To the Editor:
Ehlers-Danlos syndrome (EDS) type VIII (OMIM # 130080) is a distinct, largely unrecognized form of EDS characterized primarily by generalized periodontal disease causing progressive loss of the alveolar bone and subsequent dental loss. The associated clinical abnormalities include joint and skin manifestations and with much clinical overlap to other EDS subtypes, mainly the hypermobility and classic types [Stewart et al., 1977; Reinstein et al., 2011; Castori et al., 2010]. A few reported patients had facial characteristics like EDS type IV. The diagnosis of EDS type VIII is established in an individual presenting with dental and connective tissue findings and a typical pattern of inheritance. Previous studies suggest that EDS type VIII is due to dominantly transmitted heterozygous mutations in a yet to be identified gene that is most likely expressed in the periodontal ligament – the tooth supporting matrix – in addition to other connective tissues. Periodontal disease in EDS type VIII seems to be highly penetrant, and can affect young children, which rarely have periodontal disease, even in the presence of poor oral hygiene. Limited data are available on the spectrum of clinical manifestations and natural history of the disorder, resulting in part from the fact that periodontitis and joint hypermobility syndromes are common in the general population [Papapanou, 1999; Khalili, 2008; Biro et al., 1983; Seçkin et al., 2005]. Thus, it is likely that individuals with milder clinical manifestations do not come to medical attention and thus go undetected.
Musculoskeletal involvement is a frequent finding in hereditary disorders of connective tissue (HDCT). The range of skeletal abnormalities is broad and involves rather benign pectus deformity and pes planus to a more severe expression including progressive scoliosis, contractures, craniosynostosis, recurrent large joint dislocations, and chronic joint instability leading to an early onset degenerative joint disease.
There is significant phenotypic variability in EDS type VIII, especially in regard to the skeletal phenotype. Several skeletal phenotypes are known in EDS type VIII, including large and small joint laxity (minimal or significant) and dislocations, Marfanoid habitus, arachnodactyly, chronic joint and limb pain, pectus excavatum, scoliosis, and pes planus [Karrer et al., 2000; Reinstein et al., 2011].
We aimed to explore the skeletal manifestations and complications in a proposita of a previously unreported three generation kindred with EDS type VIII. The patient is a 37-year-old woman who was referred for evaluation of connective tissue disorder. She always had problems with her teeth. Her deciduous teeth appeared at age 1 but soon after turned black and rotten, and all had to be removed before age 18 months. Her permanent teeth appeared at age 7. During her teenage years and in her 20's she underwent numerous dental treatments and extractions, eventually loosing most of her permanent teeth, except for her incisors, in her late 20's. Dental exam and imaging revealed multiple missing teeth and gingival inflammation was severe throughout the mouth. There was moderate periodontitis (class III; with IV being the most severe according to the American Dental Association classification) and radiographic widening of the periodontal ligament space on tooth 27 which was mobile. During the past year, the patient lost the residual incisors and currently wears dentures. She was told that the reason for her dental loss is “soft bone“. The patient reported being very flexible and double jointed from childhood but did not dislocate any joints. During adolescence she developed scoliosis diagnosed through routine exam in high school. She first experienced lower back, hip and knee joint pain in her early 20's; these symptoms have become chronic. At that time, rheumatology workup excluded autoimmune disorders and inflammatory arthritis and she was given pain medications without a specific diagnosis. At age 36 she was first seen by an orthopedist because of increasing left hip pain and imaging studies of the pelvis showed left proximal femur enchondroma which was excised. Since her generalized joint pain had not resolved following surgery, she was further referred for genetic evaluation. Other relevant medical history includes easy bruising with normal healing and normal scar formation. She has myopia and strabismus; a recent echocardiogram was unremarkable. The patient is now experiencing chronic pain in her back, knees, hips and most of her finger joints and is treated with high dose of opiate analgesics. She has a normal body habitus, and soft, doughy but not hyperextensible skin, mild joint laxity was noted although full evaluation for Beighton score was limited because of joint pain triggered by motion. Facial characteristics showed long and narrow nasal bridge with prominent tip; features that have been described before in patients with this type of EDS (Fig.1). Her mother and maternal grandmother have the same medical condition. Her mother, age 58, reports a very similar history with joint laxity for most of her life and dental problems. Currently joint laxity is less pronounced [Beighton score 3], and she is experiencing intermittent back and joint pains. She has osteoporosis diagnosed by bone density scan in her early 40's. She lost all her teeth by age 35 and has worn dentures since than. Facial features are similar to her daughter. The patient's maternal grandmother, currently 82, lost all her teeth by age 20. She has generalized joint pain but has not been under clinical supervision due to lack of insurance. Following establishment of clinical diagnosis of EDS type VIII in this family, radiological evaluation prompted by the proposita's complaints was completed.
