Abstract
Organs are composed of parenchymal cells that characterize organ function and nonparenchymal cells that are composed of cells in transit, as well as tissue connective tissue, also referred to as tissue stromal cells. It was originally thought that these tissue stromal cells provided only structural and functional support for parenchymal cells and were relatively inert. However, we have come to realize that tissue stromal cells, not restricted to in the thymus and lymphoid organs, also play an active role in modulating the immune system and its response to antigens. The recognition of these elements and the elucidation of their mechanisms of action have provided valuable insight into peripheral immune regulation. Extrapolation of these principles may allow us to utilize their potential for clinical application. In this article, we will summarize a number of tissue stromal elements/cell types that have been shown to induce hyporesponsiveness to transplants. We will also discuss the mechanisms by which these stromal cells create a tolerogenic environment, which in turn results in long-term allograft survival.
Keywords: allogeneic, hepatic stellate cell, immunosuppression, mesenchymal stem cell, Sertoli cells, tolerance
The immune system consists of a highly diverse set of cells that all interact in a complex and intricate network, all in an attempt to protect the human body from pathogen invasion while maintaining nonreactivity to self. Over the last few decades, our understanding of immunology has allowed transplantation to flourish. Between the years 1999 and 2007, there was a 57% increase in the number of people living with transplanted organ [1]. Advances in immunosuppression have undoubtedly facilitated short- and long-term successes [2]. Nevertheless, the nonspecificity of immunosuppressants and the concern of the complications related to their use dictates that the physician must find a balance between the risk of rejection and loss of graft or an increased risk of malignancies and opportunistic infections. The holy grail is to try to achieve donor-specific unresponsiveness without the need for chronic immunosuppressants; that is, the ability to accept the donor organ permanently while retaining the ability to respond to and destroy pathogens.
Tolerance does not naturally pertain to transplantation, although it is a necessary aspect of the normally functioning immune system. When immune homeostasis goes awry, the end result is often the development of autoimmune disease. The mechanisms of tolerance can generally be divided into central tolerance and peripheral tolerance.
T cells, which express T-cell receptors (TCRs), are first positively selected for their ability to recognize self-MHC antigens and subsequently, those that have a high affinity for self-antigens are subject to negative selection/clonal deletion [3]. This process of central tolerance by which T cells undergo deletion within the thymus is thought to lead to clonal elimination. Inevitably, there are T cells that escape this negative selection process or those becoming autoreactive after leaving the thymus and therefore peripheral tolerance is felt to play a critical role in limiting the possibility for subsequent autoimmune disorders. In organ transplantation, physicians attempt to manipulate the recipient immune system such that it recognizes the allograft as self, while preserving responsiveness to harmful pathogens.
Historically, the stromal cell components of the immune system have not received much attention, although their role in maintaining a normal functioning immune system has been appreciated. Indeed, stromal cells in the thymus play an important role in the induction of central tolerance. A specialized group of thymic stromal cells – cortical thymic epithelial cells (cTECs) and medullary thymic epithelial cells (mTECs) – plays an integral role in the selection of T cells. cTECs promote the survival (positive selection) of immature double-positive (DP) CD4+CD8+ thymocytes that carry TCRs capable of interacting with self-MHC molecules. Interactions between the TCRs of DP thymocytes and MHC class I (MHC-I) or MHC class II (MHC-II) molecules expressed by cTECs direct differentiation of the DP thymocytes into single-positive CD8+ or CD4+ thymocytes, respectively. One of the most crucial functions of mTECs is to promote the elimination (negative selection) of autoreactive single-positive thymocytes, which carry TCRs that exhibit high affinity for self-antigen–MHC complexes [4]. In addition, mTECs have also been implicated in the development of natural Tregs [5,6].
A role for stromal cells has also been demonstrated during lymphoid organ development and function. They contribute to the immune response through the provision of chemokine and cytokines synthesis, as well as by acting as a scaffold for cell trafficking. For example, it was once thought that the fibroblastic reticular cells (FRCs) found in the lymph nodes only played a role in maintaining the structural integrity of the node; however, recent evidence indicates that the cells that constitute the FRCs form conduits that are responsible for the transport of cytokines from the afferent lymph to high endothelial venules [7]. This finding was further supported by evidence that FRCs create trafficking routes for lymphocytes, chemokines and antigens to be rapidly delivered to T-cell zones thus allowing for more efficient T-cell activation [8]. These data clearly illustrate that the nonhematopoietic stromal cells play a vital role in maintaining the normal and appropriate functioning of the immune response. Perhaps most intriguingly, there have been a number of studies that demonstrated the ability of stromal cells to directly affect the immune response. FRCs express the inhibitory ligand, PD-L1, which is critical in the downregulation of the immune response to antigens that can result in overstimulation of the immune system [9]. Not only have these cells been shown to be critical in dampening the immune response, there is evidence that they are also able to express the autoimmune regulator (Aire) gene, suggesting a role in maintaining peripheral tolerance by deletion of autoreactive cells [10].
We have now come to realize that the impact of stromal cells on the functioning of the immune system is more far reaching than that mentioned above. Interestingly, stromal cells from nonlymphoid organs also play a critical role in regulating the immune response in very profound ways. Stromal cells such as the Sertoli cell (SC), hepatic stellate cell (HpSC) and the mesenchymal stem cell (MSC) have shown significant promise in their ability to negatively regulate the immune response thus providing the tolerogenic environment needed for survival of transplanted grafts. For the remainder of the review, attention will be focused on these cells and their potential role in transplantation.
Sertoli cells
Perhaps the earliest studied of all nonlymphoid stromal cells are SCs. The testis has been recognized for its immune privileged status; antigens circulating within the testes are shielded from immune attack and destruction. This is an important physiologic phenomenon because at the site of spermatogenesis, developing germ cells express antigens that may be recognized as foreign and hence subject to an immune attack [11,12]. The principal cells primarily responsible for mediating immune privilege status are SCs. These cells function primarily as nurse cells – not only protecting germ cells from immune destruction but also providing numerous factors necessary for spermatogenesis [13]. Based on this characteristic of SCs, such as being able to protect germ cells from immune attack, it has been postulated that they should also have the ability to protect nontesticular grafts in the setting of transplantation [14].
SCs can protect allogeneic islet of Langerhans
Early studies exploring the function of SCs focused on the engraftment of allogeneic islet cells into the testes of guinea pigs. While the authors noted improved survival of the allografts, it was unclear at the time that the SCs were the cell type primarily responsible for conferring this protective effect [15,16]. Once it was determined that the SC was indeed the cell responsible for the observed tolerogenicity, studies evolved to cotransplantation of isolated SCs and tissues of interest. The protective ability of SCs has also been demonstrated in other species, including rats and monkeys, as well as different tissues such as parathyroid [17] and skin [18]. Many of these studies used islet–SC cotransplants injected under the renal capsule. In 1993, Selawry et al. demonstrated that cotransplantation of SCs with allogeneic islets resulted in extended survival of the islets albeit with a 3-day course of cyclosporine immediately post-transplant [19]. Subsequent improvements in the methods of isolation of SCs led to 100% survival of cotransplanted islets for more than 100 days postoperatively. More importantly, this improvement in survival was achieved without the use of immunosuppressive drugs [20]. It has been suggested that the formation of tubule-like structures alongside the islet allografts is necessary for long-term graft survival [21]. It has long been postulated that the tubule-like structure formed by SCs have tight junctions between themselves thus forming a physical barrier around transplanted allografts, protecting them from effector cell invasion and destruction. While this is an attractive proposition, there is also evidence to suggest that this may not be true. Histological assessment of long-term survivors has demonstrated that while the tubular structure may be necessary for long-term survival, the cotransplanted islet grafts were not found sequestered inside the tubules. In addition, a recent study showed that intravenous (iv.) infusion of SCs were able to prolong the survival of islets injected under the renal capsule of rats [22]. Subsequent histological analysis of long-term survivors did not reveal any islets surrounded by tubules. It has been assumed that SCs need to be polarized in the correct orientation, which in turn promotes the secretion of factors responsible for both SCs survival and immunoprotection.
SCs improve the survival of xenogeneic islet grafts
In addition to the unsavory effects of life-long immunosuppression, the shortage of transplantable tissue/organs is clearly one of the significant limiting factors in transplantation. While controversial, the ability to successfully transplant organs from one species to another will go a long way to alleviate the problem of organ shortage. Nevertheless, the immune barriers to acceptance of xenografts is regarded as more challenging than for allografts.
In light of this, there have been many studies that have shown that SCs can also protect xenogeneic grafts. There have been a number of reports that have shown that SCs can prolong the survival of xenogeneic skin grafts [23], neurons [24], adrenal chromaffin cells [25] and islet cells [26]. It must, however, be noted that some of the studies with xenogeneic tissue used encapsulation or short immunosuppressive therapy.
Studies have also shown that not only can syngeneic SCs provide immune protection but also xenogeneic SCs. For the same reasons mentioned above, this is an important finding as it facilitates obtaining the necessary tissue for potential clinical use. Yin et al. was able to demonstrate a significant improvement in the survival of allo-islet cells of rats using SCs from pigs. This study also showed that the mechanisms responsible for tolerance was likely to be independent of Fas ligand (FasL) as the SCs used did not express FasL [27].
Taken together, these data suggest that SCs appear to have the ability to extend their immunosuppressive effects even across a robust immunological barrier. Furthermore, the successful use of xenogeneic SCs demonstrates that their self-protecting ability is not species dependent.
