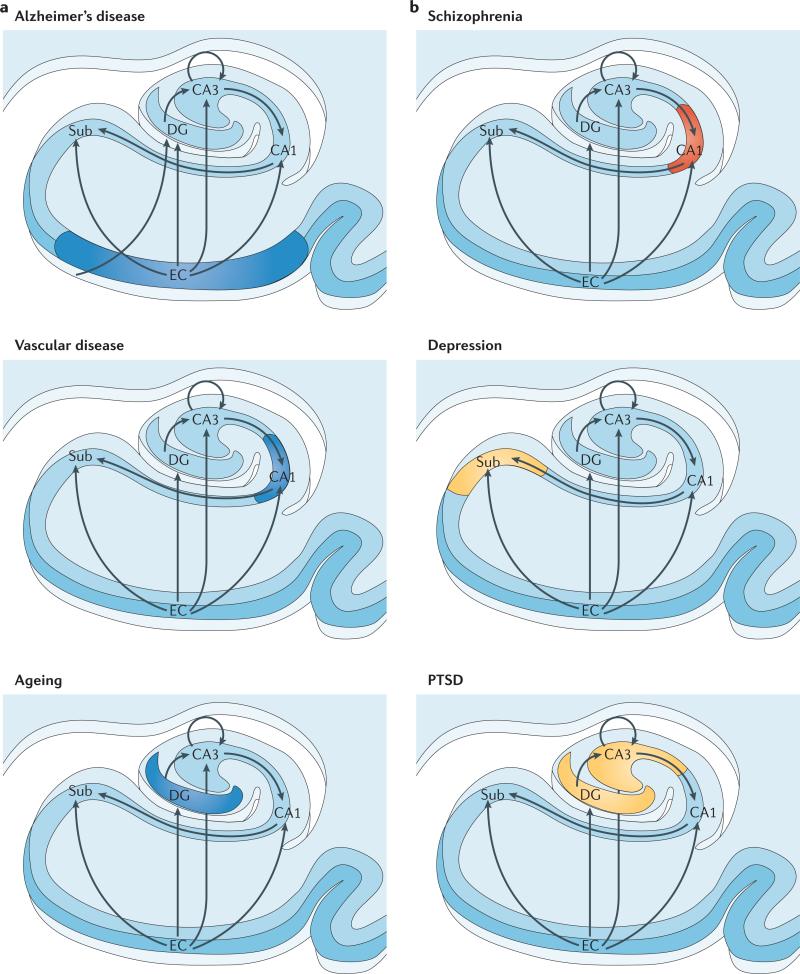
Figure 2. Regional vulnerability and metabolic state differentiate disorders that affect the hippocampal formation.
Although multiple hippocampal subregions can be affected in disorders, by comparing patterns of alterations that are observed by functional and structural MRI it is possible to isolate individual subregions differentially affected by each disorder. Furthermore, functional imaging techniques that are sensitive to metabolic state have suggested that some hippocampus-based disorders are characterized by hypometabolism (shown in blue), whereas others are abnormally hypermetabolic (shown in red). a | Alzheimer's disease, vascular disease and ageing all contribute to hippocampal alterations in late life. A direct comparison suggests that the entorhinal cortex (EC) is differentially associated with Alzheimer's disease and the CA1 with vascular disease, whereas the ageing process per se seems to differentially target the dentate gyrus (DG). Hypometabolism has been localized to the EC in Alzheimer's disease, to CA1 in vascular disease and the DG in ageing. b | Schizophrenia and depression typically begin during adolescence, and post-traumatic stress disorder (PTSD) currently has its highest incidence in young adulthood. A direct comparison suggests that CA1 is differentially associated with schizophrenia and that the subiculum (Sub) may be differentially associated with depression. In the case of PTSD, both CA3 and the DG have been implicated. Evidence for global hippocampal hypermetabolism exists for both schizophrenia and depression. In schizophrenia, this hypermetabolism may be driven by hypermetabolism in CA1, whereas subicular hypermetabolism in depression is a hypothesis that remains untested (shown in yellow). In PTSD the metabolic state of the hippocampal formation is as yet undetermined (shown in yellow).