Figure 1.
Facial and dental appearance of family with EDS type VIII.
A, B, and D – proposita; C – her mother. Note long nose with narrow root and prominent tip that have been reported in patients with this type of EDS. Patients wear dentures.
Skeletal survey at the age of 37 years demonstrated multiple abnormal findings in the axial and appendicular skeleton as detailed below. There was moderate scoliosis and radiographically decreased bone density; the latter was confirmed by a dual-emission X-ray absorptiometry (DEXA) study yielding a T score of −2.2 (Fig.2). The sacroiliac joints and hip joints demonstrated no obvious degeneration on conventional radiography. Furthermore, at the right hip, ossicular findings suggested tendinopathy of the gluteal musculature, and at the left hip, there were postsurgical changes of the femoral neck following osteosynthetic treatment of enchondroma (Fig.3). At the right shoulder there was acromio-clavicular joint degeneration, with osteophytic changes and abnormal joint space, also suggesting ligamentous disease. No abnormalities were identified at the left shoulder, the elbow and wrist joints. Radiography and subsequent MR imaging demonstrated distinct osteoarthritis of the right knee joint. Notably, there was marked thinning and damage of the retro-patellar cartilage, as well as in the medial and lateral knee compartments, associated with multiple subchondral cysts and osteophytic changes. At the left knee joint, mild thinning of the cartilaginous surfaces was observed but without further osseous degenerative changes. Joint effusion was present on both sides (Figs.4–5). There were no traumatic or degenerative changes of the collateral and cruciate ligaments of the patellar or quadriceps tendons. Based on an orthopedist evaluation, a joint replacement procedure was suggested to treat right knee joint degeneration.
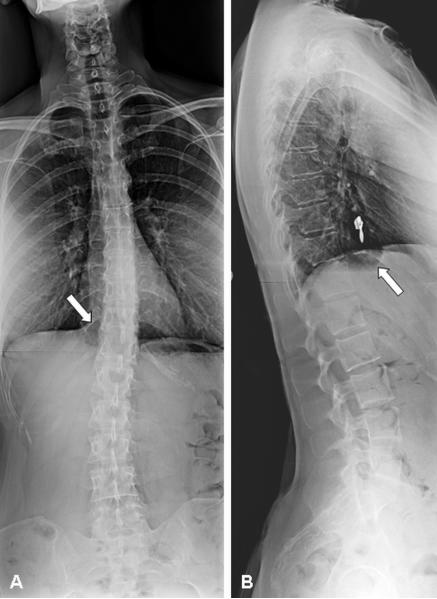
Figure 2.
Anterior-posterior and lateral spine radiographs.
Note moderate S-shaped scoliosis of the spine with maximum point at the thoracic-lumbar junction [A] and decreased bone density as observed on conventional radiography with apparent increased density of the vertebral endplates [B]. In addition, an abnormal pre/paravertebral air-fluid-level collection [arrows] is demonstrated on both planes indicative of a gastro-esophageal hernia [A, B].