Systemic tolerance induction by SCs
Perhaps the most intriguing suggestion and the one that holds the most promise for broad human application is evidence that SCs have the ability to induce systemic tolerance. Shamekh et al. was able to show that C57/BL6 mice injected with rat SCs through the lateral tail vein tolerated rat skin grafts significantly longer than control non-SC-transplanted mice, while maintaining a competent humoral response [28]. Recently, Li et al. was also able to demonstrate that iv. infusion of SCs prolonged the survival of islet cells in the absence of immunosuppressive therapy. The authors injected rats with SCs through the tail vein followed by implantation of islet cells beneath the renal capsule. The control group had no SC infusion. The results demonstrated that the experimental group had a mean survival time of 41.6 days while the control was only 7.4 days (p < 0.05). Six days post-transplantation, the long-term survivors had a significantly lower amount of CD4+ cells when compared with the control group (15.6 vs 48.6%, respectively). The same pattern was observed for CD8+ T cells. The authors also provided evidence to show that not only did SC infusion affect the T-cell composition; it also affected the cytokine profile of the animals; at 6 days postoperative, IL-2 and IFN-γ were significantly lower in the experimental group compared with the controls of islet only. Interestingly, in the early postoperative period, IL-4 patterns were opposite from those was observed with IL-2 and IFN-γ. They also demonstrated that the protective effect of SCs was reversed with addition of anti-FasL antibody and anti-TGF-β1 antibody, implying that both FasL and TGF-β1 play an important role in tolerance induction [29].
Not all of the results, however, have been positive; in fact, Lim et al. were unable to show a survival difference in cardiac allografts that were pretransplanted with immortalized neonatal porcine SCs (NPSCs). Despite this finding, there were some very interesting findings from that study: despite no statistical difference in the survival of the cardiac allografts, mixed lymphocyte reaction (MLR) assays of lymphocytes isolated from rats that were pretreated with NPSCs showed significant suppression against allogeneic splenocytes. The authors also demonstrated that there was a shift in the cytokine profile from Th1 to Th2 in lymphocytes exposed to NPSCs. These data seem to indicate that SCs have the potential to dampen T-cell responses. It also raises the question of why there was then no improvement in the survival of the cardiac allograft that were pretransplanted with immortalized NPSCs. Interestingly, the addition of cobra venom factor improved the survival of the cardiac allografts in the setting of pretreatment with NPSCs. Cobra venom factor is well known for its ability to activate the alternative pathway with the generation of C3a and C5a, thus resulting in the inhibition of the complement system [30]. In providing an explanation for this interesting phenomenon, it has been hypothesized that in vascularized grafts during the immediate post-transplantation period, humoral factors play a critical role and, as such, the ‘cellular immunomodulators’, NPSCs, are not capable of prolonging survival by themselves [31].
SCs can prolong the survival of islets in the setting of Type 1 diabetes: implications in autoimmune disorders
The role of SCs has not only been explored in the setting of transplantation; in fact, studies have also shown very promising results in Type 1 diabetes. Suarez-Pinzon et al. isolated and purified SCs from the testes of non-obese diabetic (NOD) mice and implanted them with syngeneic islets into the right renal capsule of diabetic NOD mice. After 60 days, 64% (nine out of 14) remained normoglycemic compared with none in the group with islets only [32]. More recently, SC-coated microcapsules were injected into the peritoneal cavity of NOD mice. In the group of mice that were already overtly diabetic, 81% had a reversion of their diabetes and became long-term survivors (>120 days). The control population had 100% disease progression with death occuring between 28 and 60 days. The authors noted that if the mice were injected with the SC-coated microcapsules before they were overtly diabetic, 88% never became diabetic [33].
While it is out of the scope of this review, it is important to note that SCs have shown some promise in other diseases that have some degenerative/inflammatory components to its pathophysiology. Sanberg et al. and Luca et al. have both demonstrated that SCs are able to provide some modulatory effects on disease models of amyotropic lateral sclerosis and Parkinson’s disease [25,34]. Also, in an experimental model of Huntington’s disease, the authors concluded that the beneficial effects of SC therapy were similar to that obtained by the use of systemic NSAIDs [35].
Large-animal & human studies with SCs
One of the early studies with large animals was performed in three diabetic male rhesus monkeys. Their testes were moved into the abdominal cavity and allogeneic islets were transplanted into them. The three monkeys returned to normoglycemia for >6 months; in fact, two out of three survived for 54 and 60 months each. The study confirmed that the transplanted islets were responsible for the normoglycemia by performing an orchiectomy and observed rapid return of the diabetic state. Of note, all three monkeys were given an initial brief immunosuppressive course [36].
The largest published clinical trial took place in 2005 in 12 adolescent Type 1 diabetic patients. Two collagen-generating devices were implanted subcutaneously in the upper anterior wall of the patient’s abdomen and left for 2 months to allow for the formation vascularized collagen tissue. After 2 months, 250,000 neonatal porcine islets with 30–100 SCs per islet were infused into one of the devices. Both the islet cells and SCs utilized in this study came from neonatal pigs. Throughout the study, none of the participants received immunosuppressive therapy. A total of 50% of recipients of porcine islets significantly reduced their requirements for exogenous insulin, with two patients achieving transient insulin independence. This was in stark contrast to the control group (no transplant). Using HPLC, porcine insulin was detected at the 4-year time point in two of the patients [37].
While this study perhaps has potential and shows some promise, it may be difficult to draw any significant conclusions given that the experimental design did not include an islet-only group. The observed protection may have been from the physical shield provided by the collagen-generating device. A more extensive list of SC applications in transplantation is provived in Table 1.
Table 1.
In vivo use of Sertoli cells in transplantation.
| Animal | Model | Outcome | Ref. |
|---|---|---|---|
| Mouse | Mouse islets | Return to normoglycemia | [19,20] |
| Mouse | Rat islets | Prolonged graft survival | [34] |
| Mouse | Fish islets | Prolonged graft survival | [26] |
| Mouse | Skin grafts | Prolonged graft survival† | [28] |
| Mouse | Heart | Prolonged graft survival† | [31] |
| Rat | Adrenal chromaffin cells | Decrease in microglial response | [25] |
| Rat | Neurons | Decrease in microglial response | [24] |
| Beagle dogs | Porcine islet | No difference in Sertoli cell group vs immunosuppression group‡ | [130] |
| Human | Porcine islet | Reduction in exogenous insulin requirement at 4 years | [37] |
Systemic tolerance induced by intravenous administration of Sertoli cells.
Islets were placed intratesticular.
Mechanisms of SC immunosuppression
It is unclear as to the exact mechanism(s) that are responsible for the observed SC immunosuppression; however, it is important to note that analysis of the cellular infiltrate has revealed that rejected SC/islet cografts have a high number of CD4+ T cells, CD8+ T cells and macrophages; however, successful grafts are characterized by fewer CD4+ T cells and macrophages and very few CD8+T cells [21]. In another study by Li et al., the iv. systemic administration of SCs also led to the observation of decreased amounts of CD4+ and CD8+ T cells in the peripheral blood of mice with long-term islet survival [38]. While the exact mechanisms of this observation is not know, Selawry and De Secaris using in vitro studies, showed that SCs produced a soluble protein(s) that was able to inhibit the proliferation of both T and B lymphocytes. These cells appeared to have been arrested in the G1 phase of cell cycle with concomitant reduction in IL-2. The addition of exogenous IL-2 was not enough to overcome the inhibitory effect, suggesting that this inhibitory protein also blocked the IL-2 responsiveness of in vitro activated T cells [39,40].
The Fas–FasL pathway has also been submitted as a possible mechanism for the above-mentioned T-cell inhibition. In a study by Takeda et al., it was noted that wild-type SCs cotransplanted with allogeneic islets resulted in prolonged graft survival; however, allogeneic islets cografted with SCs isolated from donors lacking functional FasL and transplanted into wild-type mice or cografted with wild-type SC transplanted into mice with a defect in Fas were rejected in the same time frame as islets transplanted alone [41]. Confounding this observation is the fact that SCs have also been shown to produce protease inhibitor 9, a known inhibitor to granzyme B and Fas–FasL pathway [42,43]. Moreover, islets from mice transgenicly modified to express FasL did not protect endogenous or allogeneic islets from immune rejection [44]. This observation was corroborated by Kang et al. when he showed that not only is there no improved protection; in fact, there was increased lymphocytic infiltration leading to augmented graft destruction [45]. These discrepancies indicate that the mechanisms are still unclear and further investigation into the role of Fas–FasL is necessary for clarification.
It has also been postulated that TGF-β may play an important role in SC-induced immunosuppression. Mice that have undergone successful transplantation with SCs and allogeneic islets show a twofold increase in TGF-β expression compared with the control group. Blockage of TGF-β expression led to early graft rejection. Graft rejection was associated with an increase in IFN-α and decrease in IL-4 leading the authors to conclude that the TGF-β production by SCs led to a shift in lymphocyte differentiation from Th1 to Th2 [46].
Given the complexity of the immune response, it is fathomable to deduce that the mechanisms for immunosuppression by SCs are also probably complex. Continued work in this field is necessary to fully understand this complexity.
Hepatic stellate cells
Liver tolerance is a well-known phenomenon, which was first documented in the 1960s when it was noted that in pigs, some liver allografts were accepted across MHC mismatch without the need for any immunosuppressive therapy [47]. These experiments were replicated with similar results in other species including rats and mice [48]. It was also supported by the fact that the liver contributes to tolerance to the antigens delivered via the portal vein or an oral route [49]. Ongoing rejection of previously transplanted organs can be reversed by liver allografts and in patients who have undergone concomitant liver and lung or liver and kidney transplantation, an improved allograft survival of the nonliver graft has been observed [50]. Weaning immunosuppression has been attempted post-liver transplantation and in approximately 20% liver transplant recipients total immunosuppression freedom for at least 1 year was achieved [51]. These data along with other clinical observations such as the propensity of the liver to permit evolution of acute to chronic viral infections such as hepatitis B or C demonstrate that the liver as an organ does demonstrate tolerogenic features.
Liver tolerance is essential because the liver is continually exposed to numerous antigens, in particular food and microbial antigens from the gut [52]. If it were not for the liver’s ability to modulate the immune system, the constant exposure to these antigens will lead to an overactive innate and adaptive immune response. A constantly inflamed liver would more than likely be incompatible with life.
Studies have shown that while liver allografts are accepted spontaneously in many species, hepatocyte transplants are acutely rejected. The logical inference is to speculate that there are nonparenchymal components that may be responsible for the observed tolerance. In an attempt to determine these nonparenchymal elements, Yu et al. examined mouse liver nonparenchymal cells and noted that HpSCs have potent immune regulatory activity [53].
