Figure 3.
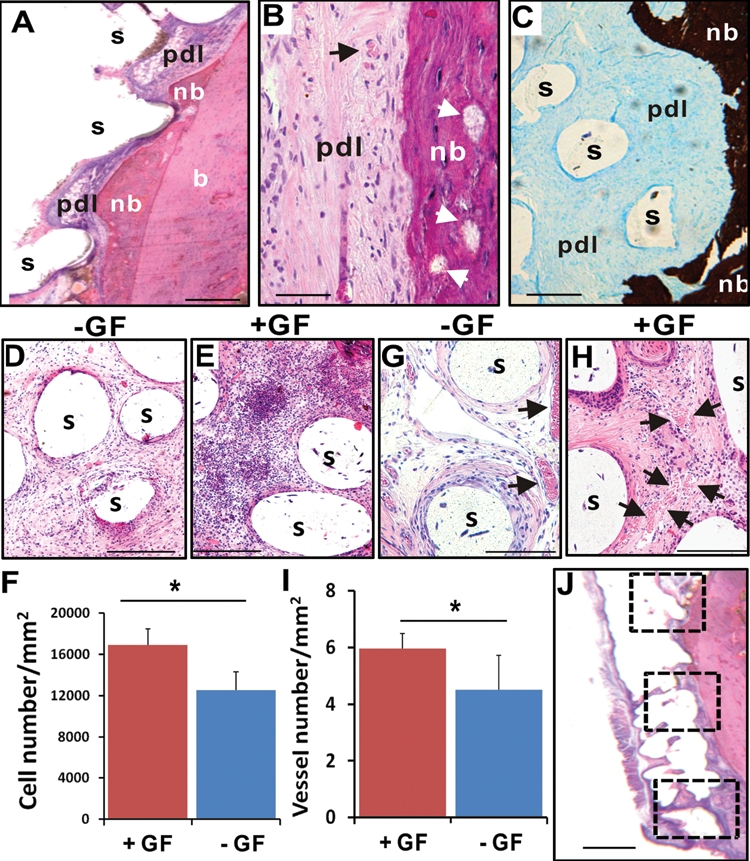
Orthotopic tooth regeneration. (A) The rat mandibular incisor scaffold integrated with surrounding tissue, showing tissue ingrowth into scaffold microchannels and multiple tissue phenotypes, including the native alveolar bone (b), newly formed bone (nb), and a fibrous tissue interface reminiscent of the periodontal ligament (pdl). The newly formed bone (nb) showed ingrowth into microchannel openings and inter-staggered with scaffold microstrands (s). (B) Newly formed bone (nb) has bone trabeculae-like structures (arrows) and embedded osteocyte-like cells, immediately adjacent to a putative periodontal ligament (pdl) consisting of fibroblast-like cells and collagen buddle-like structures. (C) Newly formed bone (nb) is well-mineralized (von Kossa preparation), in contrast to the adjacent unmineralized, putative periodontal ligament (pdl). (D) Cells populated the scaffold’s microchannels even without growth-factor delivery. Remarkably, SDF1 and BMP7 delivery yielded substantial cell homing in microchannels (E). (F) Combined SDF1 and BMP7 delivery homed significantly more cells into microchannels than without growth-factor delivery (p < 0.01; N = 11). Angiogenesis took place in scaffolds’ microchannels without growth-factor delivery (G), but was more substantial with growth-factor delivery (H). (I) Combined SDF1 and BMP7 delivery elaborated significantly more blood vessels than without growth-factor delivery (p < 0.05; N = 11). (J) The numbers of recruited cells and blood vessels were quantified from 3 different locations along the entire root length of the rat mandibular incisor scaffold: the superior region of alveolar ridge and the inferior region of root apex, with a midpoint in between. s, scaffold; GF, growth factor(s). Scale: 100 µm.