Figure 3.
Pelvic radiographs. Anterior-posterior radiograph of the pelvis.
Note normal joint spaces of the hip joints on both sides without obvious degeneration. On the right side, adjacent to the greater trochanter there is an abnormal ossicle [arrow] suggesting tendinopathy of the gluteal muscles. The left femur demonstrates postsurgical changes with osteosynthetic treatment of the femoral neck.
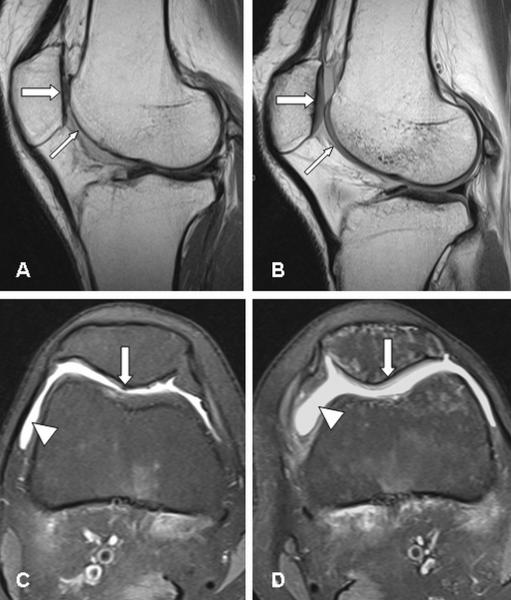
Figure 4.
MR imaging of the knee joints.
Sagittal [A, B] and transverse [C, D] images of the right [A, C] and left [B, D] knee joint, respectively. On the right side, absence of the articular cartilage [thin arrow] of the femoral joint surface [A] and marked defects and thinning of the retro-patellar cartilage [thick arrow]; whereas the cartilaginous layers [arrows] of the left knee are only mildly thinned [B]. The transverse images feature joint effusion on both sides [arrowheads] [C, D], and again distinct cartilage damage of the right retro-patellar surface [arrow] [C], and slight cartilaginous changes left-sided [arrow] [D].
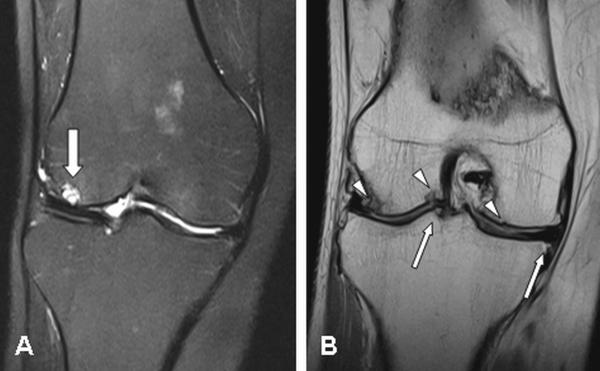
Figure 5.
Coronal MR imaging of the right knee joint.
The lateral joint compartment demonstrates a distinct cyst [arrow] of the subchondral bone [A], and multiple surface and subchondral irregularities [arrowheads], as well as osteophytic spurs [arrows] [B], which are overall the result of marked degeneration.
We show here the radiological manifestations of early-onset osteoarthritis and reduced bone density that can be associated with EDS type VIII. Although prevalent in middle-age and older adults [affecting 10% of individuals over the age of 50 years and up to 70% of the population over the age of 65 years], osteoarthritis is not a common finding in younger individuals unless resulting from mechanical loading/overuse [Karachalios et al., 2004]. The natural history and skeletal complications associated with EDS VIII are understudied, mainly because of the complexity in patient diagnosis; recruitment and long term follow up. While chronic joint pain and scoliosis have been reported in a recent study of an EDS type VIII family, those manifestations have not been documented radiologically but were rather based on patients description [Reinstein et al., 2011]. Although considerable childhood joint hypermobility was reported by the family reported here, progressive joint stiffness made it less noticeable at the time of examination. These observations highlight the importance of screening for early skeletal manifestations in patients with EDS type VIII, as the symptoms and the radiological abnormalities can present years before the patient comes to medical attention and a correct diagnosis is made. A suggested clinical follow-up would consist of spinal surveillance for scoliosis, imaging studies for joint pain, and DEXA bone density scan followed by proper treatment when indicated.