HpSCs make up approximately 15% of the total cell population within the liver. They are located in the subendothelial space adjacent to the basolateral surface of the hepatocyte. HpSCs are the major site of vitamin A storage within the body [54,55]. They have been extensively studied for their role in fibrogenesis and induction of cirrhosis. In fact, the activation of HpSCs has been deemed as the key event in fibrogenesis. Once activated by an insult, they become myofibroblastic and deposit extracellular matrix, leading to liver fibrosis [56].
As alluded to above, the HpSC has been shown to not only be intricately involved in fibrogenesis but it has also been shown to be the likely candidate responsible for the observed liver tolerance [53,57]. There have been a number of studies that have demonstrated that HpSCs have the ability to dampen the immune response. As mentioned previously, MHC-mismatched liver grafts are accepted spontaneously between many mouse strains. Qian et al. examination of T cells in spontaneously accepted liver allografts revealed prominent apoptotic cells dispersed throughout the nonparenchymal cell population. When acute liver allograft rejection was induced by administration of IL-2, apoptotic activity was reduced substantially [58]. In further investigations, Yu et al. was able to show that HpSCs inhibited the T-cell response elicited by allogeneic DCs. This inhibition was HpSC dose dependent. Interestingly, the authors went on to show that the inhibition was not secondary to inhibition of activation; instead, inhibition was secondary to T-cell apoptosis. CD4+ and CD8+ T cells were both susceptible to HpSC-induced apoptosis. B7-H1, a B7 family molecule that has been shown to negatively regulate T-cell responsess has also been shown to be upregulated on lipopolysaccharide (LPS) or IFN-γ-activated HpSCs. Blocking B7-H1 on HpSCs at least partially reversed the inhibitory effect of HpSC on T cells [53]. Based on these experiments, one can conceptualize in the setting of inflammation/transplantaion (increased IFN-γ or LPS exposure), HpSCs upregulate the expression B7-H1 leading to T-cell apoptosis and thus induction of a tolerogenic environment.
Another example that illustrates the immune modulatory ability of the HpSC was demonstrated in a study by Chen et al. in which the authors were able to show in a graft-versus-host disease (GVHD) mouse model, HpSCs were able to improve survival. Mice cotransplanted with HpSCs experienced less diarrhea and weight loss and improved their mean survival from 15.3 ± 5.2 days to 57.5 ± 30.6 days [59].
The most profound evidence that has demonstrated the ability of HpSC to modulate the immune response utilized a model of syngeneic HpSCs cotransplanted with islet allografts. The authors demonstrated that six of 11 mice that received islet allografts plus HpSC remained euglycemic. In the control group, such as those that received islets only, all became diabetic by 17 days [60]. Immunohistochemical analysis of successful grafts revealed two interesting observations:
Transplanted HpSC were shown to deposit a matrix around the islets that consisted of α-smooth muscle actin, which encapsulated the graft and appeared to form a protective barrier around the islets;
The graft showed a paucity of infiltrating lymphocytes, both CD4 and CD8.
Furthermore, terminal deoxynucleotidyl transferase dUTP nick-end labeling staining of the cotransplanted islet (TUNEL) + HpSC graft revealed an increased amount of apoptotic mononuclear cells when compared with islet only. Mechanistically, these data lend credence to the hypothesis that HpSC-induced tolerance may be due to both the provision of a physical barrier thus limiting the infiltration of mononuclear cells and also deletion of T cells. Further support of the ‘deletion theory’ was provided by experiments in which B7-H1−/− HpSCs were cotransplanted with islets. The results demonstrated that the mice lost their ability to protect the islet allografts from rejection. These results closely mimic the protection of islet allografts reported in studies of cotransplantation of SCs mentioned earlier. However, in contrast to the ability of xenogeneic and allogeneic sertolic cells to modulate rejection, the use of allogeneic HpSC (in contrast to syngeneic HpSC) appeared to be unable to provide a statistically significant prolongation of islet allograft survival. It must also be noted that syngeneic HpSCs were unable to induce systemic tolerance as demonstrated by the finding that cotransplantation of HpSC and islet allograft into the right renal capsule and islet allograft only into the left followed by right nephrectomy did not maintain euglycemia, illustrating another significant difference between SCs and HpSCs [60].
It would perhaps be naive to believe that it is only through the above-mentioned mechanism that HpSCs are able to modulate the immune response. In fact, recent evidence suggests that HpSCs are also able to preferentially expand allogeneic CD4+CD25+FoxP3+ Tregs. Allogeneic CD4+ T cells were isolated and cocultured in vitro with IFN-γ-treated HpSCs. The results demonstrated that the percentage of Tregs increased by >100% compared with the control group. Interestingly, the authors were able to demonstrate that the increase in the number of Tregs was not secondary to the induction of new ones; instead, it was probably due to expansion of already existing Tregs. These data were backed by evidence that HpSCs are able to increase Treg levels in vivo. In a study by Jiang et al. lymphocytes were isolated from the draining lymph nodes on postoperative day 7 as well as from survivors >90 days. Mice that underwent no transplantation and islet allografts only were used as controls. The results demonstrated that there was a significantly elevated number of CD4+CD25+FoxP3+ Tregs in the draining lymph node of the mice that exhibited long-term graft survival. These combined in vitro and in vivo data suggest that with the ability of activated HpSCs to expand the population of Tregs, an ensuing shift in the local environment to a more tolerogenic phenotype allows for long-term survival of islet allografts without the need for immunosuppression [61].
The role of myeloid-derived suppressor cells (MDSCs) in transplantation has been recently coming to light [62]. These cells represent a heterogeneous population of immature myeloid cells that consists of myeloid progenitors characterized by a strong ability to suppress T-cell functions [63]. Most of the data on MDSCs have come from oncology literature where it has been shown that these cells accumulate in cancer patients and function to help neoplasm evade immune surveillance. Recently, however, Chou et al. demonstrated that HpSCs are able to promote tolerance through the induction of MDSCs in an allo-islet transplant model. HpSC-induced MDSCs demonstrated potent immune inhibitory activity. The authors showed that the induction of MDSC is dependent on an intact IFN-γ signaling pathway in HpSCs and that their induction is mediated by soluble factors produced by HpSCs. Perhaps most relevant to possible human application is the fact that the authors demonstrated that large amounts of MDSC can be propagated in vitro from bone marrow-derived myeloid precursor cells under the influence of HpSC [64].
While HpSCs have shown a robust ability to be immunoregulatory, they have reduced flexibity when compared with SCs especially when one considers cell availability and alloreactivity. Their recent role in the induction of MDSC is one that holds tremendous promise however. While it is beyond the scope of this review to look at MDSCs in transplantation, reviews on its use exist [65].
Mesenchymal stem cells
In the recent past, MSCs have received considerable attention for their therapeutic potential in tissue regeneration and repair. MSCs can be defined as pluripotent nonhematopoietic progenitor cells that are capable of differentiating into multiple lineages of mesenchymal origin. These lineages include bone, adipocytes, cartilage, muscle, neurons, islets and hepatocytes [66]. While the initial work done on MSCs came from cells isolated from the bone marrow, several other MSCs from varying sources have been shown to possess similar immunosuppressive abilities. These sources include adiopose tissue [67–70], cord blood [71–73], peripheral blood [74–75] and amniotic fluid [76–78]. In addition to their role in tissue regeneration and repair, there is substantial evidence that supports the notion that MSCs play a critical role in immune modulation.
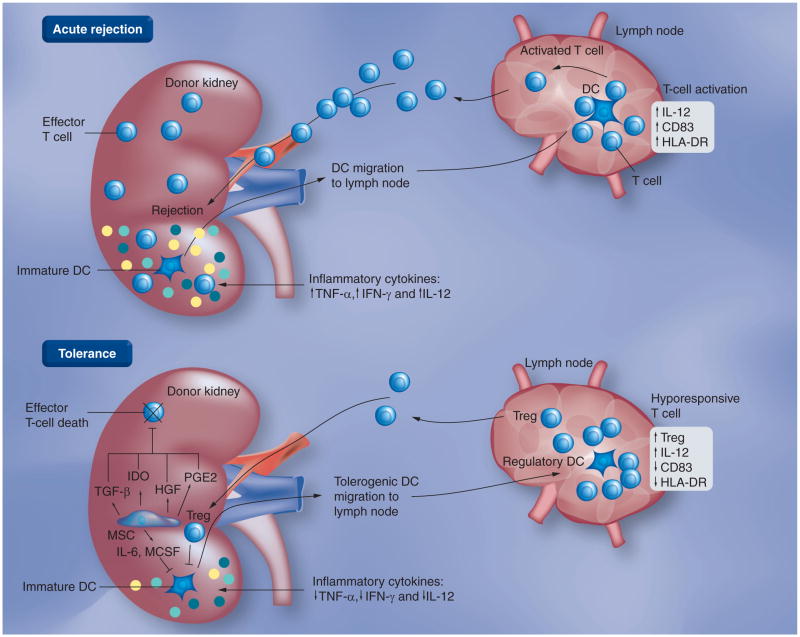
The use of MSCs in transplantation came from observations in which it was noted that MSCs were able to suppress T lymphocyte activation and proliferation in vitro and has been demonstrated in a number of species including rodents, baboons and humans [79–85]. In addition to their ability to suppress T-cell proliferation, there is evidence to show that MSC influences on the immune system is multidimensional, ranging from the induction of Th2 responses to upregulation of Tregs to the inhibitory effects on maturation of dendritic cells [86–91]. Mechanistically, by using transwell experiments, most studies have concluded that cell–cell contact is not needed for T-cell suppression [92]. As demonstrated in Figure 1, several soluble factors have been identified as probable candidates responsible for this phenomenon. These include:
Figure 1. Direct pathway of rejection and the possible mechanisms by which mesenchymal stem cells are able to protect grafts.
DC: Dendritic cell; IDO: Indoleamine 2,3-dioxygenase; MCSF: Macrophage colony stimulating factor; MSC: Mesenchymal stem cell. Reproduced with permission from Cleveland Clinic Center for Medical Art & Photography © 2011. All rights reserved.
