Abstract
Background
Total auricular reconstruction in congenital lobule type microtia is one of the most challenging problems faced by a reconstructive surgeon as it demands precise surgical technique combined with artistic creativity. Ear reconstruction requires carefully planned procedures.
Methods
We present a simple method for auricular reconstruction consisting of three stages. The first stage is carving the cartilage framework from the costal cartilages of 6th, 7th and 8th ribs, lobule transposition and insertion in a skin pocket. The second stage is performed 5 months later to elevate the ear framework using a full thickness skin graft and a cartilage spare part. The third stage is done after 3–4 months later to give finer detail to the reconstructed ear. This method was used in 27 patients with lobule type microtia.
Results
The results of the reconstructed auricles in 27 patients were satisfactory with good aesthetic balance. The complications ranged from small localized skin infection treated with topical and oral antibiotics to catastrophic loss of the skin pocket and the framework.
Conclusion
Although various donor sites have been used for harvesting the cartilage, only costal cartilage provides a substantial source for fabricating total ear framework. The cosmetic outcome and least complication results in our series support this conclusion.
Keywords: Auricle, Microtia, Costal cartilage
Introduction
The term microtia indicates a small, abnormally shaped or absent external ear. The occurrence of this abnormality is about once in every 6,000–12,000 births [1]. It is the most common major congenital anomaly of the external ear. The affected ear usually has conductive hearing loss (about 40–60 dB) secondary to lack of an external auditory canal and to ossicular fixation [2]. Genetic studies have revealed several possible etiologic factors chromosomal aberrations, multifactorial inheritance and autosomal and recessive traits. The most common syndromes associated with microtia are Goldenhar syndrome, hemifacial microsomia and Treacher–Collins syndrome.
Microtia is classified into grade I: all anatomic subunits present but misshapen, grade II: anatomic subunits either deficient or absent and grade III: classic “peanut ear” and anotia (Fig. 1) [3]. Another classification into lobule-type and concha type is also useful. The lobule type is common among microtic auricular disorders. It is characterized by the presence of a sausage shaped skin remnant of the ear and ear lobule without a concha, acoustic meatus and tragus. The other type of microtia is the concha type which is characterized by ear remnant with a lobule, concha, acoustic meatus, tragus and incisura intertragica. It is thought to be milder than the lobule type.
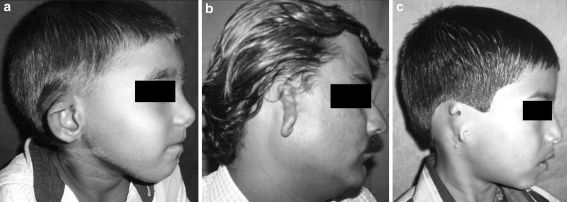
Fig. 1.
a Photograph showing grade I microtia. b Photograph showing grade II microtia. c Photograph showing grade III microtia
Lesser deformities are those of hypoplasia of the middle third or superior of the ear, cupear, lopear, cryptotia and cockle shell ear deformities [4]. The origin of microtia repair had its significant beginnings in 1920, when Gillies buried carved homograft rib cartilage under mastoid skin, then separated it from the head with a cervical flap. Pierce (1930) modified this method by lining the new ear’s posterior surface with a skin graft and building the helix with a flap of rolled up skin. Young (1944) and Peer (1947) turned to autogenous rib cartilage banked in the abdominal skin and used later but with poor results. A major breakthrough came in 1959 when Tanzer rekindled using autogenous rib cartilage, which was carved in a solid block. His excellent results have persisted during the years [5]. Cronin introduced silicone ear framework, but suffered high incidence of extrusion like all inorganic implants [6].
Fukuda stated, in order to achieve all the necessary features for total auricular reconstruction, a one-piece three-dimensional costal cartilage framework consisting of a base frame, a valve like tragus, incisura intertragica, antitragus, antihelix, superior crus, inferior crus and helices were fabricated. Furthermore in order to cover the fabricated frame various flaps and grafts in multiple stages were necessary before finally arriving at the end results.
