Abstract
Acute fibrinous and organising pneumonia (AFOP) was recently described as an unusual pattern of diffuse lung disease. Particular characteristics make the differential diagnosis with the well recognised clinical patterns of diffuse alveolar damage, cryptogenic organising pneumonia or eosinophilic pneumonia. The lack of hyaline membranes, the presence of intra-alveolar fibrin, absence of noticeable eosinophils and patchy distribution suggests that AFOP define a distinct histological pattern. The authors describe the case of a woman diagnosed with AFOP after surgical lung biopsy, in association with primary biliary cirrhosis. The patient presented dyspnoea, fatigue, dry cough and thoracic pain. The CT scan showed bilateral patchy infiltrates predominantly in the lower lobes. Flexible bronchoscopy and subsidiary techniques were inconclusive and biopsy through video-assisted thoracoscopic surgery led to anatomopathological diagnosis of AFOP. The patient is having a good clinical response to prednisone.
Background
There are only a few clinical cases reported and it is important to discuss the consistency of this new histological pattern and understand its clinical picture.
With this case we pretend to better characterize this entity and lend support to the validity of this independent histological pattern.
Case presentation
A 55-year-old Caucasian woman presented with 1-month history of dyspnoea, fatigue and abnormal lung findings in chest x-ray (figure 1). A few weeks later she began with a dry cough, thoracic pain and had one episode of low-volume haemoptysis. Treatment with antibiotic was completed, without radiological improvement.
Figure 1.
Initial chest x-ray: right side opacity with alveolar characteristics.
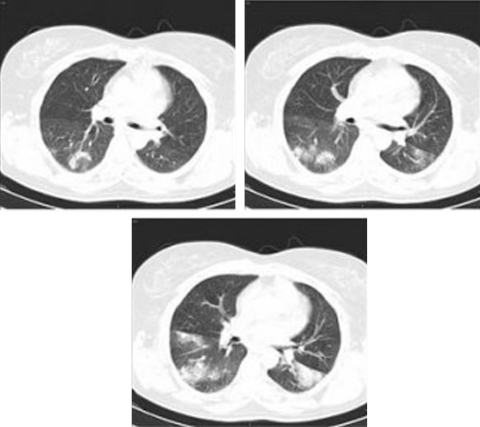
The CT scan showed multiple bilateral opacities with preferential peribronchial distribution and alveolar characteristics. There were also areas of ground glass opacities (figure 2).
Figure 2.
CT scan: bilateral lung consolidations and ground glass opacities.
She was a healthcare assistant, non-smoker and medicated for hypothyroidism and dyslipidaemia. No relevant clinical family history was identified.
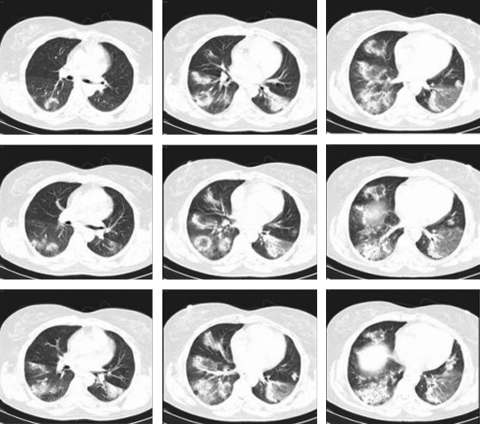
During investigation, there was radiological worsening with enlargement and spread of lung opacifications (figure 3) and rapid clinical deterioration.
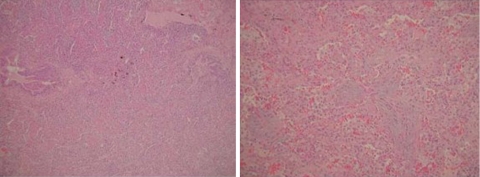
Figure 3.
Histology: lymphoplasmocitary inflammatory infiltrate, fibroblast proliferation and fibrin balls.
Pulmonary auscultation revealed crepitations in bilateral lower zones, otherwise the physical examination was normal.
Laboratory studies showed normal including white cell count, kidney function and urinalyses; sedimentation rate (85 mm/1ah), C reactive protein (7.8 mg/dl), alkaline phosphatase (136 U/l) and c-glutamyl transferase (121 U/l) were elevated.
Investigations
Initial investigation was not diagnostic and further studies were done to confirm or exclude possible infectious, inflammatory and neoplastic causes.
Lung function tests with spirometry and lung volumes revealed normal and a slight decrease (63% of predicted value) in carbon monoxide diffusing capacity. Arterial blood gases were normal.
Tumour markers (NSE, CYFRA 21.1, CEA, CA 125, CA 15.3, CA 19.9 e β2), SACE and autoantibodies (ANA, ENA, ANCA) were within normal range except for AMA 640 U/ml (>20) and anti-M2 67.5 U/ml (>7.0).
Flexible bronchoscopy followed by bronchoalveolar lavage (BAL) and transbronchial biopsy (TBB) was performed and revealed no endobronchial lesion. BAL specimen did not show any micro-organisms or malignant cells. The BAL differential cell count contained high levels of lymphocytes 62% (CD4/CD8 1.3), macrophages 20%, eosinophils 12% and neutrophils 5%. TBB histology revealed a ‘BOOP-like’ pattern.
As a definitive diagnosis was not reached, video-assisted thoracoscopic surgery was performed and lead to the pathological diagnosis of acute fibrinous and organising pneumonia (AFOP) with lymphoplasmocitary inflammatory infiltrate (no eosinophils) and fibroblast proliferation associated with type II pneumocytes hyperplasia. Oedema was presented in some alveolar spaces whereas others had numerous macrophages and fibrin balls. No evidence of hyaline membranes was observed (figure 3).