Indoleamine 2,3-dioxygenase (IDO): IDO is an enzyme that forms the rate-limiting step in tryptophan metabolism. When cells produce an excess of IDO, it leads to tryptophan consumption. This is notable because tryptophan starvation results in inactivation of T cells. Available evidence also indicates that build-up of products (as it occurs with the excessive production of IDO) of tryptophan metabolism such as kynurenine derivatives and O2-free radicals serve to regulate T-cell proliferation and survival [93–95]. Meisel et al. demonstrated that MSCs were able to inhibit allogeneic T-cell responses in vitro using mixed lymphocyte reaction and that the addition of exogenous tryptophan was able to significantly restore the allogeneic T-cell proliferation [96];
TGF-β: this secreted cytokine has been shown to be a potent immunosuppressive agent [97]. In a study carried out by Di Nicola et al., it was shown that neutralizing antibodies against TGF-β restored at least in part the proliferative ability of T cells in MLR [79];
Prostaglandin E2 (PGE2): inhibitors of pros-taglandin E2 have been shown to mitigate the antiproliferative effect of MSC in MLR [88].
On the other hand, there is also substantial evidence that seems to suggest that some of these very factors have a limited role at best [92,98]. It may also be fair to conclude that different T-cell stimulants, such as mitogens (ConA), allo-T cells, anti-CD3 and anti-CD28, activate different suppressive pathways that may explain the apparent contradictions in some of these studies [98]. Despite the conflicting data, MSCs are clearly able to modulate its host immune response [99]. These cells have been used both in murine and human treatment of GVHD and the outcomes have been favorable [100–101]. In additon, a number of investigators have demonstrated the ability of MSC to downregulate autoreactive T-cell responses in autoimmune diseases (Type 1 diabetes, collagen-induced arthritis or autoimmune colitis) [102–104]. The use of MSC in transplantation has yielded encouraging results.
Islet transplantation
In a study published by Ding et al., syngeneic MSCs cotransplanted with allogeneic islet cells under the renal capsule demonstrated that 100% of the mice (n = 6) remained normoglycemic long term (>90 days). This was in stark contrast to mice that were injected with islets only; they became overtly diabetic within 30 days. The authors went on to provide both in vitro and in vivo evidence that MMP-2 and MMP-9 secretion by MSCs were essential in maintaining the tolerogenic phenotype [104]. In another experiment by Li et al., the authors demonstrated that cotransplantation of allogeneic islets and MSCs also resulted in restoration of normoglycemia. They were able to show that within the peripheral blood of mice that had prolonged survival of the islet graft, the ratios of Th1:Th2 and Tc1:Tc2 were markedly reduced, in contrast to the increased ratio in mice that had no MSCs. The authors were also able to show that immature DCs derived from mice that underwent successful transplantation had little to no production of IL-12 after stimulation, in contrast to immature DCs generated from mice that rejected their allograft, where elevated IL-12 was demonstrated. Taken together, these data show the presence of MSC shifts the immune balance to a tolerogenic phenotype thorough mulitple mechanisms [105].
Skin allograft transplant
Bartholomew et al. looked at the ability of iv. administered MSC to protect skin transplants in MHC-mismatched recipient baboons. They noted that animals receiving iv. MSCs had their transplanted skin significantly increased survival to 11.3 ± 0.3 days, from 7 days in animals without MSC injection. Interestingly, third-party skin grafts had equal survival as the initial donor grafts, suggesting that the immunosuppressive effect was nonspecific [106].
Heart transplant
A study by Casiraghi et al. demonstrated that donor-derived MSC infusion into the portal vein 7 days before transplantation resulted in prolonged survival of semiallogeneic heart transplants (33% alive after 100 days) compared with mice not receiving MSC infusion into the portal vein (100% dead by day 13) [107]. A second iv. administration of MSC did not improve the survival of the semiallogeneic heart transplants. Interestingly, adoptive transfer of splenocytes from MSC-treated mice with >100-day survival to naive mice yielded prolongation of donor cardiac allograft. A second experiment was then performed in which the isolated splenocytes from long-term survivors were sorted into several subsets: CD8+ and CD4+ (CD4+CD25+ and CD4+CD25+). The individual subsets of T cells were then adoptively transferred into naive mice the day before transplantation and survival of the transplanted heart were then assessed. Mice that received the CD8+ cells acutely rejected within 15 days, CD4+CD25− mice showed modest prolongation in cardiac allograft survival but rejected within 38 days, whereas CD4+CD25+-infused mice had indefinite survival of their cardiac allograft. FACS analysis of the splenocytes demonstrated a more than two-fold increase in the number of CD4+CD25+FoxP3+ Tregs compared with naive mice. Taken together, these data provide strong evidence that MSCs are able to induce the formation of Tregs. These very cells are also responsible at least in part for the observed immune tolerance. Interestingly, however, it must be noted that syngeneic MSCs were unable to prolong fully allogeneic cardiac allograft survival [108].
Graft-versus-host disease
Perhaps the most comprehensively studied model of MSCs in transplantation comes from its use in the treatment of acute GVHD. GVHD is a known complication of allogeneic hematopoietic stem cell transplantation that can cause considerable morbidity and mortality. In clincial trials, MSCs were used to treat steroid-resistant GVHD. In their first series of patients with grades III–IV steroid-refractory acute GVHD, responses were seen in six out of eight patients; furthermore, improved survival was noted in patients treated with MSCs compared with ones not treated with MSCs during the same time period (p = 0.03) [101,108]. Because of the success of the study, a Phase II trial was initiated in which 55 patients with therapy-resistant acute GVHD were treated with MSCs [109]. Complete response was noted in 54% of patients while 16% had a partial response. Response rate was not related to MSC donor and recipient HLA match. Complete responders had an overall 2-year survival after MSC infusion of 52%, as opposed to 16% for partial and nonresponders (p = 0.018). Children tended to have a better response at 68% compared with 43% (p = 0.07) in adults [110]. Several other studies have been undertaken looking at MSC source, dosage and different serum for MSC expansion [111–116]. Consistently, MSCs were shown to provide complete or partial response in the majority of patients. Importantly, no adverse effects were noted during therapy with MSCs. Debate does exist regarding the occurrence of leukemic relapse [117]; however, more robust studies are needed to confirm any such link. In light of the in vitro immunosuppresive properties of MSC and early promising results with its use in GVHD, a consortium of experts in the field was put together to specifically take the use of MSC and apply it to the next level of therapy, solid organ transplantation. The Mesenchymal Stem Cells In Solid Organ Transplantation (MISOT) group has been charged with the responsibility of providing a forum for the discussion of basic science and clinical data that can then be used in the planning of clinical trials [118]. In their last meeting in 2010, the group evaluated several protocols that are being planned and ones that have already been initiated in clinical studies involving the use of MSC in human kidney and liver transplantation [119]. The results of these studies are sure to provide the transplantation community with invaluable data on the safety profile and the efficacy of these cells.
While the overwhelming majority of studies seem to indicate that MSCs are able to protect allografts from immune attack, there are some reports to the contrary. Sbano et al. attempted to use allogeneic MSCs for tolerance induction in a rat skin transplant model but noted that not only did MSC not protect the grafts, those groups also had accelerated rejection [120]. It must however be noted that the MSCs were delivered intravenously and not via the portal vein. That may provide the explanation for the lack of observed tolerance induction since Casiraghi et al, in the study above had similar results of rejection when MSC were delivered through the tail vein instead of the portal vein [107].
Placenta-derived stromal cells
Recent data have shown that placenta-derived stromal cells have similar abilities to modulate T-cell responses as does bone marrow-derived stromal cells (BM-MSCs). Several authors have shown that placenta-derived stromal cell suppress both mitogen-induced and allogeneic lymphocyte proliferation in both CD4 and CD8 populations [121–123]. In fact, Chang et al. further demonstrated that the immunosuppression observed with placenta-derived MSCs (PDMCs) was significantly stronger than that with BM-MSCs. The mechanisms of this immunosuppression has been shown to be multifactorial-decreased lymphocyte proliferation with concomitant increase in the number of Tregs partially mediated by IL-10 and TGF-β play a probable role [123]. Other studies have shown that cell–cell contact is necessary for suppression implicating an unknown surface molecule [122].
Consistent with reports of MSCs from other origins [124–127], PDMCs have also been shown to affect the differentiation of dentritic cells from peripheral blood monocytes [128]. Mechanistically, the authors showed that the presence of PDMCs in DC cultures resulted in their arrest in the G0 phase. They went on to show that there was also a loss in the production of inflammatory cytokines such as TNF-α, CXCL10, CXCL9 and CCL5.
Many authors have concluded that the immunosuppressive properties of PDMCs, along with their multilineage differentiation potential, ease of accessibility and abundant cell numbers, make them good potential sources for therapeutic applications. To date, a number of preclinical studies have been performed looking at the role of these cells in disease processes including Parkinson’s disease, stroke and Type 1 diabetes [129]. While these studies have shown significant promise on regenerative medicine, there are no studies looking at the efficacy of PDMCs in transplantation. Given the success of BM-MSC in transplantation, one can surmise that PDMCs ought to have significant potential in transplantation therapeutics.
Future perspective
Cellular-based immunotherapy shows significant promise as a potential treatment option for the induction of tolerance in transplantation. We have gone from in vitro bench studies in the 1970s to Phase II clinical trials using MSCs in the treatment of GVHD. We have yet to study the role of these stromal cells in human solid organ transplantation. The work done by the MISOT group is exciting and encouraging and soon we should be seeing their results.
It is of paramount importance that we realize that the application of stromal cells is not only limited to transplantation. With some foresight, one can appreciate its use in the development of new therapeutic strategies for chronic viral infections, autoimmune disease, cancer, among others. For example, the interaction of PD-1/PD-L1 has been shown to be important in HpSC-induced transplant tolerance. Work from these studies has led to the development of monoclonal antibody therapy against PD-1. This antibody is currently under Phase I clinical trials for cancer therapy and has been showing promising results. Moreover, the recent plethora of data on the role of MDSC in immune regulation are likely to have a profound impact on the future of transplantation. One of the keys to its success in therapy is whether the findings of efficient ex vivo production in mice can be replicated in human models. The long-term possible oncologic complications are unknown at this time and, as such, more research needs to be done to elucidate it. These studies are not only important in the development of novel immunotherapeutic approaches, they are also critical in providing insight into the mechanisms responsible for tolerance induction both in transplantation and cancer therapy.
