Abstract
Latinos have higher rates of diabetes and diabetes-related complications compared to non-Latinos. Clinical diabetes self-management tools that rely on innovative health information technology (HIT) may not be widely used by Latinos, particularly those that have low literacy or numeracy, low income, and/or limited English proficiency. Prior work has shown that tailored diabetes self-management educational interventions are feasible and effective in improving diabetes knowledge and physiological measures among Latinos, especially those interventions that utilize tailored coaching and navigator programs. In this article, we discuss the role of HIT for diabetes management in Latinos and describe a novel “eNavigator” role that we are developing to increase HIT adoption and thereby reduce health care disparities.
Keywords: cell phone text messaging, diabetes self-management, digital divide, Latino health care disparities, patient navigation
Introduction
The incidence of type 2 diabetes (T2DM) and its long term sequelae are increasing in the United States (U.S.), particularly among Latinos,1–6 who are now the largest ethnic minority, comprising 16% of the U.S. population.7 Efforts to redesign care through the use of innovative HIT must address cultural and language barriers faced by this growing population. In this report, we discuss challenges and potential benefits of tailoring HIT interventions to Latino patients with T2DM.
How Can We Help Patients to Reduce Diabetes-Related Complications?
Diabetes-related macro- and microvascular complications are preventable through normalization of blood glucose, blood pressure, and lipid levels.8 Improved glucose control can be achieved through intensive diabetes self-management (DSM) education,9 which has been shown to improve both the self-management practices and the confidence of patients in their ability to complete these activities, leading to improved outcomes.10–13
Diabetes self-management requires close teamwork between patients and their health care providers (HCPs), raising particular challenges for Latinos with limited English proficiency (LEP) who do not have culturally and linguistically concordant HCPs. This situation is not likely to improve anytime soon, since recent national medical student and physician surveys consistently show disproportionately low numbers of Latino health care providers compared with the corresponding proportion of the national population of Latinos.14–15 Studies have shown that DSM support occurs inconsistently during medical visits and that patient communication and understanding is suboptimal, especially among LEP Latinos.16–17 Latinos perform daily self-monitoring of blood glucose less frequently than Caucasians, especially low-income LEP Latinos.18 These populations have additional impediments, such as low health literacy and numeracy, lack of trust in HCPs, and poor social support.19–22 However, a survey of patients with diabetes in safety-net settings reported both an interest in receiving self-management support and the belief that their diabetes would be better controlled if they communicated better with their HCP.23 In addition, culturally appropriate and culturally relevant Spanish-language cognitive-behavioral DSM educational interventions have shown feasibility, acceptability, and efficacy in improving diabetes knowledge and physiological measures.24–25 Thus, systems designed to improve DSM among Latinos have the potential to substantially improve health care outcomes.
How Do We Fully Engage Latinos with Multiple Barriers to Care in Diabetes Self-Management?
Unfortunately, there are precious little data to guide health system redesign for different patient populations. Latinos who are LEP, low literate or illiterate, low income, or those with multiple chronic comorbidities may be the most difficult to reach or the least likely to participate or remain in clinical trials.26–27 Few large, randomized trials of DSM interventions have specifically targeted Latinos.28–30 Interventions that link self-monitoring of blood glucose to educational or behavioral advice and changes in clinical management have been most successful,31 and research has shown that minority patients do much better in connecting multiple components of high-quality care and self-management when they have culturally and linguistically sensitive support, such as culturally tailored coaching and navigator programs.32–34
Since 2005, culturally tailored patient navigator programs have been developed and implemented to support T2DM care (including self-management). Patient navigators are generally defined as bilingual members of the clinical care team from the patient community who are familiar with social and cultural nuances of the patients they serve and who work to connect patients to clinicians to prevent or manage disease.35–37 This role differs from that of health coaches, who are more likely to use motivational interviewing and other techniques to help change patient behavior. Navigators work to identify individuals most at risk for suboptimal care and to mitigate barriers to the receipt of that care. Navigation programs are oriented towards flexible problem solving rather than providing a predefined set of services.