Recently, interest in the pre-fabrication concept has been rekindled via modern tissue engineering techniques in which bovine cartilage cells are grown in the laboratory and seeded upon a synthetic ear from which is then implanted beneath the skin of a mouse. The early experimental results are interesting, but, it needs a long time of effort and work before it can be applied to humans [7]. In this article, a reliable method of total auricular reconstruction for the severe lobule type microtia is described. The results will be discussed in view of other techniques.
Patients and Methods
Twenty seven patients with a lobule-type microtia were included in this study. All patients had the following characters of lobule-type microtia, absent pinna except for a vertical sausage-shaped skin remnant without a concha, acoustic meatus and tragus [4]. All the patients had a unilateral anomaly seventeen patients were males and ten were females. The ages ranged from 12 to 26 years with an average of 16 years. We did not operate before the age of 10 years so, as to have sufficient growth of the normal contralateral ear and costal cartilage.
Surgical Protocol
Preoperative Planning
The successful grafting of a well-sculpted three-dimensional cartilage framework is the foundation for a sound ear repair. A film pattern from the contralateral normal ear was taken and reversed to plan the new framework then a new pattern 1–2 mm smaller in all dimensions to allow for the extra thickness of covering skin which occurs when the cartilaginous framework is inserted under it. The ear’s location is predetermined in the office by studding the opposite side and making facial measurements that help to achieve symmetry (Fig. 2).
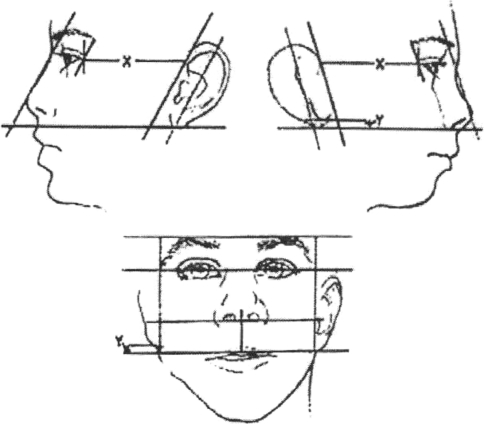
Fig. 2.
Preoperative determination of auricular location. The ear’s slant is positioned to match the opposite side, roughly parallel to the profile of the nose; the distance is matched from the corner of the eye and the microtic lobe’s position is noted (usually displaced upward) when tracing the reverse film pattern, so that the lobe will eventually be positioned correctly when it is transposed into position and “spliced” into the new ear during the second stage of the surgical repair
Surgical Stages
Total external ear reconstruction in the lobule type microtia requires basically three stages. The technique followed in our case was modification of Brents technique (9).
First Stage
Costal cartilage harvesting and framework in Rib cartilage harvesting and framework insertion: We remove the rib cartilages through an oblique incision made just above the lower rib margin from the side opposite the ear being constructed. The cartilaginous portion of the six, seven and eighth rib is harvested according to the previously measured template. The six and seventh rib cartilages form the base framework and the eighth costal cartilage is used to form the rim or helix (Fig. 3).
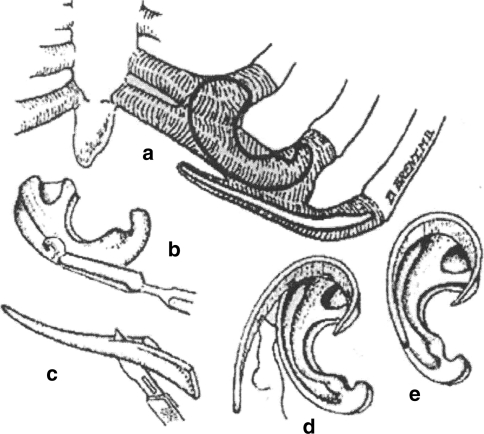
Fig. 3.
a Donor site: chest on side opposite to ear being repaired. The helical rim is obtained from “floating” rib cartilage, the main pattern from a fused block of two cartilages. b Sculpting the main block with chisel. c Thinning the “floating” rib cartilage to produce the helical rim. d Affixing the rim to the main framework with nylon sutures. e Completed framework [14]
Using scalpels and sterilized wood-carving chisels the basic ear framework was carved from the main cartilage block, then the helical rim was carved by thinning of the piece from the floating eighth rib on its outer convex surface to cause deliberate wrapping in a favorable direction, and was sutured to the framework with 6-0 prolene sutures.
