Abstract
We describe the rationale, method, and intake demographic and clinical findings of the Harvard/Brown Anxiety Research Project-Phase II (HARP-II). HARP-II is the first prospective, observational, longitudinal study to describe the characteristics and course of anxiety in African American, Latino, and Non-Latino White individuals. Participants met criteria for at least one of the following disorders: Generalized Anxiety Disorder, Social Phobia, Panic Disorder with or without Agoraphobia, Agoraphobia without history of Panic Disorder, Posttraumatic Stress Disorder. Initial intake data, collected between 2004 and 2011, are presented for 165 African American, 150 Latino, and 172 Non-Latino White participants. Participants evidenced substantial psychiatric comorbidity (mean number of Axis I disorders = 3.4), and moderate to severe symptoms and functional impairment. HARP-II will examine clinical course, in the context of potential socio-cultural and individual moderators (e.g., discrimination, acculturation, negative affect). Results should lead to improved understanding, prognostics, and treatment of anxiety in diverse populations.
Keywords: longitudinal study, anxiety, African American, Latino, Hispanic, ethnicity, minority
1. Introduction and Study Rationale
Anxiety disorders are the most common class of mental health disorders in the U.S. (Kessler et al., 2005). Although much progress has been made in understanding and predicting the clinical course of anxiety disorders, substantial gaps exist in the literature regarding African Americans, Latinos and non-Latino Whites. This is of particular public health significance given that currently African Americans and Latinos each comprise approximately 13% of the population, and by 2030, it is projected that approximately 35% of the U.S. population will be of these backgrounds (20% Latino and 15% African Americans; (U.S. Census Bureau, 2004, www.census.gov/ipc/www/usinterimproj/). Despite the increasing and substantial number of African American and Latino individuals in the U.S., there are yet no published data on the clinical course of adult anxiety disorders collected using a prospective longitudinal design in these populations.
The Harvard/Brown Anxiety Research Project (HARP) is a prospective, observational, longitudinal study of anxiety disorders that has been following participants for over 22 years. HARP is one of few studies examining the long-term course of anxiety disorders and has produced findings on the chronic and debilitating nature of anxiety disorders. For example, in 12 years of follow-up the probabilities of recovering from social phobia (SP), panic disorder with agoraphobia (PDA), and generalized anxiety disorder (GAD) were very low (.37, .48, .58 respectively) and lower than comorbid major depressive disorder (.73)(Bruce et al., 2005). Moreover, for those individuals who do recover, many relapse, with cumulative probabilities of relapse ranging from .39 for SP to .58 for PDA. HARP revealed numerous predictors of a worse anxiety disorder course, such as psychiatric comorbidity (Bruce et al., 2005, Yonkers, Dyck, Warshaw, & Keller, 2000), lower socio-economic status (Warshaw, Massion, Shea, Allsworth, & Keller, 1997), single / divorced marital status (Steketee et al., 1999), poor relationships (Yonkers et al., 2000), and an earlier age of onset (Warshaw et al., 1997). Though HARP has significantly contributed to the understanding of the naturalistic course of anxiety, a major limitation of the original HARP cohort is that 97% of the sample is Non-Latino White.
A number of recent epidemiological studies have begun to examine the prevalence of anxiety and other psychiatric disorders in various racial and ethnic groups including African Americans and Latinos (Alegria et al., 2007a; Breslau et al., 2006; Grant et al., 2006; Huang et al., 2006; Riolo, Nguyen, Greden, & King, 2005; Smith et al., 2006; Williams et al., 2007a; Williams et al., 2007b). Two of the largest of these studies are the National Latino and Asian American Study (NLAAS; Alegria et al., 2004) and the National Survey of American Life (NSAL, Jackson et al., 2004), which were designed to be comparable to the National Comorbidity Study – Replication (NCS-R; Kessler et al. 2004). Findings from the NCS-R have estimated the lifetime prevalence of anxiety disorders to be approximately 25% in Latinos, 24% in African Americans, and 29% in Non-Latino Whites (Breslau et al., 2006). African Americans had a significantly lower rate of anxiety disorders than did Non-Latino Whites.
More recently, NLAAS authors reported a lifetime prevalence of all psychiatric disorders in Latinos that ranged from 28% for men to 30% for women (Alegria et al., 2007). Although this study has not yet reported prevalence rates for specific anxiety disorders, NLAAS findings reveal that higher rates of psychiatric disorders were associated with being Puerto Rican, US-born, third-generation Latino, and English-language-proficient. As the NCS-R included only English speaking Latinos, it seems likely that the NLAAS will find lower rates of anxiety disorders than found in Non-Latino Whites from the NCS-R.
Findings from NSAL indicate that, when compared to a Non-Latino White sample from the NCS-R, the prevalence of many anxiety disorders (GAD, PD, and SAD) is lower among African Americans than Non-Latino Whites, though the prevalence of PTSD is significantly greater among African Americans (Himle, Baser, Taylor, Campbell, & Jackson, 2009). Further, levels of mental illness severity and disability were greater among African Americans than Non-Latino Whites. That is, though African American participants were less likely to suffer from many of the anxiety disorders, those who did have an anxiety disorder were more greatly impaired than their Non-Latino White counterparts. Caribbean Black respondents with anxiety disorders were the most likely to have severe symptoms and functional problems (Himle et al., 2009).
In another large epidemiological study, the National Epidemiologic Survey on Alcohol and Related Conditions, lower 12-month prevalence rates of anxiety disorders were observed in both Blacks (10.4%) and Latinos (8.8%) compared to Whites (11.7%) (Huang et al., 2006). However, a study of 1,803 young adults (age 19–21) living in Florida (Turner & Gil, 2002) found somewhat different results. There were no differences in overall prevalence of anxiety disorders between African Americans, Cubans, foreign-born non-Cuban Latinos, and Non-Latino Whites. However, this study excluded Caribbean Blacks. Further, non-Cuban Latinos born in the U.S. were found to have a higher lifetime prevalence of anxiety disorders (19.9%) as compared to Non-Latino Whites (14.6%). This underscores the potential importance of examining nationality and birth in or outside the U.S. when examining the nature and course of anxiety disorders in African Americans (e.g., Caribbean Black or not) and Latinos.
While this data is accumulating on the prevalence and cross-sectional severity of anxiety disorder in minority populations, none of the studies in this area include prospective, longitudinal assessments of clinical course. Thus, there are no published data on the prospectively observed clinical course of anxiety and other psychiatric disorders in African American or Latino adult samples.
1.1. Potential Ethno-racial Differences / Minority Mental Health Disparities in DSM-IV Anxiety Disorder Course
Epidemiological data suggest that ethno-racial disparities may be most observable in the persistence, rather than prevalence, of anxiety disorders (Breslau et al., 2005; 2006). In their work, individuals with anxiety disorders were asked to retrospectively recall the year in which their symptoms first began. Breslau and colleagues concluded that anxiety disorders may be more persistent in minority samples than in Non-Latino Whites because their retrospectively recalled duration of illness was longer. However, the validity of this finding is unclear, due to the reliance on a one-time, retrospective recollection. No other data is available on ethno-racial differences in anxiety disorder course, and no research to date has examined the time-varying variables that may moderate course (e.g., do changes in social economic status or degree of acculturation over time relate to changes in course of anxiety disorders?) or on the detailed nature of disorder course (e.g., time to recovery, time to recurrence, length of well intervals).
1.2. Nature and Course of Culture-Bound Syndromes and Culturally-Relevant Expressions of Anxiety
Culturally-specific syndromes related to anxiety have been described (e.g., Guarnaccia, Rubio-Stipec. & Canino, 1989; Lewis-Fernandez et al., 2002; Baer et al., 2003; Bell et al., 1984; Fukuda, 1993; Douglass et al., 1994), but little empirical research exists specifying the nature or course of many of these syndromes. The most fully described culture-bound syndrome closely related to anxiety is ataques de nervios (Guarnaccia et al.,1989; Lewis-Fernandez et al., 2002). This syndrome is characterized by a sense of being out of control and symptoms including uncontrollable shouting, crying, trembling, and occasionally dissociative experiences, aggression, and/or fainting. In the NLAAS, 5.4 to 10.9% of the Latino sample reported experiencing ataques, with Puerto Ricans having the highest prevalence (Guarnaccia et al., 2010). Ataques have been repeatedly found to be associated, cross-sectionally, with an increased likelihood of having a DSM mental health disorder, including anxiety disorders. However, data is lacking on the course of ataques over time, on how this syndrome may influence the course of DSM psychiatric disorders longitudinally, and on how this syndrome may be associated with anxiety-relevant traits, such as negative affect and anxiety sensitivity, over time.
