych., FRCPath., Ph.D., T. Dianne Langford, Ph.D.; Neurovirology Component: Douglas Richman, M.D., (P.I.), David M. Smith, M.D.; International Component: J. Allen McCutchan, M.D., (P.I.); Developmental Component: Ian Everall, FRCPsych., FRCPath., Ph.D. (P.I.), Stuart Lipton, M.D., Ph.D.; Clinical Trials Component: J. Allen McCutchan, M.D., J. Hampton Atkinson, M.D., Ronald J. Ellis, M.D., Ph.D., Scott Letendre, M.D.; Participant Accrual and Retention Unit: J. Hampton Atkinson, M.D. (P.I.), Rodney von Jaeger, M.P.H.; Data Management Unit: Anthony C. Gamst, Ph.D. (P.I.), Clint Cushman, B.A., (Data Systems Manager), Daniel R. Masys, M.D. (Senior Consultant); Statistics Unit: Ian Abramson, Ph.D. (P.I.), Christopher Ake, Ph.D., Florin Vaida Ph.D.
This research was supported by National Institute of Health grants 2R01MH073419, 1T32DA031098, T32AA013525, and P30MH62512. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, nor the United States Government. The authors thank Dr. Catherine L. Carey, Lisa Moran, Matthew Dawson, Ofilio Vigil, Sarah Gibson, Marizela Cameron, and P. Katie Riggs for their help with study management and Dr. Sarah Raskin for providing us with the MIST.
References
- Antinori A, Arendt G, Becker JT, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69:1789–1799. doi: 10.1212/01.WNL.0000287431.88658.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson JH, Person C, Young C, Deitch D, Treisman G. The Neurology of AIDS: Psychiatric Disorders. In: Gendelman HE, Swindels S, Grant I, Lipton SA, Everall I, editors. The Neurology of AIDS. 2nd ed. New York: Oxford University Press; 2005. [Google Scholar]
- Brown J, McKone E, Ward J. Deficits of long-term memory in ecstasy users are related to cognitive complexity of the task. Psychopharmacology. 2010;209:51–67. doi: 10.1007/s00213-009-1766-2. [DOI] [PubMed] [Google Scholar]
- Budka H. Acta Neuropathologica. Vol. 79. Berlin: 1990. Human immunodeficiency virus (HIV) envelope and core proteins in CNS tissues of patients with the acquired immune deficiency syndrome (AIDS) pp. 611–619. [DOI] [PubMed] [Google Scholar]
- Burgess PW, Gonen-Yaacovi G, Volle E. Functional neuroimaging studies of prospective memory: What have we learnt so far? Neuropsychologia. doi: 10.1016/j.neuropsychologia.2011.02.014. (in press). [DOI] [PubMed] [Google Scholar]
- Carey CL, Woods SP, Rippeth JD, Heaton RK, Grant I The HNRC Group. Prospective memory in HIV-1 infection. Journal of Clinical and Experimental Neuropsychology. 2006;28:536–548. doi: 10.1080/13803390590949494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L, Ernst T, Leonido-Yee M, et al. Perfusion MRI detects RCBF abnormalities in early stages of HIV-cognitive motor complex. Neurology. 2000;54:389–396. doi: 10.1212/wnl.54.2.389. [DOI] [PubMed] [Google Scholar]
- Chang L, Ernst T, Speck O, et al. Additive effects of HIV and chronic methamphetamine use on brain metabolite abnormalities. American Journal of Psychiatry. 2005;162:361–369. doi: 10.1176/appi.ajp.162.2.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman LJ, Chapman JP. The measurement of differential deficit. Journal of Psychiatric Research. 1973;14:303–311. doi: 10.1016/0022-3956(78)90034-1. [DOI] [PubMed] [Google Scholar]
- Costa A, Peppe A, Caltagirone C, Carlesimo GA. Prospective memory impairment in individuals with Parkinson’s disease. Neuropsychology. 2008;22:283–292. doi: 10.1037/0894-4105.22.3.283. [DOI] [PubMed] [Google Scholar]
- Culbertson WC, Zillmer EA. The Tower of London DX (TOL-DX) Manual. North Tonawanda, NY: Multi-Health Systems; 2001. [Google Scholar]
- Davis LE, Hjelle BL, Miller VE, et al. Early viral brain invasion in iatrogenic human immunodeficiency virus infection. Neurology. 1992;42:1736–1739. doi: 10.1212/wnl.42.9.1736. [DOI] [PubMed] [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, Ober BA. The California Verbal Learning Test. 2nd ed. San Antonio, TX: The Psychological Corporation; 2000. [Google Scholar]
- DiStephano M, Sabri F, Chiodi F. HIV-1 structural and regulatory proteins and neurotoxicity. In: Gendelman HE, Grant I, Everall IP, et al., editors. The Neurology of AIDS. 2nd ed. London: Oxford University Press; 2005. pp. 49–56. [Google Scholar]
- Einstein G, McDaniel M. Normal aging and prospective memory. Journal of Experimental Psychology: Learning, Memory, and Cognition. 1990;16:717–726. doi: 10.1037//0278-7393.16.4.717. [DOI] [PubMed] [Google Scholar]
- Einstein G, McDaniel M, Thomas R, Mayfield S, Shank H, Morrisette N, et al. Multiple processes in prospective memory retrieval: Factors determining monitoring versus spontaneous retrieval. Journal of Experimental Psychology: Applied. 2005;9:147–162. doi: 10.1037/0096-3445.134.3.327. [DOI] [PubMed] [Google Scholar]
