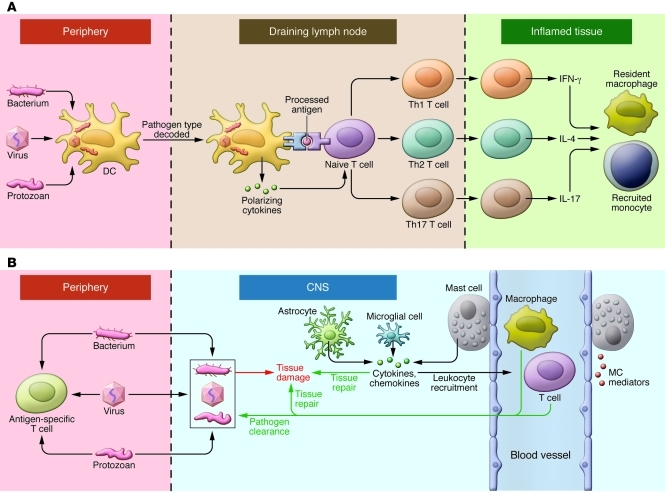
Figure 1. Innate immunity in the periphery and CNS.
(A) In the face of a peripheral infection, innate immune cells prime and instruct T lymphocytes. Tissue DCs internalize microbial protein antigens, process them into peptides, and display them on their surfaces with MHC class II molecules; migrate to draining lymph nodes; and present antigens to naive CD4+ T cells. DCs direct the quality of the subsequent inflammatory response by decoding distinctive pathogen-associated signals and transmitting this information to T cells in the form of regulatory cytokines such as IL-12 (for Th1), IL-4 (Th2), or IL-6/TGF-β (Th17). In addition, lymph node environmental cues can provide information about the site of infection (gut, skin, or other). Armed with this information, effector T cells migrate to infected tissues. Upon reactivation, Th1, Th2, and Th17 cells express phenotype-defining cytokines that act on resident and recruited innate cells, which operate collectively with factors such as complement to clear the infection. (B) Resident microglia and astrocytes exert multiple functions in the CNS, including protective and restorative responses to CNS infection or injury. Cytokines and chemokines expressed by resident CNS cells also promote the recruitment of circulating lymphocytes and myeloid cells from the periphery to assist in pathogen clearance. Innate responses in the CNS cannot directly initiate adaptive immunity. Innate CNS reactions also occur during neuroinflammatory disorders and utilize many of the same components as do host defense responses.