Mal de ojo (the evil eye) and susto (fright or soul loss), are also documented in the DSMIV-TR (APA, 2000). Recent work has better described these syndromes and begun to examine their prevalence (e.g., Baer et al. 2003; Bayles & Katerndahl, 2009; Weller, Baer, de Alba Garcia, & Rocha, 2008). Mal de ojo is thought to be inflicted on an individual, as a result of the nefarious and often envious stare of another person. Symptoms of mal de ojo are often physical (e.g., fever, diarrhea) but may be psychological as well. Susto is thought to occur as a response to a frightening event that “causes the soul to leave the body” (APA, 2000) and may be particularly relevant to Latino participants with a trauma history. Little research has examined the nature of these syndromes, and we could not identify any research that examined the course of these syndromes over time, or that has examined the role of anxiety-relevant traits (e.g. anxiety sensitivity, negative affect) in the presentation of these syndromes. In one of the few studies examining both of these syndromes (Bayles & Katerndahl, 2009), a 10-minute survey was administered to 100 Latino primary care patients, who were primarily of Mexican decent. Participants reported high rates of lifetime experience with mal de ojo (10%), susto (14%), and ataques de nervios (6%). Moreover, the occurrence of ataques was significantly correlated with susto.
Though not truly a culture-bound syndrome, sleep paralysis (the temporary loss of voluntary muscle movement upon wakening or falling asleep), is thought to be more frequent in African Americans, and most frequent in individuals with panic disorder, PTSD, and/or history of trauma (Ohayon & Shapiro, 2000; Paradis, Friedman, & Hatch, 1997; Sharpless et al., 2010; Sharpless & Barber, 2011; Steine et al., 2011). A recent systematic review (Sharpless & Barber, 2011) attempted to estimate the pooled prevalence rates for sleep paralysis across 35 studies. The authors estimate that sleep paralysis occurs in approximately 7.6% of the general population, 34.6% of patient samples with panic disorder, and as many as 44.3% of African Americans with psychiatric disorders such as panic disorder. There is no existing data on the longitudinal course of sleep paralysis, or its relationship to anxiety disorders over time.
For all of these culturally-relevant anxiety-related syndromes, data is lacking regarding course and relationship, over time, to other anxiety symptoms and functioning.
1.3. Potential Moderators of Course of Anxiety Disorders of Particular Relevance to Ethno-racial Minorities
1.3.1. Treatment Received / Mental Health Treatment Disparities
Ethno-racial minorities suffer health care disparities in access to and quality of treatment (Atdjian & Vega, 2005; Schraufnagel, Wagner, Miranda, & Roy-Byrne, 2006). Recent studies have begun to examine the unmet need for mental health services in African Americans (Jackson et al., 2007; Neighbors et al. 2007) and Latinos (Alegria et al., 2007b; Vega et al., 2007). Breslau et al. (2005) suggest that although there are assumptions that ethnic disadvantage in treatment received may be a source of the increased persistence of mood and anxiety disorders, this issue suffers from a lack of empirical data. Further, they report that the ethno-racial differences observed in the persistence of disorders remained after controlling for treatment differences. To date, Breslau et al. (2005) is the only study that examines if disparities in treatment for mood and anxiety disorders offer a partial explanation for any existing ethno-racial disparities in course of anxiety disorders.
1.3.2. Environmental Stressors
Cultural differences in stressful life conditions may be a risk factor contributing to potential ethno-racial disparities in the course of anxiety and depressive disorders (Breslau et al, 2005). Stressors that vary between cultural groups range from the relatively common experience of major life stressors to less frequent, but impactful events such as trauma exposure. Some studies suggest that ethno-racial minorities are at higher risk for certain types of trauma exposure, such as assault violence (Breslau et al., 1998) and for the development of PTSD (Koenen, Stellman, Stellman, & Sommer, 2003). Observed cross-cultural differences in trauma exposure may be partly accounted for by demographic variables such as lower income, residence in high crime neighborhoods, and less education (Adams & Boscarino, 2005; Brewin et al., 2000; Galea et al., 2004).
1.3.3. Country of Origin and Duration of U.S. Residence
Factors such as country of origin and time spent in the U.S. may impact the course of anxiety disorders. The NSAL study of mental disorders in the black population of the U.S. suggests that black Caribbean-born female immigrants to the U.S. had a lower 12-month risk of anxiety disorders, substance abuse, and any mental disorder compared to other African Americans. Longer length of residence in the U.S. was associated with increased risk of lifetime mental disorders for all Caribbean immigrants (Williams et al., 2007b). Similar findings have been reported from the NLAAS (Alegria et al., 2007c), which showed that U.S. origin and increased duration of residence were associated with greater mental health burden in Latino individuals. Differences due to length of residence were accounted for by family stressors, contextual factors and social status factors.
1.3.4. Social Economic Status
Anxiety disorders may be influenced by access to resources in the environment and thus indicators of social status such as income and education may be relevant moderators of anxiety disorder course. A number of studies have shown that low income is associated with increased prevalence and severity of anxiety disorders (e.g. Kessler, Mickelson, & Williams, 1994; Roy-Byrne, Russon, Cowley, & Katon, 2003). Further, this relationship may not be solely due to access to at least minimally adequate mental health treatment (Roy-Byrne Joesch, & Wang; 2009). The association between social economic status (SES) and anxiety is complicated in that whereas lower SES may set a context for the development of more anxiety, it is also true that anxiety disorders may lead to work dysfunction and reduced SES. Interestingly, perceived social status (a perception of one's social status relative to others in the U.S. based on money, education, and job respect) has been suggested to be an even more relevant correlate of risk for anxiety disorders (Alegria et al., 2007c), than objective indicators such as income and education.
1.3.5. Acculturation and Enculturation
Alegria et al. (2007c) provide a comprehensive description of the complex issues associated with studying adaptation to a new culture. They differentiate the construct of acculturation (acquisition of cultural elements of the dominant society) from the process of enculturation (which focuses on preserving the norms of the native group). The authors argue that both processes can occur simultaneously and should be measured separately as potential contributors to mental health. To date, little research has examined the roles of acculturation and enculturation in mental health functioning, and no studies have investigated the long-term dynamics of these processes in relation to anxiety disorders.
1.3.6. Experienced Discrimination
Experienced (or self-reported) racial or ethnic discrimination is associated with worse self-reported physical and mental health (Borrell et al., 2006; Gee, Ryan, Laflamme, & Holt, 2006; Seller, Bonham, Neighbors, & Arnell, 2009; Finch, Kolody, & Vega, 2000; Siefer, Finlayson, Williams, Delva, & Ismail, 2007) in community samples. There are a few studies demonstrating associations between experienced discrimination and anxiety disorders. Kessler and colleagues (1999) found that self-reported discrimination (based on race/ethnicity, gender, religion, age, or other factors) was associated with major depression and generalized anxiety disorder. Another study which utilized a more comprehensive assessment of DSM-IV mental disorders, (Alegria et al., 2007c; Gee, Spencer, Chen, Yip, & Takeuchi, 2007) found that self-reported racial discrimination was associated with a greater probability of having any DSM-IV disorder, depressive disorder, or anxiety disorder within the past 12 months, controlling for socio-demographic characteristics and other variables.
1.3.7. Family Burden and Family Cultural Conflict
Family burden refers to demands from immediate and extended family members. Family cultural conflict refers to conflict with family around issues affected by cultural beliefs, such as career goals. Minorities from families in which different members are at different levels of acculturation and enculturation may experience higher rates of family conflict. Alegria et al. (2007c) suggest that family burden and family cultural conflict are associated in cross-sectional analyses with an increased risk for 12-month prevalence of anxiety and depressive disorders in Latino individuals.
1.3.8. The Need for Longitudinal Data
Research has begun to examine the relationship between anxiety and a number of individual and societal factors, with particular relevance to ethno-racial minority samples (i.e. treatment received, environmental stressors, country of origin, duration of U.S. residence, SES and perceived social status, acculturation, enculturation, perceived discrimination, family burden, family cultural conflict). However, the lack of prospective studies on the course of anxiety disorders in minority samples has caused a dearth of knowledge regarding how these constructs may affect the long-term course of anxiety. Further, many of these variables are time-varying, rather than static. For example, duration of time in the U.S. increases each year an individual continues reside in this country. Income varies with as individuals find better work or are laid off. Degree of acculturation may increase over time, etc. There is a need for longitudinal studies that may examine how anxiety and functioning change over time, as individuals and their lives change.
1.4 HARP–II Specific Objectives
Given the absence of available data on the clinical course of anxiety disorders in African Americans and Latinos, and the possibility that the socio-cultural factors described above may moderate the course and outcome of anxiety disorders, the aims of HARP-II are:
AIM 1: Create the first comprehensive description of the prospective clinical course of psychopathology and psychosocial functioning associated with anxiety disorders in African Americans, Latinos, and Non-Latino Whites.
AIM 2: Test hypothesized predictors (e.g. nativity/immigration status; perceived social status; acculturation and enculturation; experienced discrimination; family burden and family cultural conflict) of the prospective clinical course of psychopathology and psychosocial functioning associated with anxiety disorders within each of the 3 ethnic groups.
AIM 3: Compare the prospective clinical course and outcome of anxiety disorders among African Americans, Latinos, and Non-Latino Whites.
AIM 4. Identify which within-group predictor variables vary by ethnicity and are associated with between- group differences in prospective course and outcome of anxiety disorders. That is, we will first examine which demographic, clinical, treatment history, and environmental stressor variables studied as within-group predictors in Aim 2 show significant variation across ethno-racial groups and then incorporate the most salient predictors that emerge to test the hypothesis that socio-cultural variables will be associated with ethno-racial differences in course.