Hepatic biopsy showed no abnormalities.
Treatment
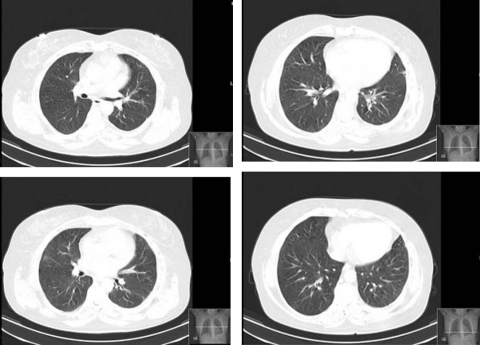
The treatment consisted of prednisone (1 mg/kg/day) with clinical, functional and radiological improvement (figures 4 and 5). There were no side effects related to prednisone. At this time, nearly 14 months after beginning treatment, the patient is asymptomatic but still under treatment (tapering doses of prednisone).
Figure 4.
Chest x-ray after 2 months of treatment.
Figure 5.
CT scan after 4 months of treatment.
As we assumed, the diagnosis of primary biliary cirrhosis because of the presence of AMA, an antibody highly specific, high levels of alkaline phosphatise and clinical association with hyperlipidaemia and hypothyroidism and ursodeoxycholic acid (13 mg/kg/day) was started.
Outcome and follow-up
A positive clinical course was observed. The patient remains asymptomatic, 14 months after histological diagnosis, and resolution of CT images was achieved (figure 5). She is observed regularly in the Pulmonology outpatient clinic.
Discussion
AFOP is an extremely rare pathologic entity that was initially described by Beasley et al1 in 2002, in a review of 17 patients, as a new histological pattern of lung injury. Hwang et al,2 in 2003, reported autopsy data from the lungs of 20 patients who died with severe acute respiratory syndrome and AFOP was identified as the cause in six cases. In more recent published studies, Prahalad et al,3 Damas et al,4 Kobayashi et al5 and Tzouvelekis et al6 describe one case report of AFOP each. The first describe an acute presentation in the context of an inflammatory myopathy, and the others as a subacute presentation in an idiopathic form.
Two different clinical courses have been observed in AFOP7 8: a fulminant presentation often overlapping with acute respiratory distress syndrome and a more subacute form, with favourable treatment response and disease progression.
It has been reported that AFOP8 may occur in an idiopathic context or in association with a wide spectrum of clinical conditions, including autoimmune disease, more often collagen vascular diseases (inflammatory myopathy, juvenile dermatomyositis), adverse drug reactions (amiodarone), occupational or environmental exposures (construction work, coal mining, zoological work), as well as infections (Haemophilus influenzae, Acinetobacter lymphomaairspray). In this case, despite the percutaneous needle biopsies of the liver showed no abnormalities, the presence of AMA and biochemical evidence of cholestasis based on alkaline phosphatase elevation established the diagnosis of primary biliary cirrhosis. Hyperlipidaemia and hypothyroidism provided corroborative data. Therefore, it was made the diagnosis of AFOP in association with primary biliary cirrhosis. Although there is no clinical report describing this association, AFOP is a new entity that has only a few clinical cases reported, and autoimmune disease is an important and previously described association.
Learning points.
-
▶
AFOP is characterised by prominent intra-alveolar fibrin deposition (fibrin balls) resulting in a morphological pattern that may represent an underreported variant of diffuse alveolar damage, cryptogenic organising pneumonia or eosinophilic pneumonia.
-
▶
Dyspnoea and dry cough are the most common presenting symptoms.
-
▶
Two different outcomes have been observed: an acute form in which the patient rapidly progress to death; and a subacute form where the patient evolutes under treatment to recovery.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Beasley MB, Franks TJ, Galvin JR, et al. Acute fibrinous and organizing pneumonia: a histological pattern of lung injury and possible variant of diffuse alveolar damage. Arch Pathol Lab Med 2002;126:1064–70 [DOI] [PubMed] [Google Scholar]
- 2.Hwang DM, Chamberlain DW, Poutanen SM, et al. Pulmonary pathology of severe acute respiratory syndrome in Toronto. Mod Pathol 2005;18:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prahalad S, Bohnsack JF, Maloney CG, et al. Fatal acute fibrinous and organizing pneumonia in a child with juvenile dermatomyositis. J Pediatr 2005;146:289–92 [DOI] [PubMed] [Google Scholar]
- 4.Damas C, Morais A, Moura CS, et al. Acute fibrinous and organizing pneumonia. Rev Port Pneumol 2006;12:615–20 [PubMed] [Google Scholar]
- 5.Kobayashi H, Sugimoto C, Kanoh S, et al. Acute fibrinous organizing pneumonia: initial presentation as a solitary nodule. J Thorac Imaging 2005;20:291–3 [DOI] [PubMed] [Google Scholar]
- 6.Tzouvelekis A, Koutsopoulos A, Oikonomou A, et al. Acute fibrinous and organising pneumonia: a case report and review of the literature. J Med Case Reports 2009;3:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryu JH, Myers JL, Swensen SJ. Bronchiolar disorders. Am J Respir Crit Care Med 2003;168:1277–92 [DOI] [PubMed] [Google Scholar]
- 8.Cordier JF. Organising pneumonia. Thorax 2000;55:318–28 [DOI] [PMC free article] [PubMed] [Google Scholar]