Guided both by principles of disease management and by cultural sensitivity, successful navigator disparity reduction interventions tend to apply culturally tailored
and intensive interpersonal skills and social networks (such as interactive or one-on-one education and community health workers).38–39 Patient navigators can provide a broader range of services and strategies to patients than health coaches. For example, patient navigators can coordinate access to a comprehensive continuum of clinical and nonclinical services by facilitating communication and cooperation between providers and by providing tailored patient education and support necessary to increase a patient's ability to comply with prescribed therapies. Culturally tailored interventions have been shown to be much more effective in patient activation among LEP minorities compared to generalized T2DM self-management training interventions.40 Studies have shown that minorities benefit more from one-on-one interventions tailored to their literacy, circumstances, and needs.41 Although navigator programs tend to succeed in reducing disparities for individual patients, the time and cost intensity of this approach poses a barrier to wider implementation of tailored navigator programs.
What is the Role of Health Information Technology in Engaging Latino Patients in Diabetes Care?
Information technology (IT) tools are increasingly used for T2DM management with improved short- and long-term process measures and outcomes.42–45 Information technology tools that engage both patients and HCPs have had the greatest impact on improving care.46–47 Most patient users of innovative HIT tools have been better-educated and better-controlled “early adopters.”48 Longstanding financial, social, and language disparities have resulted in a “digital divide,” in which technology and Internet utilization patterns differ by race/ethnicity and socioeconomic lines.49–51 However, this digital divide is beginning to narrow for Latinos. For example, from 2006 to 2008, Internet use among Latino adults rose from 54–64% (African American adults = 63% and Caucasian adults = 76%).52 Over 3/4 (77%) of U.S.-born Latinos used the Internet, as compared with 52% of the foreign-born. Indeed, 83% of U.S.-born Latino home Internet users had a broadband connection in 2008, while the rate was 68% among the foreign-born. These data indicate that most Latino patients will have the hardware necessary to engage in IT-based interventions.
In addition, the digital divide does not preclude use of HIT tools to support T2DM care. A survey of T2DM patients who were not using the Internet demonstrated that, although race and education were significant predictors of receptivity to technology adoption, interest in technology that facilitated information-sharing with their physicians was high in all groups.53 National survey data demonstrate that patients with chronic diseases report lower rates of technology access overall, but those with chronic disease who do attain access are more likely to seek out health information online54 compared with those without a chronic condition. Patients with chronic disease who attain technology access are also more likely to use an electronic patient portal, even among patients at Federally Qualified Health Centers.55 These findings suggest that the digital divide may not apply to the use of IT tools for chronic disease management. The challenge remains how to engage these patients and support their use of HIT-based T2DM management tools.
How Do We Harness Information Technology-Based Type 2 Diabetes Management Tools to Eliminate Diabetes Disparities Among Latinos?
We know that HIT-based T2DM management tools are generally successful. Several meta-analyses have demonstrated that physician-directed, visit-based clinical reminders have only a modest impact on care processes and generally little to no effect on clinical outcomes.56–57 In contrast, evidence-based IT interventions that include patients in their diabetes care have a beneficial impact on health care costs and clinical outcomes.58–59 Previous reviews of telemedicine in T2DM management have shown significant reductions in hemoglobin A1c (HbA1c) and complications, good receptiveness by patients, and patient empowerment and education.60–61 Interventions that link self-monitoring of blood glucose to educational or behavioral advice and changes in clinical management have been most successful.62 However, the patients in these studies have been overwhelmingly Caucasian and generally from higher socioeconomic backgrounds.
It is not yet known how to fully engage Latinos with computer-based disease management. Most Internet DSM programs are largely informational, at high literacy levels, and available only in English.63 A few studies suggest that Latinos can be successfully engaged via bi-directional (i.e., allowing for significant provider and patient communication) IT management tools. A large, randomized, controlled trial involving older, ethnically diverse diabetes patients residing in federally designated, medically underserved areas of New York state implemented synchronous videoconferencing (‘home televisits,’ which also included uploading of self-monitoring data and access to support information) of diabetes case management with diabetes educators compared with usual care. Trial results demonstrated lasting glycemic, blood pressure, and cholesterol improvements after 5 years of follow up.64 These findings were particularly strong for Hispanics (3/4 spoke primarily Spanish) with the highest baseline HbA1c levels, who also had the lowest income, educational attainment, and computer experience. However, it was also determined that there were high implementation costs, largely representing special purpose hardware and software costs, which present a significant barrier to widespread use of this intensive telemedicine approach.65 This study emphasizes that telemedicine case management can be sustained over time even among vulnerable or ‘hard-to-reach’ populations. In addition, lower cost telemonitoring should be included in all DSM programs, as these methods have been shown effective. Importantly, successful DSM trials point to the importance of sustained and continued contact with patients in order to maximize success.