2. Method
2.1. Design
HARP-II is an on-going prospective, observational, longitudinal follow-up study of adults with the following designated “index” anxiety disorders: Panic Disorder without Agoraphobia (PD), Panic Disorder with Agoraphobia (PDA), Agoraphobia without history of Panic Disorder (AWOPD), Generalized Anxiety Disorder (GAD), Posttraumatic Stress Disorder (PTSD), and Social Phobia (SP). The full design of the study includes an intake interview, and then yearly follow-up assessments. All intake interviews are in person. Follow-up interviews are generally completed via telephone. We present here intake data only for participants enrolled as of April of 2011.
2.2. Participants
Data presented here are from the first 439 consecutive individuals enrolled in HARP-II. Recruitment and enrollment in HARP-II is still ongoing. Our total recruitment goal is 525 participants; consisting of at least 175 African American, 175 Latino, and 175 Non-Latino White individuals with anxiety disorders. As of April of 2011, we have recruited nearly 84% of what will be our total sample. Data is thus presented in section three for our three, non-mutually exclusive groups: 165 African Americans, 150 Latinos, and 173 Non-Latino Whites (total is greater than 439 due to participants who are endorsed more than one ethno-racial category). Participants were recruited between 2004 and 2011.
2.2.1. Inclusion and exclusion criteria
Inclusion criteria are 18 years of age or older, English speaking1, presence of one or more of the intake anxiety disorders, and able to provide informed consent. Exclusion criteria are schizophrenia, active psychosis, and organic mental disorder at intake.
2.2.2. Recruitment
During the initial phase of recruitment, treatment providers in our geographic area referred prospective eligible participants. After some months of utilizing this method, we explored additional methods in order to increase enrollment rates, including newspaper, internet, and postings on mass transit. This direct outreach proved to be the most effective method of obtaining a rate of enrollment that would ensure our meeting our target objective. In total, 42 participants were recruited via referral, 260 from advertisement (newspaper, internet, bus), 38 from a family member or friend, and 99 from some other source.
2.3. Procedures
The study was approved by the institutional review board of Brown University and all participants provided written informed consent prior to enrollment. Potential participants were first briefly screened over the phone for the presence of anxiety symptoms. From 2004 to 2010, the only initial ineligibility at this phone screening was due to a lack of endorsement of anxiety symptoms or the presence of psychotic symptoms. Beginning in 2010, we employed targeted enrollment for the African American group, as preliminary examination of some key demographic variables showed significant between racial group differences. For example, after discovering that our sample of African American participants were significantly more likely to be older, unemployed, have lower incomes, and less education than the other two samples, we attempted to schedule more intake interviews with African American participants under the age of 35 who were employed, graduated from college, and had incomes above $35,000.
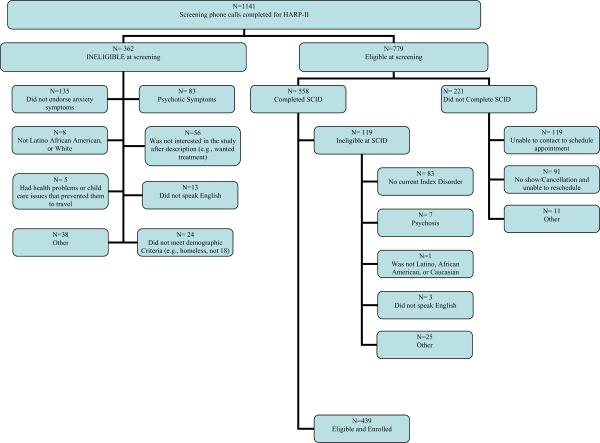
Individuals who are eligible and endorse any anxiety symptoms at screening are invited for an intake interview. Participants are compensated $60 for participating in intake interview, which is, on average three hours in duration. At the end of the intake interview, participants who meet all inclusion and none of the exclusion criteria (see section 2.2.1) are enrolled in the study. See Figure 1 for a flow chart depicting participant eligibility and enrollment.
Figure 1.
Enrollment Flowchart. This figure presents the number of participants found eligible or ineligible at each stage of enrollment screening and the reasons why participants were not enrolled.
Participants are then contacted again regularly, for follow-up interviews. The first 60 participants were interviewed 6 and 12 months following the intake interview, and yearly thereafter. For budgetary reasons, after October 2008, the 6 month interview was dropped and all participants were interviewed at 12 months post-intake and yearly thereafter. Data are here presented for the intake assessment only.
2.3.1. Intake Measures
A complete list of measures is presented in Table 1. We selected established measures with good psychometric properties when available. When such measures were unavailable we borrowed measures from the National Latino and Asian American Study (NLAAS; see Alegria et al., 2004; 2007a) or, in some instances, used measures we had designed for the original HARP cohort. HARP-II interviews assess demographic, clinical, socio-cultural, and functioning domains.
Table 1.
Baseline and Follow-up Measures in HARP-II
| Construct | Measure | Method |
|---|---|---|
| Baseline | ||
| Demographics | Demographic Questionnaire | Int |
| Age, Gender, Marital status | ||
| Race, Ethnicity | ||
| Country of birth (participant, parents, grandparents) | Languages spoken, Age of immigration | |
| Education, Occupation, Income | ||
| Environmental Stressors | ||
| Trauma exposure | Trauma Assessment for Adults (Revised) | Int |
| Diagnostic Status and Symptom Severity | ||
| Axis I Diagnoses | SCID-IV | Int* |
| Suicide history | LIFE Suicide History Assessment | Int |
| Panic symptom severity | Sheehan Panic and Anticipatory Anxiety Scale | Int |
| Social anxiety symptom severity | Liebowitz Social Anxiety Scale (LSAS) | Int† |
| Trait affect | Positive and Negative Affect Scale – Expanded Form (PANAS-X) | SR |
| Anxiety sensitivity | Anxiety Sensitivity Index (ASI) | SR |
| Agoraphobic impairment | Mobility Inventory (MI) | SR |
| Culturally Relevant Psychopathology | ||
| Ataque de nervios | NLAAS Ataque de nervios Interview | Int |
| Somatic symptoms | NLAAS 35-item somatic symptoms interview | Int |
| Sleep paralysis | Sleep Paralysis Questionnaire | Int |
| Mal de ojo and Susto | Assessment of Culturally-Specific Attributions Regarding Symptoms | Int |
| Sociocultural Factors | ||
| Social status | Perceived Social Status Questionnaire | Int |
| Acculturation | 3-Item English Language Proficiency Scale | Int |
| Enculturation | 3-Item Spanish Language Proficiency Scale, Ethnic Identity Scale | Int |
| Family stress | Family Burden (2-item) & Family Cultural Conflict (5-item) Scale | Int |
| Discrimination | Experiences of Discrimination Scale (Revised) | Int |
| Acculturative Stress | 9-item Acculturative Stress Scale | Int |
| Social Embeddedness | 10-item Social Embeddedness Scale | Int |
| Treatment Received | ||
| Past and current treatment (medication, therapy, hospitalization, etc.) | History of Treatment Questionnaire | Int |
| Barriers to treatment | Treatment Not Received Form | Int |
| Functioning | ||
| Psychosocial (relationships, work, role) | LIFE Base, Global Assessment of Functioning (GAF) | Int |
| RAND 36-Item Health Survey | SR | |
| Physical (pain, role) | RAND 36-Item Health Survey | SR |
| Yale New Haven Health Survey | Int | |
| Presence of serious medical conditions | Charlson Comorbidity Index (CCI) | Int |
| Additional Measures Administered at Follow-up | ||
| Stressful life events | LEA | Int |
| Symptomatic status (in episode, recovery, relapse) | Longitudinal Interval Follow-Up Evaluation (LIFE) | Int |
| Psychosocial treatments received | Psychosocial Treatment Interview | Int |
| Social Support | Kessler Perceived Social Support Scale | Int |
Note. All baseline measures except the SCID are also administered at follow-up assessment; SR = self-report; Int = interview
Not administered at follow-up
LSAS administration ended in 2008
2.3.1.1. Demographic Characteristics
Demographic characteristics are assessed with an interviewer-administered questionnaire. Participants are asked to provide information about their age, marital status, etc. They are also asked about country of origin and languages spoken for themselves, parents, and grandparents. They are also asked about their age of immigration, if applicable.
2.3.1.2. Clinical Characteristics
Diagnostic status and eligibility at intake is assessed with the Structured Clinical Interview for DSMI-IV Axis I Disorders-Non-Patient Version (SCID-IV-NP) (First, Spitzer, Gibbons, & Williams, 1996). The B/C screening module is also used to screen out patients with psychosis.
Suicide History is assessed with the LIFE Suicide History Assessment which gauges the frequency, lethality, and degree of intent for past suicide attempts and gestures, as well as the most severe suicide attempt, including age and date of the attempt, stressors present at the time of the attempt, and subsequent psychiatric or medical hospitalization (Keller et al., 1987; Warshaw, Keller, & Stout, 1994).