In conclusion, this report supports and extends previous research showing that EDS type VIII can be associated with early-onset degenerative joint disease and reduced bone density, as observed in some other EDS forms. Thus, it implies that clinical surveillance for those complications is warranted. Further detailed clinical studies in larger cohorts of EDS type VIII patients are needed to better delineate the skeletal phenotypic spectrum, and allow optimized clinical follow-up.
ACKNOWLEDGMENT
Dr. Rimoin appreciates support from the Steven Spielberg Pediatric Research Center, the NIH/NICHD Program Project Grant (HD36657), the Medical Genetics NIH/NIGMS Training Program Grant (5-T32-GM08243), and the Cedars-Sinai General Clinical Research Center Grant (M01-RR00425).
Supported by an NICHD Program Project Grant (2P01HD022657) and an NIGMS Postdoctoral Research Training grant (2T32GM008243)
Footnotes
None of the authors of the manuscript has declared any conflict of interest.
REFERENCES
- Biro F, Gewanter HL, Baum J. The hypermobility syndrome. Pediatrics. 1983;72:701–706. [PubMed] [Google Scholar]
- Castori M, Camerota F, Celletti C, Danese C, Santilli V, Saraceni VM, Grammatico P. Natural history and manifestations of the hypermobility type Ehlers–Danlos syndrome: A pilot study on 21 patients. Am J Med Genet. 2010;152:556–564. doi: 10.1002/ajmg.a.33231. [DOI] [PubMed] [Google Scholar]
- Karachalios T, Zibis A, Papanagiotou P, Karantanas AH, Malizos KN, Roidis N. MR imaging findings in early osteoarthritis of the knee. Eur J Radiol. 2004;50:225–230. doi: 10.1016/j.ejrad.2004.01.018. [DOI] [PubMed] [Google Scholar]
- Karrer S, Landthaler M, Schmalz G. Ehlers–Danlos type VIII. Review of the literature. Clin Oral Investig. 2000;4:66–69. doi: 10.1007/s007840050117. [DOI] [PubMed] [Google Scholar]
- Moore MM, Votava JM, Orlow SJ, Schaffer JV. Ehlers–Danlos syndrome type VIII: Periodontitis, easy bruising, marfanoid habitus, and distinctive facies. J Am Acad Dermatol. 2006;55:S41–S45. doi: 10.1016/j.jaad.2006.02.024. [DOI] [PubMed] [Google Scholar]
- Papapanou PN. Epidemiology of periodontal diseases: An update. J Int Acad Periodontol. 1999;1:110–116. [PubMed] [Google Scholar]
- Reinstein E, Wang RY, Zhan L, Rimoin DL, Wilcox WR. Ehlers-Danlos type VIII, periodontitis-type: further delineation of the syndrome in a four-generation pedigree. Am J Med Genet A. 2011;155:742–747. doi: 10.1002/ajmg.a.33914. [DOI] [PubMed] [Google Scholar]
- Seçkin U, Tur BS, Yilmaz O, Yağci I, Bodur H, Arasil T. The prevalence of joint hypermobility among high school students. Rheumatol Int. 2005;25:260–263. doi: 10.1007/s00296-003-0434-9. [DOI] [PubMed] [Google Scholar]
- Stewart RE, Hollister DW, Rimoin DL. A new variant of Ehlers–Danlos syndrome: An autosomal dominant disorder of fragile skin, abnormal scarring, and generalized periodontitis. Birth Defects. 1977;13:85–93. [PubMed] [Google Scholar]