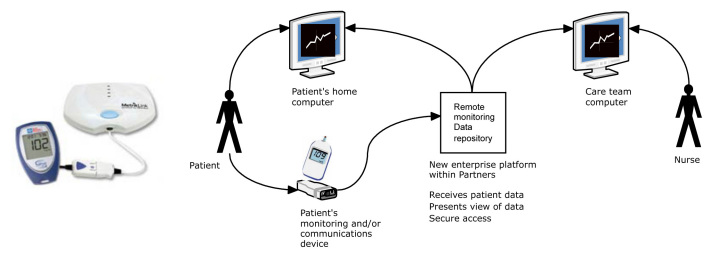
The Massachusetts General Hospital (Boston, MA) adult primary care network includes 181 primary care physicians working in 13 clinically and demographically diverse practices (4 community health centers and 9 hospital-affiliated practices). The practices use the same electronic billing and scheduling systems, and physicians have the same compensation plan and staffing resources. In our primary care network, we have developed and implemented a Web-based home glucose monitoring tool [the Diabetes Connect System (DCS)].53 The remote blood glucose monitoring application was designed within an easy-to-use Web site for both patients and their clinicians. Wireless linking technology allows patients to upload glucometer readings from commercially available glucometers to a secure Web site (Figure 1).
Figure 1.
The Diabetes Connect System utilizes wireless linking technology for uploading glucometer data to a secure Web site.
Patients and clinicians have separate Web site interfaces. Glucose data are presented in a context rich Web site intended to help the patient with self management strategies (Figure 2). Clinicians have access to a “population management” view (a stand alone Web site outside of the clinical electronic medical record systems) that lists each participating patient and corresponding key data on a single line. Clicking on a specific patient name allows a “drill-down” view of additional data for that patient. Clinicians can also set individualized parameters triggering alerts for specific patients and can initiate email-messaging interactions with participating patients. The Web tool provides a graphical representation of glucose trends with patient and clinician views. A 3-month pilot study of this technology among non-minority patients demonstrated that it was well received; participants valued the support as highly as face-to-face encounters, and mean blood glucose range and HbA1c improved.66 Eight practices within the Massachusetts General Hospital primary care network use the DCS.
Figure 2.
An example of data provided by the Diabetes Connect System Web interface.
We are in the process of adapting the DCS to the needs of LEP Latino patients by integrating a novel, culturally tailored navigator program (eNavigator) with a modified version of the DCS patient/provider interface. While still in development, this novel eNavigator interface will include an area for documenting patient-specific barriers, corresponding strategies used to overcome these barriers, and an area to support clear lines of communication between HCPs, eNavigators, and patients. This new “eNavigator” role will address the digital divide that separates many Latinos from technologically advanced care. We hypothesize that integrating the person-to-person navigator model with a language- and culturally-adapted HIT diabetes management tool will lead to improved patient–provider communication, improved patient diabetes knowledge and self-management skills, and improved glycemic control for our least technologically-savvy Latino T2DM patients. There have been no published studies of navigators using HIT tools to improve Latino diabetes care.
The Chronic Illness Care Model emphasizes patient-oriented care and the activation of patients.67,68 Emerging evidence suggests that focused interventions can increase patient activation, and that increased patient activation is associated with a reduction in racial and ethnic disparities.69,70 The eNavigator proposed in this project will be specifically designed to (1) activate LEP Latino patients in their DSM, (2) increase the patient's DSM between clinical visits by increasing the amount of time and engagement with information and personally tailored care plans, and (3) help integrate the patient, navigator, and the physician into a more effective team. The eNavigator has the potential to fundamentally change the way T2DM care is delivered to Latinos. Development of an innovative and effective computerized linguistic- and culturally tailored eNavigator would allow for the expansion of a successful disparity-reduction intervention in a cost-effective fashion.
What Are the Most Effective Modes of Health Information Technology Messaging?
As HIT tools are developed and tested in clinical populations, it is becoming clear that Web-based tools may have limited reach. The e-Navigation model can be extended to cell phone text messaging as the IT platforms continue to become more sophisticated. Wireless mobile technologies, such as cell phones and text messaging, have been shown in numerous small trials to have a beneficial impact on the management of chronic diseases, such as diabetes, asthma, and hypertension, as well as in health improvement activities, such as smoking cessation treatment—all which require ongoing advice and support.71 Text messaging has also been shown to decrease the number of missed appointments and increase the amount of communication between providers and patients between visits.72–73 Compared with computer technology, ownership and use of cell phones among persons of low socioeconomic status is as common as among those of the general population.74 This high prevalence of cell phone use increases the likelihood of successfully implementing health interventions for traditionally hard-to-reach populations by using text messaging technology. In addition, cell phone methods may be more cost-effective.