Symptom severity is assessed with the Sheehan Panic and Anticipatory Anxiety Scale (Bakish et al., 1996; Davidson et al., 1994), the Mobility Inventory (MI); Chambless, Caputo, Jasin, Gracely, & Williams, 1985; Cox, Swinson, Kuck, & Reichman, 1993; Craske, Rachman, & Tallman, 1986), and the Liebowitz Social Anxiety Scale (LSAS; Liebowitz, 1987; Heimberg et al., 1999),
Trauma exposure / environmentals stressors are assessed with a revised version of the Trauma Assessment for Adults (Resnick, Best, & Freedy, 1993; Resnick, 1996).
Trait characteristics are assessed with Positive and Negative Affect Scale – Expanded Form (PANAS-X; Watson, Clark, & Tellegen, 1988) and the Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally,1986; Peterson & Reiss, 1993; Rodriguez, Pagano, & Keller, 2004)
2.3.1.3. Culturally Relevant Psychopathology
Ataque de nervios Interview
The NLAAS 39-item interview assessing ataque de nervios is used (Alegria et al., 2004). This interview asks about the existence of symptoms, the interference caused by the syndrome, frequency of “nervous episodes”, age of onset, and precipitating events to the episodes. Individuals are coded as having experienced an ataque de nervios if they endorse the entry question “Have you ever had an ataque de nervios, or episode or nervous attack when you felt totally out of control?” and then endorse at least 4 of 15 possible symptoms accompanying the ataque.
Somatic symptoms
Since somatic symptoms are a common manifestation of anxiety and depression in Latinos, HARP uses a measure of somatic symptoms from NLAAS (Alegria et al., 2004). It comprises a list of 35 specific somatic symptoms and unexplained chronic pain adapted from the NLAAS chronic conditions measure.
Sleep paralysis
The Mellman Sleep Paralysis Questionnaire (Mellman, Aigbogun, Graves, Lawson, & Alim, 2007) assesses the presence of sleep paralysis. It contains a screening question along with additional items about frequency and duration of sleep paralysis episodes as well as associated symptoms.
Mal de ojo and Susto
Mal de ojo (the evil eye) and susto (fright or soul loss) are assessed by inquiring about culturally-specific attributions participants may make about their symptoms. At the end of the interview, participants are asked whether they believe that any of the symptoms or problems discussed are caused by mal de ojo or susto. Additional probes are used to assess which symptoms are believed to be caused by mal de ojo or susto.
2.3.1.4. Socio-cultural Factors
Perceived Social Status Questionnaire
Respondents identify their social status relative to others in the U.S. based on money, education, and job respect; a higher score indicates higher levels of perceived social status and is expected to be protective for anxiety disorders (Alegria et al., 2007c).
Acculturation and Enculturation
As described in Alegria et al. (2007c), acculturation is measured using the English Language Proficiency Scale with higher scores indicating higher-level proficiency and more successful acculturation. Enculturation is measured using the Spanish Language Proficiency Scale and Ethnic Identity Scale. Although we require all of our participants to speak English, the English Language Proficiency Scale nonetheless should be sensitive to individual differences in degree of proficiency.
Family Burden and Family Cultural Conflict
Both of these constructs are measured with items taken from the larger NLAAS interview. Family burden is assessed with a 2-item measure on frequency of demands and arguments with relatives. Family cultural conflict is a 5-item measure tapping respondents' intergenerational and cultural conflict with family members (Alegria et al., 2007c).
Experiences of Discrimination (EOD)
This questionnaire measures nine specific types of daily experiences of racial and ethnic discrimination (Krieger, Smith, Naishadham, Hartman, & Barbeau, 2005).
Acculturative Stress
Nine items assess stressors associated with immigration and change in culture, e.g., discrimination, fear of deportation, limited contact with family and friends, and difficulties with the English language (Alegria et al., 2006).
Social Embeddedness
The 10-item Social Embeddedness Scale assesses the extent and closeness of participants' relationship with relatives, friends, best friends, neighbors, and social organizations. It also assesses participants' satisfaction with the support provided by these relationships (Norris & Murrell 1987).
2.3.1.5. Psychosocial and Physical Functioning
LIFE-Base
The Baseline Psychosocial Functioning section of the Longitudinal Interval Follow-up Evaluation is used to rate the participant's functioning in the worst week of the month prior to the intake interview on the following domains: 1) work: employment status, hours worked in past week; 2) household duties; 3) student work; 4) interpersonal relations with family and friends; 5) recreation: frequency and enjoyment level; 6) overall satisfaction with life; 7) rater assessment: an assessment of overall functioning separate from symptoms. The interrater reliability for items on the LIFE-Base has been found to be good (Keller et al., 1987a).
Global Assessment of Functioning (GAF) (APA, 2000) scores are assigned by the interviewer for the participant's functioning during the month prior to the intake interview based on the worst level that the participant remained at for at least one week..
Functioning is also assessed using The RAND 36-Item Health Survey (Hays, Anderson, & Revicki, 1993) and a modified version of the Yale New Haven Health Survey (Myers,1980; Warshaw et al., 1994).
The Charlson Co-morbidity Index (CCI; Charlson, Ales, & McKenzie., 1987) is used to assess physical health status.
2.3.1.6. Treatment Received
History of Treatment Questionnaire
The history of treatment questionnaire assesses the participant's psychiatric treatment history, including frequency and type of treatment. Participants are asked whether they have ever or in the past six months received a particular treatment (e.g., inpatient hospitalization, therapy, medication, etc.). This measure is adapted from the original treatment section of the LIFE baseline interview and shows high interrater reliability (Keller et al., 1983).
Treatment not Received Form
This measure is designed for use in HARP to clarify why individuals who meet diagnostic criteria for an anxiety disorder are not receiving treatment. It queries about decisions not to pursue pharmacologic and psychotherapeutic treatment. Participants choose among predefined reasons for not pursuing treatment (e.g., financial reasons, ineffective in past, not recommended by provider).
2.3.2. Follow-up Measures
The measures listed above, with the exception of the SCID and the LIFE-Base, are given at all time points (intake and follow-up). Additionally, the following instruments were specifically designed for follow-up interviews:
Longitudinal Interval Follow-Up Evaluation (LIFE)
The LIFE is the core of all follow-up evaluations and is designed to collect detailed information on symptomatic status, psychiatric diagnostic status, somatic treatment received, and psychosocial functioning (Keller et al., 1987). Psychiatric Status Ratings (PSRs), a 6-point measure of symptomatic status (from asymptomatic at PSR=1 to incapacitated at PSR=6), are created separately for each diagnosis based on DSM criteria. PSRs divide the sample into exclusive categories at each week, corresponding to clinically meaningful states. A patient's illness can be reduced to a series of those states – such as full criteria (PSR 5 or 6), partial criteria/subsyndromal (PSR 3 or 4), or recovered (PSR 1 or 2) – along with the time spent in each state. This method is based on an approach originally used in the Collaborative Depression Study (CDS; Keller et al., 1992) and has been successfully used in over 400 different research programs enabling the tracking of course utilizing diagnostic based systems. Separate PSR scales are created for each of the DSM anxiety diagnoses followed by HARP. Using the same method, originated by our lab and in consultation with our cultural psychiatry consultants, additional PSR scales are created to further track the course of each of the culture-bound syndromes.
Symptom Course
To assess symptoms using the PSRs, the interviewer asks how the participant's symptoms have been since the last interview and then probes for change points (e.g., “I had about one panic attack a week until Christmas, but then things got better, and I only had limited symptom attacks until mid-March…”). Individual PSRs are then assigned for each week of follow-up.
Course of Psychosocial Functioning
The Psychosocial Functioning Section of the LIFE interview at follow-up probes the same domains of functioning as this section of the LIFE-Base (see section 2.3.1.6.1). A follow-up rating is created for each month of the follow-up interval. Similarly, a GAF score is assigned to each month of the follow-up interval.
Somatic Treatment
Using the LIFE, the interviewer also records the name and dose of each specific psychotropic medication received, and the weeks during which this treatment is taken.
Psychosocial Treatment Interview (PTI)
This rater-administered instrument records the characteristics and frequency of psychosocial treatment received by participants during the follow-up interval. The PTI inquires about the frequency with which the participant's provider employs any of a series of specific therapeutic techniques during treatment. It is given during each annual follow-up.
Environmental Stressors are assessed with the Life Events Assessment (LEA). The LEA is adapted from the Psychiatric Epidemiology Research Interview Life Events Scale (Dohrenwend, Krasnoff, Askenasy, & Dohrenwend, 1978). HARP's version of the LEA assesses if any of a list of 52 events had occurred since the last follow-up interview. The start date and valence (positive or negative) of stressful life events are also tracked. LEA items assess a number of stress domain categories, such as work or school, family or living circumstances, love relations with a spouse or partner, crime and legal matters, financial matters, physical health, social matters.
Social Support is assessed with the Kessler Perceived Social Support scale and was adapted from adapted from Coventry, Gillespie, Heath, and Martin (2004). The 19-item scale assesses participants' perceived support from their spouse, siblings, children, parents, other relatives, and friends.