Conclusion
In conclusion, the evidence is quite convincing that the above-mentioned stromal cells are able to modulate immune responses. Whether one population shows more promise will probably depend on the ability to provide and expand these populations of cells as well as the indication for treatment. Thus, more research needs to be done to bring this type of cellular therapy to the bedside.
Executive summary.
Sertoli cells
Nurse cells found in the testes support spermatogenesis and protect sperms from immune attack.
Sertoli cells (SCs) from several species including rats amd monkeys have been shown to protect allogeneic tissues. These tissue types include islets, parathyroid and skin, among others. The SC immune regulatory capability has been shown to be quite extensive. For example, their protective capabilities extend to xenogeneic models making their application quite versatile. Moreover, SCs have shown the ability to protect islets in a Type 1 diabetes model, signifying that they also have a role in protecting against autoimmune disorders.
Exact mechanisms by which SCs perform their immune-protective role are unclear; however, there is evidence supporting deletion of CD4+, CD8+ T cells and macrophages. The molecule(s) responsible for this observation is unknown but the addition of exogenous IL-2 was unable to recover T-cell inhibition. Other authors have shown that TGF-β production by SCs may also play a role in shifting the lymphocyte response from a Th1 to Th2 reaction.
Hepatic stellate cells
The hepatic stellate cell (HpSCs) is the main storage cell for vitamin A.
HpSCs are well known for their pivotal role in liver fibrosis/cirrhosis.
HpSCs have been recently shown to be an immune modulator by prolonging allogeneic islet survival.
Further evidence supporting the immune modulatory role of HpSCs has been demonstrated in a graft-versus-host disease mouse model in which HpSCs lowered the extent of diarrhea and weight loss and improved mean survival of mice.
HpSCs suppress both CD4+ and CD8+ T cells by induction of apoptosis through the costimulatory molecule B7-H1.
Both Tregs and myeloid-derived suppressor cells have been implicated in HpSC-induced immune regulation.
Mesenchymal stem cells
Mesenchymal stem cells have been studied extensively for their role in tissue regeneration and repair.
Immune suppressive characteristics have been shown in several species including rodents, baboons and humans.
Mesenchymal stem cells have been able to protect allogeneic islets, skin and heart in murine models.
These cells have been successfully used in treatment of graft-versus-host disease in humans and there are ongoing European trials looking at its use in transplantation.
Mechanisms include T-cell inhibition through indoleamine 2,3-dioxygenase and prostaglandin E2. The immunosuppressive effect of TGF-β has also been implicated.
Footnotes
For reprint orders, please contact: reprints@futuremedicine.com
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- 1.Wolfe RA, Roys EC, Merion RM. Trends in organ donation and transplantation in the United States, 1999–2008. Am J Transplant. 2010;10(4 Pt 2):961–972. doi: 10.1111/j.1600-6143.2010.03021.x. [DOI] [PubMed] [Google Scholar]
- 2.Kemmer N, Neff G. Recipient-based approach to tailoring immunosuppression in liver transplantation. Transplant Proc. 2010;42(5):1731–1737. doi: 10.1016/j.transproceed.2010.02.076. [DOI] [PubMed] [Google Scholar]
- 3.Parham P. Elements of the immune system and their roles in defense. In: Paul WE, editor. The Immune System. 2. Garland Science Publishing; NY, USA: 2005. pp. 1–34. [Google Scholar]
- 4.Irla M, Hollander G, Reith W. Control of central self-tolerance induction by autoreactive CD4+ thymocytes. Trends Immunol. 2010;31(2):71–79. doi: 10.1016/j.it.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Spence PJ, Green EA. Foxp3+ regulatory T cells promiscuously accept thymic signals critical for their development. Proc Natl Acad Sci USA. 2008;105(3):973–978. doi: 10.1073/pnas.0709071105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aschenbrenner K, D’Cruz LM, Vollmann EH, et al. Selection of Foxp3+ regulatory T cells specific for self antigen expressed and presented by Aire+ medullary thymic epithelial cells. Nat Immunol. 2007;8(4):351–358. doi: 10.1038/ni1444. [DOI] [PubMed] [Google Scholar]
- 7.Anderson AO, Shaw S. T cell adhesion to endothelium: the FRC conduit system and other anatomic and molecular features which facilitate the adhesion cascade in lymph node. Semin Immunol. 1993;5(4):271–282. doi: 10.1006/smim.1993.1031. [DOI] [PubMed] [Google Scholar]
- 8.Bajénoff M, Egen JG, Koo LY, et al. Stromal cell networks regulate lymphocyte entry, migration, and territoriality in lymph nodes. Immunity. 2006;25(6):989–1001. doi: 10.1016/j.immuni.2006.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mueller SN, Matloubian M, Clemens DM, et al. Viral targeting of fibroblastic reticular cells contributes to immunosuppression and persistence during chronic infection. Proc Natl Acad Sci USA. 2007;104(39):15430–15435. doi: 10.1073/pnas.0702579104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gardner JM, Devoss JJ, Friedman RS, et al. Deletional tolerance mediated by extrathymic Aire-expressing cells. Science. 2008;321(5890):843–847. doi: 10.1126/science.1159407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Rand MG, Romrell LJ. Appearance of cell surface auto- and isoantigens during spermatogenesis in the rabbit. Dev Biol. 1977;55(2):347–358. doi: 10.1016/0012-1606(77)90178-6. [DOI] [PubMed] [Google Scholar]
- 12.Tung PS, Fritz IB. Specific surface antigens on rat pachytene spermatocytes and successive classes of germinal cells. Dev Biol. 1978;64(2):297–315. doi: 10.1016/0012-1606(78)90080-5. [DOI] [PubMed] [Google Scholar]
- 13.Griswold MD. The central role of Sertoli cells in spermatogenesis. Semin Cell Dev Biol. 1998;9(4):411–416. doi: 10.1006/scdb.1998.0203. [DOI] [PubMed] [Google Scholar]
- 14.Mital P, Kaur G, Dufour JM. Immunoprotective Sertoli cells: making allogeneic and xenogeneic transplantation feasible. Reproduction. 2010;139(3):495–504. doi: 10.1530/REP-09-0384. [DOI] [PubMed] [Google Scholar]
- 15.Ferguson J, Scothorne RJ. Extended survival of pancreatic islet allografts in the testis of guinea-pigs. J Anat. 1977;124(Pt 1):1–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Ferguson J, Scothorne RJ. Further studies on the transplantation of isolated pancreatic islets. J Anat. 1977;124(Pt 1):9–20. [PMC free article] [PubMed] [Google Scholar]
- 17.Naji A, Barker CF. The influence of histocompatibility and transplant site on parathyroid allograft survival. J Surg Res. 1976;20(4):261–267. doi: 10.1016/0022-4804(76)90012-3. [DOI] [PubMed] [Google Scholar]
- 18.Whitmore WF, Gittes RF. Studies on the prostate and testis as immunologically privileged sites. Cancer Treat Rep. 1977;61(2):217–222. [PubMed] [Google Scholar]
- 19.Selawry HP, Cameron DF. Sertoli cell-enriched fractions in successful islet cell transplantation. Cell Transplant. 1993;2(2):123–129. doi: 10.1177/096368979300200206. [DOI] [PubMed] [Google Scholar]
- 20.Korbutt GS, Elliott JF, Rajotte RV. Cotransplantation of allogeneic islets with allogeneic testicular cell aggregates allows long-term graft survival without systemic immunosuppression. Diabetes. 1997;46(2):317–322. doi: 10.2337/diab.46.2.317. [DOI] [PubMed] [Google Scholar]
- 21.Dufour JM, Lord SJ, Kin T, et al. Comparison of successful and unsuccessful islet/Sertoli cell cotransplant grafts in streptozotocin-induced diabetic mice. Cell Transplant. 2008;16(10):1029–1038. [PubMed] [Google Scholar]
- 22.Li Y, Xue WJ, Tian XH, et al. Study on systemic immune tolerance induction in rat islet transplantation by intravenous infusion of Sertoli cells. Transplantation. 2010;89(12):1430–1437. doi: 10.1097/TP.0b013e3181da607e. [DOI] [PubMed] [Google Scholar]
- 23.Shamekh R, El-Badri NS, Saporta S, et al. Sertoli cells induce systemic donor-specific tolerance in xenogenic transplantation model. Cell Transplant. 2006;15(1):45–53. doi: 10.3727/000000006783982205. [DOI] [PubMed] [Google Scholar]
- 24.Willing AE, Sudberry JJ, Othberg AI, et al. Sertoli cells decrease microglial response and increase engraftment of human hNT neurons in the hemiparkinsonian rat striatum. Brain Res Bull. 1999;48(4):441–444. doi: 10.1016/s0361-9230(99)00023-4. [DOI] [PubMed] [Google Scholar]
- 25.Sanberg PR, Borlongan CV, Saporta S, Cameron DF. Testis-derived Sertoli cells survive and provide localized immunoprotection for xenografts in rat brain. Nat Biotechnol. 1996;14(13):1692–1695. doi: 10.1038/nbt1296-1692. [DOI] [PubMed] [Google Scholar]