Summary
We are currently at an important turning point in health care—one in which HIT will move from a luxury to a necessity. We can harness HIT's potential to achieve equality in health care delivery for all. Interventions for DSM must incorporate theory-based principles and provide tailored feedback and information with the possibility of intensive personalized communication between clinical HCPs and patients. There is a national priority for eliminating health care disparities through targeted and tailored translational research focused on priority populations. Some studies have suggested that Latinos are a “hard-to-reach” population for clinical trials or intensive chronic illness management. The combination of the belief that Latinos are hard to reach and that a digital divide exists has led to the erroneous exclusion of Latinos from important clinical research and intensive DSM. Major advances in the care of this population may be possible if we can effectively adapt emerging HIT tools to the needs and patterns of the Latino community.
Glossary
Abbreviations
- (DCS)
Diabetes Connect System
- (DSM)
diabetes self-management
- (HCP)
health care provider
- (HIT)
health information technology
- (HbA1c)
hemoglobin A1c
- (IT)
information technology
- (LEP)
limited English proficiency
- (T2DM)
type 2 diabetes mellitus
- (U.S.)
United States
References
- 1.Gregg EW, Cadwell BL, Cheng YJ, Cowie CC, Williams DE, Geiss L, Engelgau MM, Vinicor F. Trends in the prevalence and ratio of diagnosed to undiagnosed diabetes according to obesity levels in the U.S. Diabetes Care. 2004;27(12):2806–2812. doi: 10.2337/diacare.27.12.2806. [DOI] [PubMed] [Google Scholar]
- 2.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Ann Intern Med. 2009;150(8):505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 3.Cowie CC, Rust KF, Ford ES, Eberhardt MS, Byrd-Holt DD, Li C, Williams DE, Gregg EW, Bainbridge KE, Saydah SH, Geiss LS. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care. 2009;32(2):287–294. doi: 10.2337/dc08-1296. Epub 2008 Nov 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cowie CC, Rust KF, Byrd-Holt DD, Gregg EW, Ford ES, Geiss LS, Bainbridge KE, Fradkin JE. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care. 2010;33(3):562–568. doi: 10.2337/dc09-1524. Epub 2010 Jan 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Emanuele N, Sacks J, Klein R, Reda D, Anderson R, Duckworth W, Abraira C Veterans Affairs Diabetes Trial Group. Ethnicity, race, and baseline retinopathy correlates in the veterans affairs diabetes trial. Diabetes Care. 2005;28(8):1954–1958. doi: 10.2337/diacare.28.8.1954. [DOI] [PubMed] [Google Scholar]
- 6.Lanting LC, Joung IM, Mackenbach JP, Lamberts SW, Bootsma AH. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: a review. Diabetes Care. 2005;28(9):2280–2288. doi: 10.2337/diacare.28.9.2280. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Census Bureau. Hispanic or Latino by Type: 2010. 2010 Census Summary File 1. http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_SF1_QTP10&prodType=table. Accessed on December 15, 2011.
- 8.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 9.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352(9131):837–853. [PubMed] [Google Scholar]
- 10.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24(3):561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 11.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21(10):1644–1651. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 12.Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. How well do patients' assessments of their diabetes self-management correlate with actual glycemic control and receipt of recommended diabetes services? Diabetes Care. 2003;26(3):738–743. doi: 10.2337/diacare.26.3.738. [DOI] [PubMed] [Google Scholar]
- 13.Holman H, Loring K. Patient self-management: a key to effective-ness and efficiency in care of chronic disease. Public Health Rep. 2004;119(3):239–243. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brotherton SE, Etzel SI. Graduate medical education, 2010-2011. JAMA. 2011;306(9):1015–1030. doi: 10.1001/jama.2011.1236. [DOI] [PubMed] [Google Scholar]
- 15.American Medical Association. Minority Affairs Section. Physician Statistics. http://www.ama-assn.org/ama/pub/about-ama/our-people/member-groups-sections/minority-affairs-consortium/physician-statistics/total-physicians-raceethnicity.page.