2.3.3. Rater Training and Supervision
Interviews are conducted by clinical interviewers with a bachelors or masters degree in psychology or a related field. Interviewers complete a rigorous training program, similar to that described by Warshaw, Dyck, Allsworth, Stout, and Keller (2001), before being certified to conduct intake and follow-up interviews. Training for each type of interview consists of a graduated set of tasks and experiences, beginning with reading relevant papers, studying instruments and instruction booklets, watching training tapes, and reviewing suggestions for handling common interviewing problems. Interviewers then participate in a 1– 2 day didactic session solely focused on the conduct of clinical interviews. They also review and discuss videotapes of interviews conducted by experienced interviewers, and conduct mock interviews. Following this, new interviewers directly observe experienced interviewers as they meet with participants. The next step is for new interviewers to begin to conduct interviews, while being directly observed by training supervisors and/or more experienced interviewers. These interviews are also audio or video-recorded, for close review by training supervisors. Only after conducting at least three closely observed and directly reviewed interviews, and being judged by training supervisors as meeting the needed criteria with regard to both content and process of the assessment, are new interviewers certified to collect data independently.
After certification, all clinical interviewers remain closely supervised. HARP-II clinical staff/faculty (licensed psychologists and/or psychology postdoctoral fellows) review each diagnosis for each case enrolled in the study. Cases are reviewed at a weekly team meeting with clinical interviewers, clinical staff/faculty, and training supervisors. Further, all interviews undergo a rigorous clinical editing process to ensure accuracy of intake diagnoses.
To achieve and maintain calibration among raters regarding follow-up interviews, we videotape one complete interview every three months, alternating raters, resulting in four videotapes per year. All raters watch and rate these tapes independently. The training supervisor monitors the ratings from each interviewer and provides feedback. All interviewers meet every three months to discuss their ratings of the designated tape. Problems are addressed and raters discuss difficult clinical decisions that occurred during the interim. Once sufficient follow-up reliability data has been collected, for each of the raters, the median reliability from the ICCs for all possible pairs of raters will be calculated. This methods also allows identification of any rater who is consistently providing ratings discordant with those of the rest of the interviewers. We have set a high standard of reliability for the raters. Poor calibration of a rater with the rest of the team, serves as a signal for retraining, extra editing, and any other help as needed.
2.3.4. Data management and analytical plans
Course and other data are entered into an interactive on-line hierarchical database. The data entry programs perform extensive checks at the time the data are entered to ensure the longitudinal and cross-sectional integrity of the data. Gaps, overlaps, and inconsistencies in the data are detected and flagged for immediate attention. From the on-line database, data are transferred to SAS data sets for analysis. Initial examination of our data revealed that, thus far, groups appear roughly comparable in terms of most demographic characteristics; however, the Latino group is significantly younger and more educated. We have begun targeted enrollment of older and less educated Latinos. It is our hope that this will yield samples comparable on key demographic characteristics, for eventual use in between group analyses (as planned in Aims 3 and 4; see section 1.4). For subsamples (e.g., examination of participants with social phobia) in which demographic differences exist between ethno-racial groups, we will consider employment of techniques such as case-based matching or propensity matching, as appropriate.
2.3.5. Ethical considerations
The HARP-II protocol is approved and monitored by the Brown University Institutional Review Board. All participants provide informed written consent prior to their intake assessment. HARP attempts to balance the scientific needs of a naturalistic, prospective study with the ethical obligations to participants. Given that several effective treatment options exist for anxiety disorders, HARP-II provides a one-page description of anxiety disorders and treatment referrals to all participants during their intake assessment.
3. Results
3.1. Demographic Characteristics
Demographics are provided on Table 2, for each ethno-racial group. Ethno-racial group membership is not mutually exclusive and is determined in the following manner. First, participants are asked to self-identify their ethnicity (Latino or Non-Latino) and their race (African American/Black, White, Asian, Native American, other) on the demographic questionnaire. All participants self-identifying as Latino are represented in the Latino column of Table 2; all participants self-identifying as African American / Black are represented in the second column. Non-Latino White background is determined via 1) self-identifying as White and as Non-Latino; or 2) self-identifying as White and Latino, AND reporting that at least one parent was born in a non-Latin country or clearly reporting on follow-up questioning that one's background included both Latino and Non-Latino White heritage. Thus, the additive N for each column is greater than the total sample, as there are many individuals who reported membership in more than one, or all three of these ethno-racial groups.
Table 2.
Demographic Characteristics
| African American N= 165 | Latino N = 150 | Non-Latino White N = 173 | |
|---|---|---|---|
| N % | N % | N % | |
| Ethnicity/Race | |||
| Non-Latino White Only | N/A | N/A | 142 (82%) |
| African American only | 142 (86%) | N/A | N/A |
| Latino Only | N/A | 109 (73%) | N/A |
| African American and Latino | 15 (9%) | 15 (10%) | N/A |
| African American and Non-Latino White | 5 (3%) | N/A | 5 (3%) |
| Latino and Non-Latino White | N/A | 23 (15%) | 23 (13%) |
| AA, Latino, and Non-Latino White | 3 (2%) | 3 (2%) | 3 (1%) |
| Country of Birth | |||
| U.S. | 149 (90%) | 76 (51%) | 164 (95%) |
| Outside U.S. | 16 (10%) | 74 (49%) | 9 (5%) |
| Puerto Rico | 1 (1%) | 31 (21%) | 0 (0%) |
| Dominican Republic | 2 (1%) | 12 (8%) | 1 (1%) |
| Other | 13 (8%) | 31 (21%) | 8 (4%) |
| Spanish spoken | |||
| Participant | 11 (7%) | 95 (63%) | 11 (63%) |
| Participant's parent | 19 (12%) | 100 (67%) | 15 (9%) |
| Gender | |||
| Male | 54 (33%) | 41 (27%) | 68 (39%) |
| Female | 111 (67%) | 109 (73%) | 105 (61%) |
| Education | |||
| Less than HS | 25 (15%) | 29 (19%) | 27 (16%) |
| Less than HS | 25 (15%) | 29 (19%) | 27 (16%) |
| HS degree or GED | 51 (31%) | 27 (18%) | 43 (25%) |
| Partial college | 46 (28%) | 37 (25%) | 57 (33%) |
| AA degree | 14 (8%) | 17 (11%) | 17 (10%) |
| BA degree | 21 (13%) | 31 (21%) | 20 (12%) |
| Graduate degree | 8 (5%) | 9 (6%) | 9 (5%) |
| Marital Status | |||
| Married | 16 (10%) | 22 (15%) | 20 (12%) |
| Single | 97 (59%) | 77 (51%) | 100 (58%) |
| Divorced /separated or widowed | 52 (31%) | 51 (34%) | 53 (31%) |
| Current Employment a | |||
| Full-time | 28 (17%) | 36 (24%) | 23 (13%) |
| Part-time | 22 (13%) | 32 (21%) | 31 (18%) |
| Homemaker | 6 (4%) | 6 (4%) | 2 (1%) |
| Student | 15 (9%) | 35 (24%) | 30 (17%) |
| Unemployed | 45 (27%) | 34 (23%) | 61 (35%) |
| Physical Disability | 41 (25%) | 18 (12%) | 25 (15%) |
| Psychiatric Disability | 44 (27%) | 31 (21%) | 37 (21%) |
| Medical or Psychiatric Leave | 1 (1%) | 2 (1%) | 0 (0%) |
| Retired | 4 (2%) | 2 (1%) | 3 (2%) |
| Volunteer | 18 (11%) | 20 (13%) | 15 (9%) |
| Annual household income b | |||
| Less than 20,000 | 111 (67%) | 81 (55%) | 108 (62%) |
| 20 – 49,999 | 41 (25%) | 50 (34%) | 47 (27%) |
| 50 – 64,999 | 5 (3%) | 11 (7%) | 3 (2%) |
| Over 65,000 | 8 (5%) | 6 (4%) | 15 (9%) |
| M SD | M SD | M SD | |
| Age | 41.56 (11.32) | 34.75 (10.95) | 37.56 (12.65) |
| For those born outside the U.S, age moved to the U.S. | 10.81 (7.99) | 14.31 (11.09) | 21.44 (15.50) |
Note. Columns are not mutually exclusive, as many participants reported multi-ethnic backgrounds. The total number of participants recruited to date is 439, not the sum total of each column.
Data presented here is for participants enrolled as of April, 2011. Of note, beginning in July of 2011, we extended our targeted enrollment to all three groups in order to enroll African American and Non-Latino White participants who were younger, employed, and more educated, and Latino participants who were older, unemployed, and less educated.
Categories are not mutually exclusive
Numbers do not add up to group totals due to missing data.
As table 2 reveals, a notable number of our participants report multi-racial/multi-ethnic identities. For the purposes of our study aims 1 and 2, all individuals reporting each ethno-racial identity will be included in the within group analyses of that sample. That is, participants who identify as both African American and Latino will be included in within group analyses of African Americans and in within group analyses of Latinos. For aims 3 and 4, which propose to examine potential between group differences in the influence of various predictors on course, the analytic plan will vary with individual papers and after examination of potential differences between multi-racial participants and single-racial groups.
Overall, the majority of each of the three samples was female and had completed some formal education after high school. Only a small minority of each of the three samples was currently married. Nearly half of the Latino sample was born outside of the U.S. and more than half spoke Spanish in addition to English. The majority of all three samples reported low income, with over half stating that their household annual income was less than $20,000.