- 26.Yang H, Wright JR., Jr Co-encapsulation of Sertoli enriched testicular cell fractions further prolongs fish-to-mouse islet xenograft survival. Transplantation. 1999;67(6):815–820. doi: 10.1097/00007890-199903270-00006. [DOI] [PubMed] [Google Scholar]
- 27.Yin Z, Chen D, Hu F, et al. Cotransplantation with xenogenetic neonatal porcine Sertoli cells significantly prolongs islet allograft survival in nonimmunosuppressive rats. Transplantation. 2009;88(3):339–345. doi: 10.1097/TP.0b013e3181ae5dcf. [DOI] [PubMed] [Google Scholar]
- 28.Shamekh R, El-Badri NS, Saporta S, et al. Sertoli cells induce systemic donor-specific tolerance in xenogenic transplantation model. Cell Transplant. 2006;15(1):45–53. doi: 10.3727/000000006783982205. [DOI] [PubMed] [Google Scholar]
- 29.Li Y, Xue WJ, Tian XH, et al. Study on systemic immune tolerance induction in rat islet transplantation by intravenous infusion of Sertoli cells. Transplantation. 2010;89(12):1430–1437. doi: 10.1097/TP.0b013e3181da607e. [DOI] [PubMed] [Google Scholar]
- 30.Lim HG, Lee HM, Oh BC, Lee JR. Cell-mediated immunomodulation of chemokine receptor 7-expressing porcine Sertoli cells in murine heterotopic heart transplantation. J Heart Lung Transplant. 2009;28(1):72–78. doi: 10.1016/j.healun.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 31.Leventhal JR, Sakiyalak P, Witson J, et al. The synergistic effect of combined antibody and complement depletion on discordant cardiac xenograft survival in non-human primates. Transplantation. 1994;57:974–978. [PubMed] [Google Scholar]
- 32.Suarez-Pinzon W, Korbutt GS, Power R, Hooton J, Rajotte RV, Rabinovitch A. Testicular Sertoli cells protect islet β-cells from autoimmune destruction in NOD mice by a transforming growth factor-β1-dependent mechanism. Diabetes. 2000;49(11):1810–1818. doi: 10.2337/diabetes.49.11.1810. [DOI] [PubMed] [Google Scholar]
- 33.Fallarino F, Luca G, Calvitti M, et al. Therapy of experimental Type 1 diabetes by isolated Sertoli cell xenografts alone. J Exp Med. 2009;206(11):2511–2526. doi: 10.1084/jem.20090134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luca G, Calvitti M, Nastruzzi C, et al. Encapsulation, in vitro characterization, and in vivo biocompatibility of Sertoli cells in alginate-based microcapsules. Tissue Eng. 2007;13(3):641–648. doi: 10.1089/ten.2006.0137. [DOI] [PubMed] [Google Scholar]
- 35.Emerich DF. Sertoli cell grafts for Huntington’s disease. An opinion. Neurotox Res. 2004;5(8):567. doi: 10.1007/BF03033176. [DOI] [PubMed] [Google Scholar]
- 36.Dufour JM, Rajotte RV, Korbutt GS, Emerich DF. Harnessing the immunomodulatory properties of Sertoli cells to enable xenotransplantation in Type I diabetes. Immunol Invest. 2003;32(4):275–297. doi: 10.1081/imm-120025106. [DOI] [PubMed] [Google Scholar]
- 37.Valdes-Gonzalez RA, Dorantes LM, Garibay GN, et al. Xenotransplantation of porcine neonatal islets of Langerhans and Sertoli cells: a 4-year study. Eur J Endocrinol. 2005;153:419–427. doi: 10.1530/eje.1.01982. [DOI] [PubMed] [Google Scholar]
- 38.Li Y, Xue WJ, Tian XH, et al. Study on systemic immune tolerance induction in rat islet transplantation by intravenous infusion of Sertoli cells. Transplantation. 2010;89(12):1430–1437. doi: 10.1097/TP.0b013e3181da607e. [DOI] [PubMed] [Google Scholar]
- 39.De Cesaris P, Filippini A, Cervelli C, et al. Immunosuppressive molecules produced by Sertoli cells cultured in vitro: biological effects on lymphocytes. Biochem Biophys Res Commun. 1992;186(3):1639–1646. doi: 10.1016/s0006-291x(05)81596-7. [DOI] [PubMed] [Google Scholar]
- 40.Selawry HP, Kotb M, Herrod HG, Lu ZN. Production of a factor, or factors, suppressing IL-2 production and T cell proliferation by Sertoli cell-enriched preparations. A potential role for islet transplantation in an immunologically privileged site. Transplantation. 1991;52:846–850. doi: 10.1097/00007890-199111000-00018. [DOI] [PubMed] [Google Scholar]
- 41.Takeda Y, Gotoh M, Dono K, et al. Protection of islet allografts transplanted together with Fas ligand expressing testicular allografts. Diabetologia. 1998;41:315–321. doi: 10.1007/s001250050909. [DOI] [PubMed] [Google Scholar]
- 42.Bladergroen BA, Strik MC, Bovenschen N, et al. The granzyme B inhibitor, protease inhibitor 9, is mainly expressed by dendritic cells and at immune-privileged sites. J Immunol. 2001;166(5):3218–3225. doi: 10.4049/jimmunol.166.5.3218. [DOI] [PubMed] [Google Scholar]
- 43.Cunningham TD, Jiang X, Shapiro DJ. Expression of high levels of human proteinase inhibitor 9 blocks both perforin/granzyme and Fas/Fas ligand-mediated cytotoxicity. Cell Immunol. 2007;245(1):32–41. doi: 10.1016/j.cellimm.2007.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Allison J, Georgiou HM, Strasser A, Vaux DL. Transgenic expression of CD95 ligand on isletβ cells induces a granulocytic infiltration but does not confer immune privilege upon islet allografts. Proc Natl Acad Sci USA. 1999;94(8):3943–3947. doi: 10.1073/pnas.94.8.3943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kang SM, Schneider DB, Lin Z, et al. Fas ligand expression in islets of Langerhans does not confer immune privilege and instead targets them for rapid destruction. Nat Med. 1997;3(7):738–743. doi: 10.1038/nm0797-738. [DOI] [PubMed] [Google Scholar]
- 46.Suarez-Pinzon W, Korbutt GS, Power R, et al. Testicular Sertoli cells protect islet β-cells from autoimmune destruction in NOD mice by a transforming growth factor-β1-dependent mechanism. Diabetes. 2000;49(11):1810–1818. doi: 10.2337/diabetes.49.11.1810. [DOI] [PubMed] [Google Scholar]
- 47.Kang SM, Schneider DB, Lin Z, et al. Fas ligand expression in islets of Langerhans does not confer immune privilege and instead targets them for rapid destruction. Nat Med. 1997;3(7):738–43. doi: 10.1038/nm0797-738. [DOI] [PubMed] [Google Scholar]
- 48.Qian S, Thai NL, Lu L, Fung JJ, Thomson AW. Liver transplant tolerance: mechanistic insights from animal models, with particular reference to the mouse. Transplant Rev. 1997;11:151–164. [Google Scholar]
- 49.Cantor HM, Dumont AE. Hepatic suppression of sensitization to antigen absorbed into the portal system. Nature. 1967;215:744–745. doi: 10.1038/215744a0. [DOI] [PubMed] [Google Scholar]
- 50.Benseler V, McCaughan GW, Schlitt HJ, et al. The liver: a special case in transplantation tolerance. Semin Liver Dis. 2007;27:194–213. doi: 10.1055/s-2007-979471. [DOI] [PubMed] [Google Scholar]
- 51.Orlando G, Soker S, Wood K. Operational tolerance after liver transplantation. J Hepatology. 2009;50:1247–1257. doi: 10.1016/j.jhep.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 52.Knolle PA. Involvement of the liver in the induction of CD8 T cell tolerance towards oral antigen Z. Gastroenterology. 2006;44(1):51–56. doi: 10.1055/s-2005-858988. [DOI] [PubMed] [Google Scholar]
- 53.Yu MC, Chen CH, Liang X, et al. Inhibition of T-cell responses by hepatic stellate cells via B7-H1-mediated T-cell apoptosis in mice. Hepatology. 2004;40(6):1312–1321. doi: 10.1002/hep.20488. [DOI] [PubMed] [Google Scholar]
- 54.Giampieri MP, Jezequel AM, Orlandi F. The lipocytes in normal human liver. A quantitative study. Digestion. 1981;22(4):165–169. doi: 10.1159/000198640. [DOI] [PubMed] [Google Scholar]
- 55.Jezequel AM, Novelli G, Venturini C, Orlandi F. Quantitative analysis of the perisinusoidal cells in human liver; the lipocytes. Front Gastrointest Res. 1984;8:85–90. [Google Scholar]
- 56.Friedman SL. Hepatic stellate cells: protean, multifunctional, and enigmatic cells of the liver. Physiol Rev. 2008;88(1):125–172. doi: 10.1152/physrev.00013.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen CH, Kuo LM, Chang Y, et al. In vivo immune modulatory activity of hepatic stellate cells in mice. Hepatology. 2006;44(5):1171–1181. doi: 10.1002/hep.21379. [DOI] [PubMed] [Google Scholar]
- 58.Qian S, Lu L, Fu F, et al. Apoptosis within spontaneously accepted mouse liver allografts: evidence for deletion of cytotoxic T cells and implications for tolerance induction. J Immunol. 1997;158(10):4654–4661. [PMC free article] [PubMed] [Google Scholar]
- 59.Chen CH, Shu KH, Su YH, et al. Cotransplantation of hepatic stellate cells attenuates the severity of graft-versus-host disease. Transplant Proc. 2010;42(3):971–915. doi: 10.1016/j.transproceed.2010.02.039. [DOI] [PubMed] [Google Scholar]
- 60.Chen CH, Kuo LM, Chang Y, et al. In vivo immune modulatory activity of hepatic stellate cells in mice. Hepatology. 2006;44(5):1171–1181. doi: 10.1002/hep.21379. [DOI] [PubMed] [Google Scholar]
