LETTER
Escherichia coli isolates harboring CTX-M β-lactamases have rarely been obtained from children in the United States. Here we report eight such isolates from seven community-dwelling pediatric patients and their microbiological and clinical correlates. Pediatric E. coli isolates identified as extended-spectrum β-lactamase (ESBL) positive by the New York Hospital Queens Clinical Microbiology Laboratory (February to June 2009) using BD Phoenix NMIC/ID-123 panels (Becton Dickinson and Company, Sparks, MD) were PCR screened for blaCTX-M, E. coli phylogenic group (A, B1, B2, or D), sequence type ST131 clonal group membership, and 51 extraintestinal pathogenic E. coli (ExPEC) virulence genes (5, 7) and underwent XbaI pulsed-field gel electrophoresis (PFGE) analysis (5, 11). MICs were determined by Etest (bioMérieux, North America). Relevant demographic and clinical data were obtained via medical record review and patient and provider interviews.
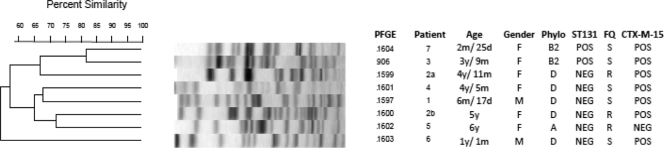
Six patients contributed 1 isolate each; another patient contributed 2 isolates (2a and 2b) with dissimilar PFGE profiles from separate infection episodes. All isolates were resistant to ceftriaxone (MICs, 16 to ≥32 μg/ml) and ceftazidime (MICs ≥16 μg/ml) but susceptible to meropenem (MICs, ≤1 μg/ml). Six (75%) were coresistant to trimethoprim-sulfamethoxazole and 3 (38%) to levofloxacin. All 8 contained a CTX-M group 1 β-lactamase gene; 7 (88%) had blaCTX-M-15 (Table 1). The closest PFGE profile similarity level was 83% (Fig. 1).
Table 1.
Phylogenetic background, ESBL variant, and virulence determinants of 8 ESBL-positive pediatric Escherichia coli urine isolates
| Trait | Trait profile of isolatea: |
|||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2a | 2b | 3 | 4 | 5 | 6 | 7 | |
| Phylogenetic group | D | D | D | B2 | D | A | D | B2 |
| ST131 present | No | No | No | Yes | No | No | No | Yes |
| ESBL variant | CTX-M-15 | CTX-M-15 | CTX-M-15 | CTX-M-15 | CTX-M-15 | CTX-M group 1 | CTX-M-15 | CTX-M-15 |
| Adhesin gene(s) | fimH, hra | afa/draBC, hra, iha | fimH | fimH | fimH, hra | None | papAH/C/EF/GII, iha, hra, fimH | fimH, hra |
| Toxin gene(s) | hlyF, tsh | sat | None | sat | hlyF, tsh, vat | None | hlyD, sat | None |
| Siderophore gene(s) | iroN, fyuA, iutA | fyuA | fyuA | fyuA, iutA | iroN, fyuA | fyuA, iutA | fyuA, iutA | fyuA, ireA |
| Protectin or invasin gene(s) | K15, traT | K5, traT | kpsMTII | K2, traT | iss, traT | traT | K2 | K1, ibeA |
| Miscellaneous gene(s) | iss, cvaC | malX | ompT, malX | ompT, usp, malX | ompT | None | malX | ompT, usp |
Virulence determinant gene and product designations: fimH, type 1 fimbriae; fyuA, yersiniabactin receptor; kpsMII, group II capsule synthesis; traT, serum resistance-associated outer membrane protein; afa/draBC, Dr-binding adhesins; ibeA, invasion of brain endothelium; papC, pilus assembly; papA, P fimbrial structural subunit; iutA, aerobactin receptor; cvaC, colicin V; usp, uropathogenic-specific protein (bacteriocin); ireA, iron-regulated element (siderophore receptor), iroN, catechole siderophore receptor; iss, serum survival gene; ompT, outer membrane protease; sat, secreted autotransporter toxin; tsh, autotransporter; hlyD, α-hemolysin; hlyF, variant hemolysin; vat, vacuolating toxin; K5, group 2 capsule variant (shown above); K15, group 2 capsule variant (shown above); malX, pathogenicity island marker; hra, pathogenicity island marker.
Fig 1.
Pulsed-field gel electrophoresis analysis of 8 CTX-M-positive pediatric Escherichia coli urine isolates from 7 patients. PFGE, pulsed-field gel electrophoresis pulsotype; Phylo, phylogenetic group; ST131, positive (POS) or negative (NEG) for ST131; FQ, fluoroquinolone resistant (R) or susceptible (S); CTX-M-15, positive or negative for blaCTX-M-15.
Seven (88%) isolates were from virulence-associated phylogenetic group B2 (n = 2) or D (n = 5) (Table 1). Both group B2 isolates represented ST131. All isolates contained numerous extraintestinal pathogenic E. coli (ExPEC)-associated virulence determinants from various functional categories (Table 1). The ST131 isolates' virulence genotypes resembled those of previously reported ST131 isolates (4–6).
Of the 7 patients (ages, 2 months to 6 years), 5 were female (Fig. 1). All were evaluated initially in the Emergency Department (ED), usually for fever. Only 4 (57%) had an identifiable ESBL-associated risk factor (premature birth, health care worker mother, day care attendance, or prior antibiotic exposure). Most received ceftriaxone empirically in the ED, followed by an intramuscular (i.m.) or oral (p.o.) β-lactam agent. Patient 2, who responded well clinically to oral trimethoprim-sulfamethoxazole after a single ceftriaxone dose, returned 1 month later for a new (different strain) episode and received one dose of ceftriaxone for 5 days. Telephone follow-up confirmed, for all 8 episodes, no further symptoms after the initial ED visit and subsequent therapy, despite uniform in vitro resistance to ceftriaxone (MICs, all at ≥16 μg/ml) and, for the trimethoprim-sulfamethoxazole-treated episode, trimethoprim-sulfamethoxazole.