3.2. Clinical characteristics
Table 3 details the clinical characteristics of each of the ethno-racial samples. Overall, all three samples met DSM-IV criteria for a large number of Axis I disorders, in excess of the one index disorder required for study eligibility. That is, between 23% and 30% of each sample met criteria for 5 or more Axis I disorders. While the presence of at least one index anxiety disorder was required for study entry, nearly half of participants also met criteria for current Major Depressive Disorder. Data was only available on the ataques de nervios interview for a sub-sample of participants, as this measure was added during the course of study enrollment. Interestingly, all three groups also reported relatively high rates of ataques de nervios. This was particularly true for the Latino and Non-Latino White samples, who endorsed rates of ataques de nervios equal to that of their rates of MDD. Further, the samples evidenced high symptom severity and significant impairment in functioning, as evidenced by low mean GAF scores, ranging from 50 to 53 and by 22% of the sample having made a suicide gesture or attempt. Interestingly, the samples reported a high amount of current and lifetime mental health treatment, with 84 – 92% having a history of psychosocial treatment and 74 to 85% having utilized psychopharmacotherapy.
Table 3.
Clinical Characteristics
| African American N= 165 | Latino N = 150 | Non-Latino White N = 173 | |
|---|---|---|---|
| N % | N % | N % | |
| Diagnoses | |||
| Panic Disorder with Agoraphobia | 77 (47%) | 62 (41%) | 87 (51%) |
| Panic Disorder without Agoraphobia | 10 (6%) | 10 (7%) | 16 (9%) |
| Agoraphobia w/o hx of Panic Disorder | 1 (1%) | 6 (4%) | 5 (3%) |
| GAD | 94 (57%) | 90 (60%) | 105 (61%) |
| Social Phobia | 85 (52%) | 86 (57%) | 92 (53%) |
| PTSD | 67 (41%) | 45 (30%) | 41 (24%) |
| OCD | 41 (25%) | 31 (21%) | 43 (25%) |
| Specific Phobia | 66 (40%) | 59 (39%) | 57 (33%) |
| Major Depressive Disorder | 78 (47%) | 71 (47%) | 72 (42%) |
| Bipolar Disorder | 11 (7%) | 5 (3%) | 11 (6%) |
| Other Mood Disorder | 5 (3%) | 3 (2%) | 9 (5%) |
| Alcohol abuse / dependence | 9 (5%) | 6 (4%) | 13 (8%) |
| Substance abuse / dependence | 6 (4%) | 6 (4%) | 18 (10%) |
| One Axis I disorder | 22 (13%) | 18 (12%) | 23 (13%) |
| Two Axis I disorders | 29 (18%) | 32 (21%) | 35 (20%) |
| 3 disorders | 38 (23%) | 37 (25%) | 40 (23%) |
| 4 disorders | 27 (16%) | 27 (18%) | 35 (20%) |
| 5 or more disorders | 49 (30%) | 36 (24%) | 40 (23%) |
| Ataque de Nerviousa | 25 (25%) | 44 (47%) | 52 (42%) |
| Psychosocial treatment | |||
| Current | 61 (34%) | 74 (49%) | 68 (40%) |
| Life time | 139 (84%) | 137 (91%) | 159 (92%) |
| Psychotropic Medication | |||
| Current | 72 (44%) | 81 (54%) | 105 (61%) |
| Lifetime | 122 (74%) | 117 (78%) | 146 (85%) |
| History of Suicide Gesture or Attempt | 36 (22%) | 33 (22%) | 37 (22%) |
| M SD | M SD | M SD | |
| GAF | 50.27 (7.60) | 51.99 (7.16) | 53.31 (5.43) |
| GSA | 3.87 (0.81) | 3.69 (0.85) | 3.55 (0.88) |
| Number of Axis 1 disorders | 3.48 (1.67) | 3.38 (1.66) | 3.42 (1.73) |
The ataque de nervious measure was added after enrollment for HARP-II began. Thus, for those participants who did not complete it at baseline, data from their first completed form is presented. Ns are as follows: AA = 101; Latino = 94; Non-Latino White = 124.
4. Discussion
All groups evidenced substantial comorbidity of anxiety and other Axis I disorders and meaningfully severe symptoms and functional impairment. The mean number of Axis I disorders was 3.41 and mean GAF scores were in the moderate to severe symptoms and functional impairment range. Further, there was a very high rate (22% of the sample) of self-reported prior suicide attempts or gestures. Interestingly, the rank order of intake anxiety disorder diagnoses is the same for all three ethno-racial groups. That is all three groups evidenced the greatest number of GAD diagnoses, followed by Social Phobia, Panic Disorder with Agoraphobia, and then PTSD. Very few participants from any of the ethno-racial backgrounds, met criteria for Panic Disorder without Agoraphobia or Agoraphobia without history of Panic Disorder. As expected, there was a high rate of comorbid major depressive disorder; rates ranging from 42 – 47%. Interestingly, there was also a very high rate of ataques de nervios, though data collection for this measure on the full sample is still pending.
Examination of our sample characteristics also reveals that the HARP-II Latino sample is diverse with regard to measures of enculturation (e.g., speaking Spanish) and being born in or outside of the U.S. We are pleased as this should provide us with the needed variability to examine the relationship between these factors and the course of anxiety over time.
Interpretation of these findings is limited by the fact that HARP-II is not an epidemiological study, and thus, results do not speak to the relative prevalence of specific anxiety and comorbid disorders or to the demographic characteristics associated with these disorders in the population at large. For example, all three ethno-racial groups in the HARP-II sample reported very low income. We are unable to draw conclusions as to whether this is a meaningful correlate of anxiety disorders (i.e., that individuals in the U.S. who suffer from anxiety have low income) or a consequence of our recruitment methods. Rather, results are here presented to provide a full description of our baseline study sample, on which longitudinal course data will be collected. That is, it will be important for future data from the HARP-II project to be interpreted in the context of this low-income sample.
Surprisingly, especially given the low-income status of our sample, the vast majority of participants had received some type of mental health treatment in the past. Despite the current severity of illness, fewer participants were currently receiving treatment. The design of HARP-II will eventually allow us to examine the adequacy of the treatment received, socio-ethnic predictors of receiving adequate mental health treatment and the relationship between receipt of adequate treatment and course of illness.
5. Conclusion
HARP-II is a prospective, observational, longitudinal study of the course of anxiety disorders in African American, Latino, and Non-Latino White individuals. The original HARP cohort provided valuable information regarding the naturalistic course and predictors of recovery in a primarily White sample. HARP-II will extend this knowledge to two important minority populations in the United States, as well as provide new data on the course of culturally bound syndromes, the relationship between socio-cultural factors and anxiety disorders, and the relationship between anxiety-related traits, ethnicity, and symptom course. The summary from the recent NIMH meeting “Closing the Gaps: The Role of Research in Reducing Mental Health Disparities in the U.S.” (NIMH, 2010) called for further research to “understand the patterning of mental health disparities by disorder”, the need for longitudinal studies on these disparities, and the need to examine the “critical roles of context and SES”. The design of HARP II will allow us to directly address these issues, examining mental health disparities in the longitudinal course of a large number of anxiety and comorbid mental health disorders, in the context of SES and other sociocultural variables that have been identified in the literature as potential risk or protective factors.
Recruitment began in 2004 and will continue until 2012. To date, we have recruited 439 participants. The one-year follow-up assessments will be complete in 2013, and the two-year follow-up assessments will be complete in 2014. We will seek additional funding in order to follow all participants for at least five years. HARP-II will thus create the only prospective, longitudinal examination of the relationship between socio-cultural variables such as perceived discrimination and acculturation and the course of anxiety disorders in African Americans and Latinos. We expect findings from HARP-II to lead to improved understanding of the burden of anxiety disorders and prognostic variables in these populations.
Acknowledgement
HARP-II is funded by the National Institute of Mental Health (5R01MH51415-14). HARP was supported in the past, in part by Upjohn Co, Wyeth-Ayerst Laboratories, Eli Lilly, and NIMH (MH-51415). Since 2008, HARP has been funded solely by NIMH. We thank Ashley Perry for her assistance in preparing the manuscript.
Financial Disclosure In the past 2 years, Dr. Weisberg has received grant funding from Pfizer. Dr. Beard and Ms. Dyck have no financial disclosures. Dr. Keller received grant funding from Pfizer and in the last 2 years received compensation from CENEREX, Medtronic and Sierra Pharmaceuticals.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
To date, the Latino sample in this study has been English-speaking only. In order to have a more representative Latino sample, we have recently undergone translation and validation of our study measures into Spanish, where Spanish speaking versions did not already exist. We are now beginning to recruit and enroll a small number of Spanish-speaking Latinos, as part of our Latino sample.