Finally, the framework was completed by carving the rest of its details with chisels. The ear position was marked using the film template and preoperatively determined measurements. A small incision was made along the ear vestige dissecting the skin pocket and removing the cartilage remnant beneath the skin. Care is taken not to damage the small blood vessel network that nourishes the skin and to recruit sufficient tension-free skin coverage, the dissection is carried out beyond the marked ear outline.
Following this pocket creation, the three-dimensional framework is inserted in the pocket with a small suction drain beneath and behind the framework. This creates a continuous suction that not only adheres the nourishing skin flap to the carved cartilage, but also prevents possible disastrous blood clots. The convolutions of the new ear were packed with vaseline gauze and a bulky non-compressive dressing was applied. An extra piece of cartilage was carved and stored under the scalp which was later used to obtain the elevation of the created framework in the second stage.
Patients were discharged on the second post operative day on pain medication and antibiotics. The ear dressing was changed after 5 days. The drain stays on the average about 2 days and the sutures were removed on the average after 7 days. The next stage was proceeded approximately 5–6 months later.
Second Stage
After the first stage, the structure has an ear like contour, but still looks two-dimensional. The cartilaginous spare part banked at the first stage is retrieved and placed in a pocket created under the framework by elevation of the mastoid periosteum. The ear framework is lifted from the base and lined with a full thickness skin graft from the groin. The graft is secured in place by sutures and a tie-over dressing followed by ear dressing for 7 days. Depending on patients desire and requirement for further refinement of detail patients were planned for the third stage.
Third Stage
Performed 3–4 months after the second stage surgery. This stage is optional but when performed gives the reconstructed ear a better esthetic and natural look. This stage involves procedures like deepening the concha, revision of post auricular graft contractures, debulking and correction of minor rotational and positional defects of the reconstructed ear. To deepen the concha and revision of post auricular contractures full thickness skin graft from contralateral post auricular region or from the groin where the skin was taken for the second stage surgery is used. This would also help in revising the scar at the previous harvest site.
Results
The results of the reconstructed auricles were satisfactory in regard with the patients and the surgeon. The complications (Table 1) ranged from small localized skin infection treated with topical and oral antibiotics to catastrophic loss of the skin pocket and the framework (Figs. 4, 5).
Table 1.
Summary of complications of auricular reconstruction using autogenous costal cartilage
| Total operated patients | Short 8th rib harvest | Infection | Under/oversized framework | Cartilage resorption/distortion | Pleural tear | Skin necrosis |
|---|---|---|---|---|---|---|
| 27 | 6 | 5 | 3 | 3 | 1 | 1 |
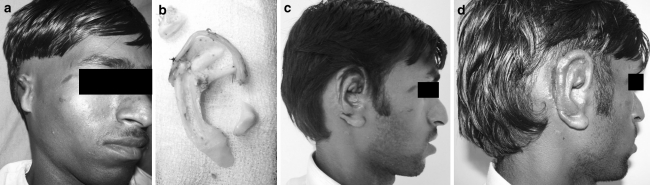
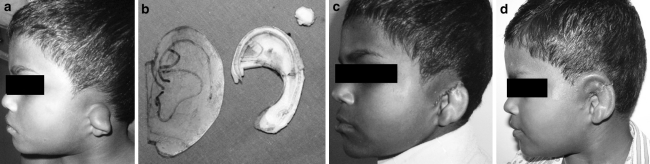
Fig. 4.
a Preoperative photograph of lobule-type microtia. b Three-dimensional costal cartilage framework. c Patient after the first stage with insertion of framework under the skin pocket. d Patient after the second stage with ear elevation and lobule-transposition
Fig. 5.
a Preoperative photograph of lobule-type microtia. b Three-dimensional costal cartilage framework. c Patient after the first stage with insertion of framework under the skin pocket. d Patient after the second stage with ear elevation and lobule-transposition
Discussion
Microtia, especially the lobular-type, represent one of the major craniofacial anomalies requiring total ear reconstruction which is a strenuous task for the surgeon who must have technical knowledge, an accurate analysis of the case and a lot of imagination in order to repair the enormous variety of clinical cases [8]. Total auricular reconstruction is a constant challenge to recreate the complex cutaneous and cartilaginous structure that no one could create to such perfection.