Enterobacteriaceae producing CTX-M enzymes, especially in community-onset infection, are an emerging public health threat (7, 8). Here we document community-associated urinary tract infections among U.S. children, predominantly due to CTX-M-15-producing E. coli, and describe the organisms, which resemble CTX-M-15-producing E. coli from adults, including the presence of the epidemic ST131 clonal group (5), extensive virulence genotypes, and coresistance to fluoroquinolones (75%) and trimethoprim-sulfamethoxazole (25%).
Notably, only 4 children exhibited established ESBL-associated risk factors (1). Accordingly, to ensure appropriate empirical therapy, ED physicians may need to consider the possibility of community-acquired ESBLs, even in pediatric patients who lack identifiable risk factors, especially in high-prevalence locales for ESBL-producing E. coli (11, 12).
Isolates 2a and 2b, recovered 1 month apart from the same patient, exhibited distinct PFGE profiles and gentamicin phenotypes, indicating reinfection with a different CTX-M-15-positive strain. This patient's ESBL-associated risk factor was her health care worker mother, a scenario suggesting possible repeated introduction of diverse health care-associated, ESBL-producing E. coli strains into the household from the mother's workplace (4, 8).
These 7 children all did well. However, the unfavorable international experience with invasive pediatric ESBL-positive enterobacterial infections, including neonatal meningitis and bacteremia (2, 9), urges heightened vigilance and provision of appropriately targeted antimicrobial therapy, now that virulent-appearing, ESBL-producing E. coli strains are present among community-dwelling pediatric patients in the United States.
ACKNOWLEDGMENTS
This material is based upon work supported by the BMA Medical Foundation (C.U.) and Office of Research and Development, Medical Research Service, Department of Veterans Affairs (J.R.J.).
Footnotes
Published ahead of print 17 January 2012
Contributor Information
Krystina L. Woods, Department of Medicine New York Hospital Queens Flushing, New York, USA
James R. Johnson, Veterans Affairs Medical Center Minneapolis, Minnesota, USA
Sofia Padkowsky, Universidad Iberoamericana (UNIBE) School of Medicine Santo Domingo, Dominican Republic.
Noriel Mariano, Infectious Disease Section New York Hospital Queens Flushing, New York, USA.
Rita Colon-Urban, SUNY College at Old Westbury Old Westbury, New York, USA.
Mahmoud Hassanein, Department of Pediatrics, New York Hospital Queens Flushing, New York, USA.
Wehbeh Wehbeh, Infectious Disease Section New York Hospital Queens Flushing, New York, USA.
Connie Clabots, Veterans Affairs Medical Center Minneapolis, Minnesota, USA.
Carl Urban, Infectious Disease Section New York Hospital Queens Flushing, New York, USA.
REFERENCES
- 1. Azap OK, et al. 2010. Risk factors for extended spectrum-β-lactamase positivity in uropathogenic Escherichia coli isolated from community-acquired urinary tract infections. Clin. Microb. Infect. 16:147–151 [DOI] [PubMed] [Google Scholar]
- 2. Boyer-Mariotte S, et al. 2008. CTX-M-15-producing Escherichia coli in fatal neonatal meningitis: failure of empirical chemotherapy. J. Antimicrob. Chemother. 62:1472–1474 [DOI] [PubMed] [Google Scholar]
- 3. Reference deleted.
- 4. Johnson JR, et al. 2009. Epidemic clonal groups of Escherichia coli as a cause of antimicrobial-resistant urinary tract infections in Canada, 2002 to 2004. Antimicrob. Agents Chemother. 53:2733–2739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Johnson JR, Johnston B, Clabots C, Kuskowski MA, Castanheira M. 2010. Escherichia coli sequence type ST131 as the major cause of serious multidrug-resistant E. coli infections in the United States (2007). Clin. Infect. Dis. 51:286–294 [DOI] [PubMed] [Google Scholar]
- 6. Nicolas-Chanoine M-H, et al. 2008. Intercontinental emergence of Escherichia coli clone O25:H4-ST131 producing CTX-M-15. J. Antimicrob. Chemother. 61:273–281 [DOI] [PubMed] [Google Scholar]
- 7. Owens RC, Jr, et al. 2011. Community transmission in the United States of a CTX-M-15-producing sequence type ST131 Escherichia coli strain resulting in death. J. Clin. Microbiol. 49:3406–3408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pitout JD, Laupland KB. 2008. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect. Dis. 8:159–166 [DOI] [PubMed] [Google Scholar]
- 9. Ramdani-Bouguessa N, et al. 2006. CTX-M-3 and CTX-M-15 extended-spectrum β-lactamases in isolates of Escherichia coli from a hospital in Algiers, Algeria. J. Clin. Microbiol. 44:4584–4586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Reference deleted.
- 11. Tiruvury H, et al. 2012. Identification of CTX-M β-lactamases among Escherichia coli from the community in New York City. Diagn. Microbiol. Infect. Dis. 72:248–252 [DOI] [PubMed] [Google Scholar]
- 12. Urban C, et al. 2010. Identification of CTX-M β-lactamases in Escherichia coli from hospitalized patients and residents of long-term care facilities. Diagn. Microbiol. Infect. Dis. 66:402–406 [DOI] [PubMed] [Google Scholar]