References
- Adams RE, Boscarino JA. Differences in mental health outcomes among Whites, African Americans, and Hispanics following a community disaster. Psychiatry. 2005;68(3):250–65. doi: 10.1521/psyc.2005.68.3.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal of Public Health. 2007a;97:68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Mulvaney-Day N, Woo M, Torres M, Gao S, Oddo V. Correlates of Past- Year Mental Health Service Use Among Latinos: Results From the National Latino and Asian American Study. American Journal of Public Health. 2007b;97:76–83. doi: 10.2105/AJPH.2006.087197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Vila D, Polo A, Cao Z, Mulvaney-Day N, Torres M, Canino G. Understanding differences in past year psychiatric disorders for Latinos living in the US. Social Science & Medicine. 2007c;65:214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Takeuchi D, Canino G, Duan N, Shrout P, Meng X-L, Vega W, Zane N, Vila D, Woo M, Vera M, Guarnaccia P, Aguilar-Gaxiola S, Sue S, Escobar J, Lin K-M, Gong F. Considering context, place and culture: the National Latino and Asian American Study. International Journal of Methods in Psychiatric Research. 2004;13:208–220. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed., text revision American Psychiatric Association; Arlington: 2000. [Google Scholar]
- Angel R, Guarnaccia PJ. Mind, body, and culture: somatization among Hispanics. Social Science & Medicine. 1989;28(12):1229–38. doi: 10.1016/0277-9536(89)90341-9. [DOI] [PubMed] [Google Scholar]
- Atdjian S, Vega WA. Disparities in mental health treatment in U.S. racial and ethnic minority groups: Implications for psychiatrists. Psychiatric Services. 2005;56:1600–1602. doi: 10.1176/appi.ps.56.12.1600. [DOI] [PubMed] [Google Scholar]
- Baer RD, Weller SC, de Alba Garcia JG, Glazer M, Trotter R, Pachter L, Klein RE. A cross-cultural approach to the study of the folk illness nervios. Cult Med Psychiatry. 2003;27:315–37. doi: 10.1023/a:1025351231862. [DOI] [PubMed] [Google Scholar]
- Bakish D, Hooper CL, Filteau MJ, Charbonneau Y, West DL, Thibaudeau C, Raine D. A double-blind placebocontrolled trial comparing fluvoxamine and imipramine in the treatment of panic disorder with or without agoraphobia. Psychopharmacology Bulletin. 1996;32(1):135–41. [PubMed] [Google Scholar]
- Bayles BP, Katerndahl DA. Culture-bound syndromes in hispanic primary care patients. International Journal of Psychiatry in Medicine. 2009;39:15–31. doi: 10.2190/PM.39.1.b. [DOI] [PubMed] [Google Scholar]
- Bell CC, Shakoor B, Thompson B, Dew D, Hughley E, Mays R, Shorter Gooden K. Prevalence of isolated sleep paralysis in black subjects. Journal of National Medical Association. 1984;76:501–508. [PMC free article] [PubMed] [Google Scholar]
- Borrell LN, Kiefe CI, Williams DR, Diez-Roux AV, Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Social Science and Medicine. 2006;63(6):1415–27. doi: 10.1016/j.socscimed.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Kendler KS, Maxwell S, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2006;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Kendler K, Su M, Aguilar-Gaxiola S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine. 2005;35:317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68(5):748–66. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, Shea MT, Keller MB. Influence of Psychiatric Comorbidity on Recovery and Recurrence in Generalized Anxiety Disorder, Social Phobia, and Panic Disorder: A 12-year Prospective Study. American Journal of Psychiatry. 2005;162:1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambless D, Caputo G, Jasin S, Gracely E, Williams C. The Mobility Inventory for agoraphobia. Behavior Research and Therapy. 1985;23:35–44. doi: 10.1016/0005-7967(85)90140-8. [DOI] [PubMed] [Google Scholar]
- Charlson MEPP, Ales KL, McKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Disease. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Coventry WL, Gillespie NA, Heath AC, Martin NG. Perceived social support in a large community sample: Age and sex differences. Soc Psychiatry Psychiatr Epidemiol. 2004;39:625–636. doi: 10.1007/s00127-004-0795-8. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Swinson RP, Kuch K, Reichman JT. Dimensions of agoraphobia assessed by the Mobility Inventory. Behaviour Research and Therapy. 1993;31(4):427–31. doi: 10.1016/0005-7967(93)90102-z. [DOI] [PubMed] [Google Scholar]
- Craske M, Rachman SJ, Tallman K. Mobility, cognitions, and panic. Journal of Psychopathology and Behavioral Assessment. 1986;8:199–210. [Google Scholar]
- Davidson JR, Beitman B, Greist JH, Maddock RJ, Lewis CP, Sheridan AQ, Carter C, Krishnan KR, Liebowitz MR, Haack DG. Adinazolam sustained-release Treatment of panic disorder: A double-blind study. Journal of Clinical Psychopharmacology. 1994;14(4):255–63. [PubMed] [Google Scholar]
- Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. Exemplification of a method for scaling life events: The PERI Life Event Scale. Journal of Health and Social Behavior. 1978;19:205–229. [PubMed] [Google Scholar]
- Douglass A, Bornstein R, Nino-Murcia G, Keenan S, Miles L, Zarcone VP, Guilleminault C, Dement WC. The Sleep Disorders Questionnaire. I: Creation and multivariate structure of SDQ. Sleep. 17(2):160–167. doi: 10.1093/sleep/17.2.160. [DOI] [PubMed] [Google Scholar]
- Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. Journal of Health and Social Behavior. 2000;41(3):295–313. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/PI, Version 2.0) Biometrics Research Department; New York: 1996. [Google Scholar]
- Fukuda K. One explanatory basis for the discrepancy of reported prevalences of sleep paralysis among healthy respondents. Perceptual and Motor Skills. 1993;77:803–807. doi: 10.2466/pms.1993.77.3.803. [DOI] [PubMed] [Google Scholar]
- Galea S, Vlahov D, Tracy M, Hoover DR, Resnick H, Kilpatrick D. Hispanic ethnicity and post-traumatic stress disorder after a disaster: evidence from a general population survey after September 11, 2001. Annals of Epidemiology. 2004;14(8):520–31. doi: 10.1016/j.annepidem.2004.01.006. [DOI] [PubMed] [Google Scholar]
- Gee GC, Ryan A, Laflamme DJ, Holt J. Self-reported discrimination and mental health status among African descendants, Mexican Americans, and other Latinos in the New Hampshire REACH 2010 Initiative: the added dimension of immigration. American Journal of Public Health. 2006;96(10):1821–8. doi: 10.2105/AJPH.2005.080085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Spencer M, Chen J, Yip T, Takeuchi DT. The association between self-reported racial discrimination and 12-month DSM-IV mental disorders among Asian Americans nationwide. Social Science and Medicine. 2007;64(10):1984–96. doi: 10.1016/j.socscimed.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Goldstein RB, Smith S, Huang B, Saha TD. The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;9(4):363–74. doi: 10.4088/jcp.v67n0305. [DOI] [PubMed] [Google Scholar]
- Guarnaccia PJ, Lewis-Fernadez R, Martinez Pincay I, Shrout P, Guo J, Torres M, Canino G, Alegria M. Ataque de nervios as a marker of social and psychiatric vulnerability: Results from the NLAAS. International Journal of Social Psychiatry. 2010;56:298–309. doi: 10.1177/0020764008101636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guarnaccia PJ, Rubio-Stipec M, Canino G. Ataques de nervios in the Puerto Rican Diagnostic Interview Schedule: the impact of cultural categories on psychiatric epidemiology. Culture, Medicine and Psychiatry. 1989;13(3):275–295. doi: 10.1007/BF00054339. [DOI] [PubMed] [Google Scholar]
- Hays RD, Anderson R, Revicki DA. Psychometric considerations in evaluating health-related quality of life measures. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation. 1993;2(6):441–449. doi: 10.1007/BF00422218. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Horner KJ, Juster HR, Safren SA, Brown EJ, Schneier FR, Liebowitz MR. Psychometric properties of the Liebowitz Social Anxiety Scale. Psychological Medicine. 1999;29:199–212. doi: 10.1017/s0033291798007879. [DOI] [PubMed] [Google Scholar]
- Himle JA, Baser RE, Taylor RJ, Campbell RD, Jackson JS. Anxiety disorders among African Americans, blacks of Caribbean descent, and non-Hispanic whites in the United States. Journal of Anxiety Disorders. 2009;23:578–590. doi: 10.1016/j.janxdis.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang B, Grant BF, Dawson DA, Stinson FS, Chou SP, Saha TD, Goldstein RB, Smith SM, Ruan WJ, Pickering RP. Race-ethnicity and the prevalence and co-occurrence of DSM-IV, alcohol and drug use disorders and Axis I and II disorders: United States 2001 to 2002. Comprehensive Psychiatry. 2006;47:252–257. doi: 10.1016/j.comppsych.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Jackson J, Neighbors H, Torres M, Martin LA, Williams DR, Baser R. Use of Mental Health Services and Subjective Satisfaction With Treatment Among Black Caribbean Immigrants: Results From the National Survey of American Life. American Journal of Public Health. 2007;97(1):60–67. doi: 10.2105/AJPH.2006.088500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, Trierweiler SJ, Williams DR. The National Survey of American life: a study of racial, ethnic, and cultural influences on mental disorders and mental health. International Journal of Methods in Psychiatry Research. 2004;13:196–207. doi: 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller M, Lavori P, Friedman B, Neilson E, Endicott J, McDonald-Scott N, Andreasen N. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–48. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, McDonald-Scott P, Endicott J, Andreasen N, Van Eerdwegh MM. The Reliability of Retrospective Treatment Reports. Psychiatry Research. 1983;9:81–88. doi: 10.1016/0165-1781(83)90092-6. [DOI] [PubMed] [Google Scholar]
- Keller M, Lavori P, Mueller T, Endicott J, Coryell W, Hirschfeld R, Shea T. Time to recovery, chronicity, and levels of psychopathology in major depression: A five-year prospective follow-up of 431 subjects. Archives of General Psychiatry. 1992;49:809–16. doi: 10.1001/archpsyc.1992.01820100053010. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM- III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age of onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R) Intf Methods Psychiatr Research. 2004;13:60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40(3):208–230. [PubMed] [Google Scholar]
- Koenen KC, Stellman JM, Stellman SD, Sommer JF. Risk factors for course of posttraumatic stress disorder among Vietnam veterans: a 14-year follow-up of American Legionnaires. Journal of Consulting and Clinical Psychology. 2003;71:980–986. doi: 10.1037/0022-006X.71.6.980. [DOI] [PubMed] [Google Scholar]
- Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of Discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Social Science and Medicine. 2005;61:1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Lewis-Fernandez R, Guarnaccia PJ, Martinez IE, Salman E, Schmidt A, Liebowitz M. Comparative phenomenology of ataques de nervios, panic attacks, and panic disorder. Culture, Medicine and Psychiatry. 2002;26(2):199–223. doi: 10.1023/a:1016349624867. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems in Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Mellman TA, Aigbogun N, Graves RE, Lawson WB, Alim TN. Sleep paralysis and trauma, psychiatric symptoms and disorders in an adult African American population attending primary medical care. Depression and Anxiety. 2007;0:1–6. doi: 10.1002/da.20311. [DOI] [PubMed] [Google Scholar]
- Myers JK. Yale Greater New Haven Health Survey. Yale University; New Haven: 1980. [Google Scholar]
- Neighbors HW, Caldwell C, Williams DR, Nesse R, Taylor RJ, Bullard KM, Torres M, Jackson JS. Race, ethnicity, and the use of services for mental disorders: results from the National Survey of American Life. Archives of General Psychiatry. 2007;64:485–94. doi: 10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health 2010 http://www.nimh.nih.gov/research-funding/scientific-meetings/2010/closing-the-gaps-the-role-of-research-in-reducing-mental-health-disparities-in-the-us.shtml.