- 61.Jiang G, Yang HR, Wang L, et al. Hepatic stellate cells preferentially expand allogeneic CD4+ CD25+ FoxP3+ regulatory T cells in an IL-2-dependent manner. Transplantation. 2008;86(11):1492–1502. doi: 10.1097/TP.0b013e31818bfd13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Boros P, Ochando JC, Chen SH, Bromberg JS. Myeloid-derived suppressor cells: natural regulators for transplant tolerance. Hum Immunol. 2010;71(11):1061–1066. doi: 10.1016/j.humimm.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Condamine T, Gabrilovich DI. Molecular mechanisms regulating myeloid-derived suppressor cell differentiation and function. Trends Immunol. 2011;32(1):19–25. doi: 10.1016/j.it.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chou HS, Hsieh CC, Yang HR, et al. Hepatic stellate cells regulate immune response by way of induction of myeloid suppressor cells in mice. Hepatology. 2011;53(3):1007–1019. doi: 10.1002/hep.24162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lees JR, Azimzadeh AM, Bromberg JS. Myeloid derived suppressor cells in transplantation. Curr Opin Immunol. 2011;23(5):692–697. doi: 10.1016/j.coi.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 66.Caplan AI. Mesenchymal stem cells. J Orthop Res. 1991;9:641–650. doi: 10.1002/jor.1100090504. [DOI] [PubMed] [Google Scholar]
- 67.Zuk PA, Zhu M, Mizuno H, et al. Multilineage cells from human adipose tissue: Implications for cell-based therapies. Tissue Eng. 2001;7:211–228. doi: 10.1089/107632701300062859. [DOI] [PubMed] [Google Scholar]
- 68.Kern S, Eichler H, Stoeve J, et al. Comparative analysis of mesenchymal stem cells from bone marrow, umbilical cord blood, or adipose tissue. Stem Cells. 2006;24:1294–1301. doi: 10.1634/stemcells.2005-0342. [DOI] [PubMed] [Google Scholar]
- 69.Lee RH, Kim B, Choi I, et al. Characterization and expression analysis of mesenchymal stem cells from human bone marrow and adipose tissue. Cell Physiol Biochem. 2004;14:311–324. doi: 10.1159/000080341. [DOI] [PubMed] [Google Scholar]
- 70.Mitchell JB, McIntosh K, Zvonic S, et al. Immunophenotype of human adipose-derived cells: temporal changes in stromal-associated and stem cell-associated markers. Stem Cells. 2006;24:376–385. doi: 10.1634/stemcells.2005-0234. [DOI] [PubMed] [Google Scholar]
- 71.Romanov YA, Svintsitskaya VA, Smirnov VN. Searching for alternative sources of postnatal human mesenchymal stem cells: candidate MSC like cells from umbilical cord. Stem Cells. 2003;21:105–110. doi: 10.1634/stemcells.21-1-105. [DOI] [PubMed] [Google Scholar]
- 72.Lee OK, Kuo TK, Chen WM, et al. Isolation of multipotent mesenchymal stem cells from umbilical cord blood. Blood. 2004;103:1669–1675. doi: 10.1182/blood-2003-05-1670. [DOI] [PubMed] [Google Scholar]
- 73.In ’t Anker PS, Scherjon SA, Kleijburg-van der Keur C, et al. Isolation of mesenchymal stem cells of fetal or maternal origin from human placenta. Stem Cells. 2004;22:1338–1345. doi: 10.1634/stemcells.2004-0058. [DOI] [PubMed] [Google Scholar]
- 74.Villaron EM, Almeida J, Lopez-Holgado N, et al. Mesenchymal stem cells are present in peripheral blood and can engraft after allogeneic hematopoietic stem cell transplantation. Haematologica. 2004;89:1421–1427. [PubMed] [Google Scholar]
- 75.Roufosse CA, Direkze NC, Otto WR, et al. Circulating mesenchymal stem cells. Int J Biochem Cell Biol. 2004;36:585–597. doi: 10.1016/j.biocel.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 76.In ‘t Anker PS, Noort WA, Scherjon SA, et al. Mesenchymal stem cells in human second-trimester bone marrow, liver, lung, and spleen exhibit a similar immunophenotype but a heterogeneous multilineage differentiation potential. Haematologica. 2003;88(8):845–852. [PubMed] [Google Scholar]
- 77.In’t Anker PS, Scherjon SA, Kleijburgvan der Keur C, et al. Amniotic fluid as a novel source of mesenchymal stem cells for therapeutic transplantation. Blood. 2003;102:1548–1549. doi: 10.1182/blood-2003-04-1291. [DOI] [PubMed] [Google Scholar]
- 78.De Coppi P, Bartsch G, Jr, Siddiqui MM, et al. Isolation of amniotic stem cell lines with potential for therapy. Nat Biotechnol. 2007;25:100–106. doi: 10.1038/nbt1274. [DOI] [PubMed] [Google Scholar]
- 79.Di Nicola M, Carlo-Stella C, Magni M, et al. Human bone marrow stromal cells suppress T lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood. 2002;99:3838–3843. doi: 10.1182/blood.v99.10.3838. [DOI] [PubMed] [Google Scholar]
- 80.Le Blanc K, Tammik L, Sundberg B, Haynesworth SE, Ringden O. Mesenchymal stem cells inhibit and stimulate mixed lymphocyte cultures and mitogenic responses independently of the major histocompatibility complex. Scand J Immunol. 2003;57:11–20. doi: 10.1046/j.1365-3083.2003.01176.x. [DOI] [PubMed] [Google Scholar]
- 81.Potian JA, Aviv H, Ponzio NM, Harrison JS, Rameshwar P. Veto-like activity of mesenchymal stem cells: functional discrimination between cellular responses to alloantigens and recall antigens. J Immunol. 2003;171:3426–3434. doi: 10.4049/jimmunol.171.7.3426. [DOI] [PubMed] [Google Scholar]
- 82.Tse WT, Pendleton JD, Beyer WM, Egalka MC, Guinan EC. Suppression of allogeneic T-cell proliferation by human marrow stromal cells: implications in transplantation. Transplantation. 2003;75:389–397. doi: 10.1097/01.TP.0000045055.63901.A9. [DOI] [PubMed] [Google Scholar]
- 83.Bartholomew A, Sturgeon C, Siatskas M, et al. Mesenchymal stem cells suppress lymphocyte proliferation in vitro and prolong skin graft survival in vivo. Exp Hematol. 2002;30:42–48. doi: 10.1016/s0301-472x(01)00769-x. [DOI] [PubMed] [Google Scholar]
- 84.Djouad F, Plence P, Bony C, et al. Immunosuppressive effect of mesenchymal stem cells favors tumor growth in allogeneic animals. Blood. 2003;102:3837–3844. doi: 10.1182/blood-2003-04-1193. [DOI] [PubMed] [Google Scholar]
- 85.Krampera M, Glennie S, Dyson J, et al. Bone marrow mesenchymal stem cells inhibit the response of naive and memory antigen-specific T cells to their cognate peptide. Blood. 2003;101:3722–3729. doi: 10.1182/blood-2002-07-2104. [DOI] [PubMed] [Google Scholar]
- 86.Maccario R, Podesta M, Moretta A, et al. Interaction of human mesenchymal stem cells with cells involved in alloantigen-specific immune response favors the differentiation of CD4+ T-cell subsets expressing a regulatory/suppressive phenotype. Haematologica. 2005;90:516–525. [PubMed] [Google Scholar]
- 87.Beyth S, Borovsky Z, Mevorach D, et al. Human mesenchymal stem cells alter antigen-presenting cell maturation and induce T-cell unresponsiveness. Blood. 2005;105:2214–2219. doi: 10.1182/blood-2004-07-2921. [DOI] [PubMed] [Google Scholar]
- 88.Aggarwal S, Pittenger MF. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood. 2005;105:1815–1822. doi: 10.1182/blood-2004-04-1559. [DOI] [PubMed] [Google Scholar]
- 89.Zhang W, Ge W, Li C, et al. Effects of mesenchymal stem cells on differentiation, maturation, and function of human monocyte-derived dendritic cells. Stem Cells Dev. 2004;13:263–271. doi: 10.1089/154732804323099190. [DOI] [PubMed] [Google Scholar]
- 90.Jiang XX, Zhang Y, Liu B, et al. Human mesenchymal stem cells inhibit differentiation and function of monocyte-derived dendritic cells. Blood. 2005;105:4120–4126. doi: 10.1182/blood-2004-02-0586. [DOI] [PubMed] [Google Scholar]
- 91.Nauta AJ, Kruisselbrink AB, Lurvink E, et al. Mesenchymal stem cells inhibit generation and function of both CD34+-derived and monocyte derived dendritic cells. J Immunol. 2006;177:2080–2087. doi: 10.4049/jimmunol.177.4.2080. [DOI] [PubMed] [Google Scholar]
- 92.Tse WT, Pendleton JD, Beyer WM, Egalka MC, Guinan EC. Suppression of allogeneic T-cell proliferation by human marrow stromal cells: implications in transplantation. Transplantation. 2003;75:389–397. doi: 10.1097/01.TP.0000045055.63901.A9. [DOI] [PubMed] [Google Scholar]
- 93.Mellor AL, Munn DH. Tryptophan catabolism and T-cell tolerance: immunosuppression by starvation? Immunol Today. 1999;20:469–473. doi: 10.1016/s0167-5699(99)01520-0. [DOI] [PubMed] [Google Scholar]
- 94.Frumento G, Rotondo R, Tonetti M, Damonte G, Benatti U, Ferrara GB. Tryptophan-derived catabolites are responsible for inhibition of T and natural killer cell proliferation induced by indoleamine 2,3-dioxygenase. J Exp Med. 2002;196:459–468. doi: 10.1084/jem.20020121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Liu XQ, Wang X. Indoleamine 2,3-dioxygenase in tumor induced tolerance. Chin Med J (Engl) 2009;122(24):3072–3077. [PubMed] [Google Scholar]
- 96.Meisel R, Zibert A, Laryea M, Göbel U, Däubener W, Dilloo D. Human bone marrow stromal cells inhibit allogeneic T-cell responses by indoleamine 2,3-dioxygenase-mediated tryptophan degradation. Blood. 2004;103(12):4619–4621. doi: 10.1182/blood-2003-11-3909. [DOI] [PubMed] [Google Scholar]
- 97.Moustakas A, Pardali K, Gaal A, Heldin CH. Mechanisms of TGF-β signaling in regulation of cell growth and differentiation. Immunol Lett. 2002;82(1–2):85–91. doi: 10.1016/s0165-2478(02)00023-8. [DOI] [PubMed] [Google Scholar]