- Einstein G, McDaniel M, Richardson S, Guynn M, Cunfer A. Aging and prospective memory: Examining the influences of self-initiated retrieval processes. Journal of Experimental Psychology: Learning, Memory and Cognition. 1995;21:996–1007. doi: 10.1037//0278-7393.21.4.996. [DOI] [PubMed] [Google Scholar]
- Ellis RJ, Calero P, Stockin MD. HIV infection and the central nervous system: a primer. Neuropsychology Review. 2009;19:144–151. doi: 10.1007/s11065-009-9094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis RJ, Langford D, Masliah E. HIV and antiretroviral therapy in the brain: neuronal injury and repair. Nature Reviews Neuroscience. 2007;8:33–44. doi: 10.1038/nrn2040. [DOI] [PubMed] [Google Scholar]
- Everall I, Vaida F, Khanlou N, Lazzaretto D, Achim C, Letendre S, Masliah E. Cliniconeuropathologic correlates of human immunodeficiency virus in the era of antiretroviral therapy. Journal of NeuroVirology. 2009;15:360–370. doi: 10.3109/13550280903131915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Scarano F, Martin-Garcia J. The neuropathogenesis of AIDS. Nature Reviews Immunology. 2005;5:69–81. doi: 10.1038/nri1527. [DOI] [PubMed] [Google Scholar]
- Heaton RK, Franklin DR, Ellis RJ, McCutchan JA, Letendre SL, Leblanc S the HNRC Group. HIV-associated neurocognitive disorders defore and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. Journal of NeuroVirology. 2010;17:3–16. doi: 10.1007/s13365-010-0006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kliegel M, Jager T, Altgasen M, Sum D. Clinical neuropsychology of prospective memory. In: Kliegel M, MecDaniel MA, Einstein GO, editors. Prospective Memory: Cognitive, Neuroscience, Developmental, and Applied Perspectives. New York, NY: Taylor & Francis Group/Lawrence Erlbaum Associates; 2008. pp. 283–308. [Google Scholar]
- Klove H. Grooved Pegboard. Lafayette, IN: Lafayette Instruments; 1963. [Google Scholar]
- Kuper M, Rabe K, Esser S, Gizewski ER, Husstedt IW, Maschke M, Obermann M. Structural gray and white matter changes in patients with HIV. Journal of Neurology. 2011;258:1066–1075. doi: 10.1007/s00415-010-5883-y. [DOI] [PubMed] [Google Scholar]
- Maki PM, Cohen MH, Weber K, Little DM, Fornelli D, Rubin LH, Martin E. Impairments in memory and hippocampal function in HIV-positive vs HIV-negative woman: a preliminary study. Neurology. 2009;72:1661–1668. doi: 10.1212/WNL.0b013e3181a55f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin EM, Nixon H, Pitrak DL, et al. Characteristics of prospective memory deficits in HIV-seropositive substance dependent individuals: Preliminary observations. Journal of Clinical and Experimental Neuropsychology. 2007;29:496–504. doi: 10.1080/13803390600800970. [DOI] [PubMed] [Google Scholar]
- Martin BA, Brown NL, Hicks JL. Ongoing task delays affect prospective memory more powerfully than filler task delays. Canadian Journal of Experimental Psychology – Revue Canadienne de Psychologie Experimentale. 2011;65:48–56. doi: 10.1037/a0022872. [DOI] [PubMed] [Google Scholar]
- McDaniel MA, Einstein GO. Strategic and automatic processes in prospective remembering: a multiprocess framework. Applied Cognitive Psychology. 2000;14:S127–S144. [Google Scholar]
- McDaniel MA, Einstein GO, Stout AC, Morgan Z. Aging and maintaining intentions over delays: Do it or lose it. Psychology & Aging. 2003;18:807–822. doi: 10.1037/0882-7974.18.4.823. [DOI] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Manual for the Profile of Mood States. San Diego: Educational and Industrial Testing Service; 1981. [Google Scholar]
- Mimura M, Kinsbourne M, O’Connor M. Time estimation by patients with frontal lesions and by Korsakoff amnesics. Journal of the International Neuropsychological Society. 2000;6:517–528. doi: 10.1017/s1355617700655017. [DOI] [PubMed] [Google Scholar]
- Psychological Corporation. WAIS-III and WMS-III technical manual. San Antonio, TX: Psychological Corporation; 1997. [Google Scholar]
- Psychological Corporation. Wechsler test of adult reading. Manual. San Antonio, TX: Author; 2001. [Google Scholar]
- Raskin S, Buckheit C, Sherrod C. MIST Memory for Intentions Test professional manual. Lutz, FL: Psychological Assessment Resources, Inc; 2010. [Google Scholar]
- Raskin SA, Sohlberg MM. The efficacy of prospective memory training in two adults with brain injury. Journal of Head Trauma Rehabilitation. 1996;11:32–51. [Google Scholar]