Microtia has an enormous emotional impact on patient and family members; especially on parents psychological support and care are of great value in the whole treatment. Surgeons cannot neglect the serious emotional distress caused by the birth of an imperfect child. For the parents it is great frustration to see their child born with such a serious physical problem. But, the surgeon should establish the adequate date for the surgery not influenced by family members who want immediate solution. The ideal time for reconstruction of the ear is after the child is 7 years old when the physical development of the ear has already reached a certain size and it will not cause a severe distortion between the reconstructed ear and the normal one. Another important factor to obtain good surgical detail is the thickness of the costal cartilage that we use to sculpture the new framework. Before the age of seven this structure is still very fragile and thin, without adequate conditions for the creation of the new auricular framework once this is explained to the parents their anxiety will diminish, thus contributing to the success of the surgery [9].
The final decision on the timing the repair should depend on the physical development and the girth of the lower chest so as to obtain an ideal costal cartilage complex.
For acquiring the ideal form and size of the earlobe by reconstruction, the technique used should satisfy some factors as follows:
Sufficient soft tissue is easily available.
The symmetrical balance is satisfactory.
The smooth margin and thin form are maintained.
The technique is simple and safe.
The color and texture can be well matched compared with surrounding tissues.
Many techniques are available for reconstruction of the ear in lobule-type microtia, each has advantages and disadvantages [10]. Basically, we need at least two components in total auricular reconstruction: The first is a framework matching the shape and contour of the ear and second is a soft tissue cover which must be thin and adequate. In cases of lobule type microtia the framework should be large enough to give the adequate ear volume; so, conchal graft from the opposite auricle is not enough. The use of homologous cartilage was tried [11] but always absorbs and failed. The use of alloplastic frameworks was attractive at the beginning and several materials were used as silicon rubber and polyethylene [7]. The use of porous polyethylene framework was widely used at a time with two stage procedure. The first stage involves rotating a superficial temporoparietal flap over the framework with skin graft and pocket. The second stage was a lobule transposition and ear elevation. This technique was thought to be less invasive and reliable method of total ear reconstruction in comparison to many other techniques. But, in the last few years many authors [3, 4, 12] reported high incidence of extrusion of all these alloplastic frames, regardless the material used inspite of the attempts to minimize this problem by covering the framework with extra tissue grafts and flaps.
The other obvious limitation of these alloplastic frames is the difficulty of a accommodating the great variation in size and shape that must be produced to match the opposite normal ear. When sculpting directly from rib cartilage these limitations do not exist because the surgeon creates the required specific size and shape each time. So, we discontinued using all these alloplastic frames in favor of costal cartilage frames. Serious attempts at tissue engineering began in the early 1980s. Cartilage, being avascular with modest nutritional requirement, was an ideal medium to begin work in this arena. This quickly lead to applications in microtia repair [13]. Bioabsorbable artificial polymers served as matrices for chondrocytes. Early results with culturing polyglycolytic/polylactic acid polymers with bovine chondrocytes demonstrated that lasting three dimensional structures were feasible. Chondrocytes multiplied and the biodegradable polymer was to some extent replaced by matrix, however, polymer replacement inevitably led to loss of prosthesis shape with time.
Ongoing work with human chondrocytes and biodegradable matrices continues and 1 day might represent the standard of care in microtia repair. Maintenance of cartilage integrity with time and thus preserving a precise and delicate auricular architecture remains the most significant hurdle to overcome before this technology is clinically feasible. To this data, when tissue engineering can provide the ideal cartilage frames, sculpted autogenous rib cartilage remains the material of choice for surgical repair of lobule-type microtia.
