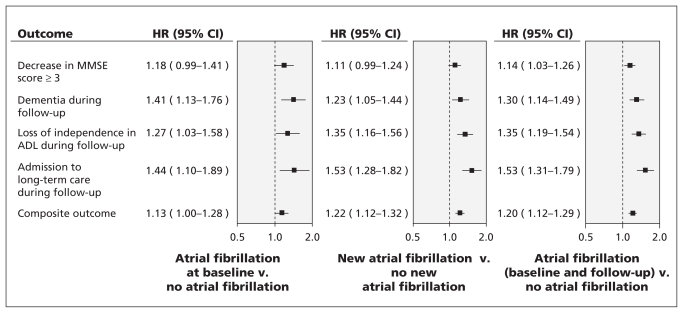
Figure 1:
Multivariable association between atrial fibrillation (at baseline and during follow-up) and cognitive and functional outcomes. Models were adjusted for the following confounding variables: age; level of education; sex; baseline MMSE score; systolic blood pressure at baseline; history of stroke or transient ischemic attack, hypertension, diabetes and myocardial infarction; levels of microalbuminuria, macroalbuminuria and creatinine; treatment with statins, β-blockers, angiotensin-converting enzyme inhibitors, antiplatelet therapy or oral anticoagulants; changes in systolic blood pressure during follow-up; smoking; body mass index; level of physical activity; presence of sleep apnea; and alcohol consumption. Hazard ratios greater than 1.00 suggest increased risk of the specified outcome. The composite outcome was a decrease in MMSE score of 3 points or more, new diagnosis of dementia at follow-up, loss of independence with performing ADL and admission to a long-term care facilty. ADL = activities of daily living, CI = confidence interval, HR = hazard ratio, MMSE = Mini–Mental State Examination.