- Raskin SA, Woods SP, Poquette AJ, McTaggart AB, Sethna J, Williams RC, Troster AI. A differential deficit in time-versus event-based prospective memory in Parkinson’s disease. Neuropsychology. 2011;Vol. 25:201–209. doi: 10.1037/a0020999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger M, Welsh R, Razani J, Martin DJ, Boone KB. A meta-analysis of the neuropsychological sequelae of HIV infection. Journal of the International Neuropsychological Society. 2002;8:410–424. doi: 10.1017/s1355617702813212. [DOI] [PubMed] [Google Scholar]
- Reitan RM, Wolfson D. The Halstead-Reitan Neuropsychological Test Battery: Theory and clinical interpretation. Tucson, AZ: Neuropsychology Press; 1985. [Google Scholar]
- Smith GV, Della Sala S, Logie RH, Maylor EA. Prospective and retrospective memory in normal ageing and dementia: A questionnaire study. Memory. 2000;8:311–321. doi: 10.1080/09658210050117735. [DOI] [PubMed] [Google Scholar]
- Weinborn M, Woods SP, Nulsen C, Park K. Prospective memory deficits in ecstacy users: Effects of longer ongoing task delay interval. Journal of Clinical and Experimental Neuropsychology. 2011;33:1119–1128. doi: 10.1080/13803395.2011.614595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkie FL, Goodkin K, van Zuilen MH, Tyll MD, Lecusay R, Edwin T. Cognitive effects of HIV-1 infection. CNS Spectrum. 2000;5:33–51. doi: 10.1017/s1092852900013249. [DOI] [PubMed] [Google Scholar]
- Woods SP, Carey CL, Moran LM, Dawson MS, Letendre SL, Grant I the HIV Neurobehavioral Research Center (HNRC) Group. Frequency and predictors of self-reported prospective memory complaints in individuals infected with HIV. Archives of Clinical Neuropsychology. 2007;22:187–195. doi: 10.1016/j.acn.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods SP, Dawson MS, Weber E, Gibson S, Grant I, Atkinson JH The HIV Neurobehavioral Research Center (HNRC) Group. Timing is everything: Antiretroviral non-adherence is associated with impairment in time-based prospective memory. Journal of the International Neuropsychological Society. 2009;15:42–52. doi: 10.1017/S1355617708090012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods SP, Dawson MS, Weber E, Grant I The HNRC Group. The semantic relatedness of cue-intention pairings influences event-based prospective memory failures in older adults with HIV infection. Journal of Clinical and Experimental Neuropsychology. 2010;32:398–407. doi: 10.1080/13803390903130737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods SP, Iudicello JE, Moran LM, *Carey CL, Dawson MS, Grant I The HNRC Group. HIV-associated prospective memory impairment increases risk of dependence in everyday functioning. Neuropsychology. 2008;22:110–117. doi: 10.1037/0894-4105.22.1.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods SP, Moran LM, Carey CL, Dawson MS, Iudicello JE, Gibson S The HIV Neurobehavioral Research Center (HNRC) Group. Prospective memory in HIV infection: Is “remembering to remember” a unique predictor of self-reported medication management? Archives of Clinical Neuropsychology. 2008;23:257–270. doi: 10.1016/j.acn.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods SP, Moran LM, Dawson MS, Carey CL, Grant I The HNRC Group. Psychometric characteristics of the Memory for Intentions Screening Test. The Clinical Neuropsychologist. 2008;22:864–878. doi: 10.1080/13854040701595999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods SP, Scott JC, Dawson MS, Morgan EE, Carey CL, Heaton RK The HIV Neurobehavioral Research Center (HNRC) Group. Construct validity of Hopkins Verbal Learning Test-Revised component process measures in an HIV-1 sample. Archives of Clinical Neuropsychology. 2005;20:1061–1071. doi: 10.1016/j.acn.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Woods SP, Weber E, Weisz BM, Twamley EW, Grant I. Prospective memory deficits are associated with unemployment in persons living with HIV infection. Rehabilitation Psychology. 2011;56:77–84. doi: 10.1037/a0022753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Geneva, Switzerland: World Health Organization; 1998. Composite International Diagnostic Interview (CIDI, version 2.1) [Google Scholar]
- Zogg J, Woods SP, Doyle K, Weber E, Grant I The HNRC Group. Are time- and event-based prospective memory comparably affected in HIV infection? Archives of Clinical Neuropsychology. 2011;26:250–259. doi: 10.1093/arclin/acr020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zogg JB, Woods SP, Weber E, Iudicello J, Dawson MS, Grant I The HNRC Group. HIV-associated prospective memory impairment in the laboratory predicts failures on a semi-naturalistic measure of health care compliance. The Clinical Neuropsychologist. 2010;24:945–962. doi: 10.1080/13854046.2010.501343. [DOI] [PMC free article] [PubMed] [Google Scholar]