- Norris F, Murrell S. Transitory impact of life-event stress on psychological symptoms in older adults. Journal of Health and Social Behavior. 1987;28:197–211. [PubMed] [Google Scholar]
- Ohayon MM, Shapiro CM. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Compr Psychiatry. 2000;41(6):469–78. doi: 10.1053/comp.2000.16568. [DOI] [PubMed] [Google Scholar]
- Paradis C, Friedman S, Hatch M. Isolated sleep paralysis in African Americans with panic disorder. Cult Diversity Mental Health. 1997;3:69–76. [PubMed] [Google Scholar]
- Peterson RA, Reiss S. Anxiety Sensitivity Index Revised test manual. IDS Publishing Corporation; Worthington, OH: 1993. [Google Scholar]
- Reiss S, Peterson R, Gursky D, McNally R. Anxiety sensitivity, anxiety frequency, and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Resnick HS. Psychometric review of Trauma Assessment for Adults (TAA) In: Stamm BH, editor. Measurement of Stress, Trauma, and Adaptation. Sidran Press; Lutherville, MD: 1996. [Google Scholar]
- Resnick HS, Best CL, Freedy JR. Trauma Assessment for Adults. Medical University of South Carolina, Department of Psychiatry, Crime Victims Research and Treatment Center; Charleston, SC: 1993. [Google Scholar]
- Riolo SA, Nguyen TA, Greden JF, King CA. Prevalence of depression by race/ethnicity: findings from the National Health and Nutrition Examination Survey III. American Journal of Public Health. 2005;95(6):998–1000. doi: 10.2105/AJPH.2004.047225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez B, Pagano M, Keller MB. Factor Structure and Stability of the Anxiety Sensitivity Index in a Longitudinal Study of Anxiety Disorder Patients. Behaviour Research and Therapy. 2004;42:79–91. doi: 10.1016/s0005-7967(03)00074-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy-Byrne PP, Joesch JM, Wang PS. Low socioeconomic status and mental health care use among respondents with anxiety and depression in the NCS-R. Psychiatric Services. 2009;60:1190–1197. doi: 10.1176/ps.2009.60.9.1190. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Russo J, Cowley DS, Katon WJ. Panic disorder in public sector primary care: clinical characteristics and illness severity compared with “mainstream” primary care panic disorder. Depression & Anxiety. 2003;17:51–7. doi: 10.1002/da.10082. [DOI] [PubMed] [Google Scholar]
- Schraufnagel TJ, Wagner AW, Miranda J, Roy-Byrne PP. Treating minority patients with depression and anxiety: what does the evidence tell us? General Hospital Psychiatry. 2006;28:27–36. doi: 10.1016/j.genhosppsych.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Sellers SL, Bonham V, Neighbors HW, Amell JW. Effects of racial discrimination and health behaviors on mental and physical health of middle-class African American men. Health Education and Behavior. 2009;36:31–44. doi: 10.1177/1090198106293526. [DOI] [PubMed] [Google Scholar]
- Sharpless BA, Barber JP. Lifetime prevalence rates of sleep paralysis: A systematic review. Sleep Medicine Reviews. 2011 doi: 10.1016/j.smrv.2011.01.007. doi:10.1016/j.smrv.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpless BA, McCarthy KS, Chambless DL, Milrod BL, Khalsa S-R, Barber JP. Isolated sleep paralysis and fearful isolated sleep paralysis in outpatients with panic attacks. Journal of Clinical Psychology. 2010;66(12):1292–306. doi: 10.1002/jclp.20724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siefer K, Finlayson TL, Williams DR, Delva J, Ismail AI. Modifiable risk and protective factors for depressive symptoms in low-income African American mothers. American Journal of Orthopsychiatry. 2007;77(1):113–23. doi: 10.1037/0002-9432.77.1.113. [DOI] [PubMed] [Google Scholar]
- Smith SM, Stinson FS, Dawson DA, Goldstein R, Huang B, Grant BF. Race/ethnic differences in the prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36(7):987–98. doi: 10.1017/S0033291706007690. [DOI] [PubMed] [Google Scholar]
- Steine IM, Harvey AG, Krystal JH, Milde AM, Grønli J, Bjorvatn B, Nordhus IH, Eid J, Pallesen S. Sleep disturbances in sexual abuse victims: A systematic review. Sleep Medicine Reviews. 2011 doi: 10.1016/j.smrv.2011.01.006. doi:10.1016/j.smrv.2011.01.006. [DOI] [PubMed] [Google Scholar]
- Steketee G, Eisen J, Dyck I, Warshaw M, Rasmussen S. Predictors of course in obsessive-compulsive disorder. Psychiatry Research. 1999;89:229–238. doi: 10.1016/s0165-1781(99)00104-3. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Gil AG. Psychiatric and substance use disorders in South Florida: Racial/ethnic and gender contrasts in a young adult cohort. Arch Gen Psychiatry. 2002;59:43–45. doi: 10.1001/archpsyc.59.1.43. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of the Census Census Bureau. 2004 ONLINE. Available: http://www.census.gov/ipc/www/usinterimproj/
- Vega WA, Karno M, Alegra M, Alvidrez J, Bernal G, Escamilla M, Escobar J, Guarnaccia P, Jenkins J, Kopelowicz A, Lagomasino IT, Lewis-Fernandez R, Marin H, Lopez S, Loue S. Research issues for improving treatment of U.S. Hispanics with persistent mental disorders. Psychiatric Services. 2007;58:395. doi: 10.1176/ps.2007.58.3.385. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term psychiatric study: an ongoing inter-rater reliability monitoring program using the longitudinal interval follow-up evaluation. Journal of Psychiatric Research. 2001;35:297–305. doi: 10.1016/s0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. Journal of Psychiatric Research. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Warshaw M, Massion A, Shea MT, Allsworth J, Keller MB. Predictors of remission in patients with panic with and without agoraphobia: Prospective five-year follow-up data. Journal of Nervous and Mental Disease. 1997;185:517–19. doi: 10.1097/00005053-199708000-00007. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark L, Tellegen A. Development of validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weller SC, Baer RD, de Alba Garcia JC, Rocha ALS. Susto and Nervios: Expressions for Stress and Depression. Cult Med Psychiatry. 2008;32:406–420. doi: 10.1007/s11013-008-9101-7. [DOI] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, Jackson JS. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Archives of General Psychiatry. 2007a;64:305–15. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Williams DR, Haile R, Gonzalez HM, Neighbors H, Baser R, Jackson JS. The Mental Health of Black Caribbean Immigrants: Results from the National Survey of American Life. American Journal of Public Health. 2007b;97:52–59. doi: 10.2105/AJPH.2006.088211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonkers K, Dyck I, Warshaw M, Keller MB. Factors predicting the clinical course of generalized anxiety disorder. The British Journal of Psychiatry. 2000;176:545–550. doi: 10.1192/bjp.176.6.544. [DOI] [PubMed] [Google Scholar]