Although various donor sites have been used for harvesting the cartilage, only costal cartilage provides a substantial source for fabricating total ear framework. Many authors support this concept as Osomo [8] and Nagata [4]. So, we continue refining and evolving the use of costal cartilage frameworks. The cosmetic outcome and least complication results in our series support this conclusion. As regard the soft tissue cover of the frame work we found the use of a skin pocket carefully dissected without a temporoparietal facial flap is very useful in the first stage reconstruction, the facial flaps with a skin graft over it is risky and the aesthetic results are much less as it masks the contour and details of the framework. Also, in the second stage we elevate the ear with a skin graft only and appear to be satisfactory without a supporting block of cartilage. It was found that it was useful to perform ear lobule transposition in the second stage not at separate stage. Ear reconstruction from autogenous tissues withstand trauma remarkably well [5]. This observation is always found in all of the present cases.
In conclusion, analysis of the patients operated using the described technique, it became evident that the procedure using costal cartilage graft under a skin pocket followed by ear elevation with a skin graft only after 3 months, has demonstrated to be very reliable technique in cases of lobule-type microtia.
Acknowledgments
Conflict of Interest
None declared.
References
- 1.Naki H. Reconstruction of microtia with a contour accentuated framework and supplemental coverage. Plast Reconstr Surg. 1986;78:604. doi: 10.1097/00006534-198611000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Brent B (1980) The correction of microtia with autogenous rib cartilage grafts: II. Atypical and complex deformities. Plast Reconstr Surg 66:13 [DOI] [PubMed]
- 3.Brent B. Auricular repair with autogenous rib cartilage grafts: two decades of experience with 600 cases. Plast Reconstr Surg. 1992;90:355. doi: 10.1097/00006534-199209000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Nagata S. Modification of the stages in total reconstruction of the auricle: Part 1 grafting the three dimensional costal cartilage framework for lobule type microtia. Plast Reconstr Surg. 1994;93(2):221. doi: 10.1097/00006534-199402000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Brent B. Microtia repair with rib cartilage grafts: a review of personal experience with 1000 cases. Clin Plast Surg. 2002;29:257. doi: 10.1016/S0094-1298(01)00013-X. [DOI] [PubMed] [Google Scholar]
- 6.Shanbhag A, Friedman MI, Augustine J, Recum AF. Evaluation of porous polyethylene for external ear reconstruction. Ann Plast Surg. 1990;24:32. doi: 10.1097/00000637-199001000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Cao Y, Vacanti JP, Paige KT. Transplantation of chondrocytes utilizing polymer-cell construct to produce tissue-engineered cartilage in the shape of human ear. Plast Reconstr Surg. 1997;100:297. doi: 10.1097/00006534-199708000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Osomo G. Autogenous rib cartilage reconstruction of congenital ear defects: report of 110 cases with Brent’s technique. Plast Reconstr Surg. 1999;104:1951. doi: 10.1097/00006534-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Brent B. The pediatrician’s role in caring for patients with congenital microtia and atresia. Pediatr Ann. 1999;28:374. doi: 10.3928/0090-4481-19990601-09. [DOI] [PubMed] [Google Scholar]
- 10.Yotsuyanag T, Yamashital K, Sawada Y. Reconstruction of congenital and acquired earlobe deformity. Clin Plast Surg. 2000;29:249. doi: 10.1016/S0094-1298(01)00010-4. [DOI] [PubMed] [Google Scholar]
- 11.Steffenson WH. Comments on reconstruction of external ear. Plast Reconstr Surg. 1955;16:194. doi: 10.1097/00006534-195509000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Brent B. Technical advances in ear reconstruction with autogenous rib cartilage graft. Personal experience with 1200 cases. Plast Reconstr Surg. 1999;104:319. doi: 10.1097/00006534-199908000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Saadeh PB, Brent B, Longacre M. Human cartilage engineering: chondrocyte extraction, proliferation and characterization for construct development. Ann Plast Surg. 1999;42:509. doi: 10.1097/00000637-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Brent B. Total auricular construction with sculpted costal cartilage. In: Brent B, editor. The artistry of reconstructive Surgery. St. Louis: The C.V. Mosby Co.; 1987. [Google Scholar]