- 98.Rasmusson I, Ringdén O, Sundberg B, Le Blanc K. Mesenchymal stem cells inhibit lymphocyte proliferation by mitogens and alloantigens by different mechanisms. Exp Cell Res. 2005;305(1):33–41. doi: 10.1016/j.yexcr.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 99.Ball LM, Bernardo ME, Roelofs H, et al. Cotransplantation of ex vivo expanded mesenchymal stem cells accelerates lymphocyte recovery and may reduce the risk of graft failure in haploidentical hematopoietic stem-cell transplantation. Blood. 2007;110(7):2764–2767. doi: 10.1182/blood-2007-04-087056. [DOI] [PubMed] [Google Scholar]
- 100.Le Blanc K, Rasmusson I, Sundberg B, et al. Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet. 2004;363(9419):1439–1441. doi: 10.1016/S0140-6736(04)16104-7. [DOI] [PubMed] [Google Scholar]
- 101.Augello A, Tasso R, Negrini SM, Cancedda R, Pennesi G. Cell therapy using allogeneic bone marrow mesenchymal stem cells prevents tissue damage in collagen-induced arthritis. Arthritis Rheum. 2007;56(4):1175–1186. doi: 10.1002/art.22511. [DOI] [PubMed] [Google Scholar]
- 102.Parekkadan B, Tilles AW, Yarmush ML. Bone marrow-derived mesenchymal stem cells ameliorate autoimmune enteropathy independently of regulatory T cells. Stem Cells. 2008;26(7):1913–1919. doi: 10.1634/stemcells.2007-0790. [DOI] [PubMed] [Google Scholar]
- 103.Fiorina P, Jurewicz M, Augello A, et al. Immunomodulatory function of bone marrow-derived mesenchymal stem cells in experimental autoimmune Type 1 diabetes. J Immunol. 2009;183(2):993–1004. doi: 10.4049/jimmunol.0900803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ding Y, Xu D, Feng G, Bushell A, Muschel RJ, Wood KJ. Mesenchymal stem cells prevent the rejection of fully allogenic islet grafts by the immunosuppressive activity of matrix metalloproteinase-2 and -9. Diabetes. 2009;58(8):1797–1806. doi: 10.2337/db09-0317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Li FR, Wang XG, Deng CY, Qi H, Ren LL, Zhou HX. Immune modulation of co-transplantation mesenchymal stem cells with islet on T and dendritic cells. Clin Exp Immunol. 2010;161(2):357–363. doi: 10.1111/j.1365-2249.2010.04178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bartholomew A, Sturgeon C, Siatskas M, et al. Mesenchymal stem cells suppress lymphocyte proliferation in vitro and prolong skin graft survival in vivo. Exp Hematol. 2002;30(1):42–48. doi: 10.1016/s0301-472x(01)00769-x. [DOI] [PubMed] [Google Scholar]
- 107.Casiraghi F, Azzollini N, Cassis P, et al. Pretransplant infusion of mesenchymal stem cells prolongs the survival of a semiallogeneic heart transplant through the generation of regulatory T cells. J Immunol. 2008;181(6):3933–3946. doi: 10.4049/jimmunol.181.6.3933. [DOI] [PubMed] [Google Scholar]
- 108.Ringdén O, Uzunel M, Rasmusson, et al. Mesenchymal stem cells for treatment of therapy-resistant graft-versus-host disease. Transplantation. 2006;81(10):1390–1397. doi: 10.1097/01.tp.0000214462.63943.14. [DOI] [PubMed] [Google Scholar]
- 109.Le Blanc K, Frassoni F, Ball L, et al. Mesenchymal stem cells for treatment of steroid-resistant, severe, acute graft-versus-host disease: a Phase II study. Lancet. 2008;371(9624):1579–1586. doi: 10.1016/S0140-6736(08)60690-X. [DOI] [PubMed] [Google Scholar]
- 110.Ringden O, Le Blanc K. Mesenchymal stem cells for treatment of acute and chronic graft-versus-host disease, tissue toxicity and hemorrhages. Best Pract Res Clin Haematol. 2011;24(1):65–72. doi: 10.1016/j.beha.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 111.Fang B, Song Y, Liao L, Zhang Y, Zhao RC. Favorable response to human adipose tissue-derived mesenchymal stem cells in steroid-refractory acute graft-versus-host disease. Transplant Proc. 2007;39(10):3358–3362. doi: 10.1016/j.transproceed.2007.08.103. [DOI] [PubMed] [Google Scholar]
- 112.Ho S-J, Dyson P, Rawling T, et al. Mesenchymal stem cells for treatment of steroid resistant graft-versus-host disease. Biol Blood Marrow Transplant. 2009;13:46–47. [Google Scholar]
- 113.Kebriaei P, Isola L, Bahceci E, et al. Adult human mesenchymal stem cells added to corticosteroid therapy for the treatment of acute graft-versus-host disease. Biol Blood Marrow Transplant. 2009;15(7):804–811. doi: 10.1016/j.bbmt.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 114.Von Bonin M, Stölzel F, Goedecke A, et al. Treatment of refractory acute GVHD with third-party MSC expanded in platelet lysate-containing medium. Bone Marrow Transplant. 2009;43(3):245–251. doi: 10.1038/bmt.2008.316. [DOI] [PubMed] [Google Scholar]
- 115.Lucchini G, Introna M, Dander E, et al. Platelet-lysate-expanded mesenchymal stromal cells as a salvage therapy for severe resistant graft-versus-host disease in a pediatric population. Biol Blood Marrow Transplant. 2010;16(9):1293–1301. doi: 10.1016/j.bbmt.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 116.Prasad VK, Lucas KG, Kleiner GI, et al. Efficacy and safety of ex vivo cultured adult human mesenchymal stem cells (Prochymal™) in pediatric patients with severe refractory acute graft-versus-host disease in a compassionate use study. Biol Blood Marrow Transplant. 2011;17(4):534–541. doi: 10.1016/j.bbmt.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 117.Ning H, Yang F, Jiang M, et al. The correlation between cotransplantation of mesenchymal stem cells and higher recurrence rate in hematologic malignancy patients: outcome of a pilot clinical study. Leukemia. 2008;22(3):593–599. doi: 10.1038/sj.leu.2405090. [DOI] [PubMed] [Google Scholar]
- 118.Dahlke MH, Hoogduijn M, Eggenhofer E, et al. Toward MSC in solid organ transplantation: 2008 position paper of the MISOT study group. Transplantation. 2009;88(5):614–619. doi: 10.1097/TP.0b013e3181b4425a. [DOI] [PubMed] [Google Scholar]
- 119.Hoogduijn MJ, Popp FC, Grohnert A, et al. Advancement of mesenchymal stem cell therapy in solid organ transplantation(MISOT) Transplantation. 2010;90(2):124–126. doi: 10.1097/TP.0b013e3181ea4240. [DOI] [PubMed] [Google Scholar]
- 120.Sbano P, Cuccia A, Mazzanti B, et al. Use of donor bone marrow mesenchymal stem cells for treatment of skin allograft rejection in a preclinical rat model. Arch Dermatol Res. 2008;300(3):115–124. doi: 10.1007/s00403-007-0827-9. [DOI] [PubMed] [Google Scholar]
- 121.Magatti M, De Munari S, Vertua E, et al. Human amnion mesenchyme harbors cells with allogeneic T-cell suppression and stimulation capabilities. Stem Cells. 2008;26(1):182–192. doi: 10.1634/stemcells.2007-0491. [DOI] [PubMed] [Google Scholar]
- 122.Banas RA, Trumpower C, Bentlejewski C, et al. Immunogenicity and immunomodulatory effects of amnion-derived multipotent progenitor cells. Hum Immunol. 2008;69(6):321–328. doi: 10.1016/j.humimm.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 123.Chang CJ, Yen ML, Chen YC, et al. Placenta-derived multipotent cells exhibit immunosuppressive properties that are enhanced in the presence of interferon-gamma. Stem Cells. 2006;24(11):2466–2477. doi: 10.1634/stemcells.2006-0071. [DOI] [PubMed] [Google Scholar]
- 124.Beyth S, Borovsky Z, Mevorach D, et al. Human mesenchymal stem cells alter antigen-presenting cell maturation and induce T-cell unresponsiveness. Blood. 2005;105(5):2214–2219. doi: 10.1182/blood-2004-07-2921. [DOI] [PubMed] [Google Scholar]
- 125.Zhang W, Ge W, Li C, et al. Effects of mesenchymal stem cells on differentiation, maturation, and function of human monocyte-derived dendritic cells. Stem Cells Dev. 2004;13(3):263–271. doi: 10.1089/154732804323099190. [DOI] [PubMed] [Google Scholar]
- 126.Nauta AJ, Fibbe WE. Immunomodulatory properties of mesenchymal stromal cells. Blood. 2007;110(10):3499–3506. doi: 10.1182/blood-2007-02-069716. [DOI] [PubMed] [Google Scholar]
- 127.Jiang XX, Zhang Y, Liu B, et al. Human mesenchymal stem cells inhibit differentiation and function of monocyte-derived dendritic cells. Blood. 2005;105(10):4120–4126. doi: 10.1182/blood-2004-02-0586. [DOI] [PubMed] [Google Scholar]
- 128.Magatti M, De Munari S, Vertua E, et al. Amniotic mesenchymal tissue cells inhibit dendritic cell differentiation of peripheral blood and amnion resident monocytes. Cell Transplant. 2009;18(8):899–914. doi: 10.3727/096368909X471314. [DOI] [PubMed] [Google Scholar]
- 129.Parolini O, Caruso M. Review: preclinical studies on placenta-derived cells and amniotic membrane: an update. Placenta. 2011;32(Suppl 2):S186–S195. doi: 10.1016/j.placenta.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 130.Gores PF, Hayes DH, Copeland MJ, et al. Long-term survival of intratesticular porcine islets in nonimmunosuppressed beagles. Transplantation. 2003;75(5):613–618. doi: 10.1097/01.TP.0000052376.89400.8D. [DOI] [PubMed] [Google Scholar]