- 16.Schillinger D, Bindman A, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ Couns. 2004;52(3):315–323. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 17.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17(4):243–252. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levine DA, Allison JJ, Cherrington A, Richman J, Scarinci IC, Houston TK. Disparities in self-monitoring of blood glucose among low-income ethnic minority populations with diabetes, United States. Ethn Dis. 2009;19(2):97–103. [PubMed] [Google Scholar]
- 19.Heisler M, Faul JD, Hayward RA, Langa KM, Blaum C, Weir D. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the health and retirement study. Arch Intern Med. 2007;167(17):1853–1860. doi: 10.1001/archinte.167.17.1853. [DOI] [PubMed] [Google Scholar]
- 20.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, Ford DE. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 21.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 22.Karter AJ, Ferrara A, Darbinian JA, Ackerson LM, Selby JV. Self-monitoring of blood glucose: language and financial barriers in a managed care population with diabetes. Diabetes Care. 2000;23(4):477–483. doi: 10.2337/diacare.23.4.477. [DOI] [PubMed] [Google Scholar]
- 23.Sarkar U, Piette JD, Gonzales R, Lessler D, Chew LD, Reilly B, Johnson J, Brunt M, Huang J, Regenstein M, Schillinger D. Preferences for self-management support: findings from a survey of diabetes patients in safety-net health systems. Patient Educ Couns. 2008;70(1):102–110. doi: 10.1016/j.pec.2007.09.008. Epub 2007 Nov 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: a pilot study. Ann Behav Med. 2005;29(3):225–235. doi: 10.1207/s15324796abm2903_9. [DOI] [PubMed] [Google Scholar]
- 25.Mauldon M, Melkus GD, Cagganello M. Tomando Control: a culturally appropriate diabetes education program for Spanish-speaking individuals with type 2 diabetes mellitus–evaluation of a pilot project. Diabetes Educ. 2006;32(5):751–760. doi: 10.1177/0145721706291999. [DOI] [PubMed] [Google Scholar]
- 26.Baquet CR, Commiskey P, Daniel Mullins C, Mishra SI. Recruit-ment and participation in clinical trials: socio-demographic, rural/urban, and health care access predictors. Cancer Detect Prev. 2006;30(1):24–33. doi: 10.1016/j.cdp.2005.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosal MC, White MJ, Borg A, Scavron J, Candib L, Ockene I, Magner R. Translational research at community health centers: challenges and successes in recruiting and retaining low-income Latino patients with type 2 diabetes into a randomized clinical trial. Diabetes Educ. 2010;36(5):733–749. doi: 10.1177/0145721710380146. Epub 2010 Aug 20. [DOI] [PubMed] [Google Scholar]
- 28.Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the Starr County border health initiative. Diabetes Care. 2002;25(2):259–268. doi: 10.2337/diacare.25.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lorig K, Ritter PL, Villa F, Piette JD. Spanish diabetes self-management with and without automated telephone reinforcement: two randomized trials. Diabetes Care. 2008;31(3):408–414. doi: 10.2337/dc07-1313. [DOI] [PubMed] [Google Scholar]
- 30.Rosal MC, Ockene IS, Restrepo A, White MJ, Borg A, Olendzki B, Scavron J, Candib L, Welch G, Reed G. Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income latinos: latinos en control. Diabetes Care. 2011;34(4):838–844. doi: 10.2337/dc10-1981. Epub 2011 Mar 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Farmer A, Gibson OJ, Tarassenko L, Neil A. A systematic review of telemedicine interventions to support blood glucose self-monitoring in diabetes. Diabet Med. 2005;22(10):1372–1378. doi: 10.1111/j.1464-5491.2005.01627.x. [DOI] [PubMed] [Google Scholar]
- 32.Gary TL, Batts-Turner M, Yeh HC, Hill-Briggs F, Bone LR, Wang NY, Levine DM, Powe NR, Saudek CD, Hill MN, McGuire M, Brancati FL. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2009;169(19):1788–1794. doi: 10.1001/archinternmed.2009.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Percac-Lima S, Grant RW, Green AR, Ashburner JM, Gamba G, Oo S, Richter JM, Atlas SJ. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009;24(2):211–217. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sisk JE, Hebert PL, Horowitz CR, McLaughlin MA, Wang JJ, Chassin MR. Effects of nurse management on the quality of heart failure care in minority communities: a randomized trial. Ann Intern Med. 2006;145(4):273–283. doi: 10.7326/0003-4819-145-4-200608150-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dohan D, Schrag D. Using navigators to improve care of underserved patients: current practices and approaches. Cancer. 2005;104(4):848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 36.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am J Prev Med. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 37.Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, Mandelblatt JS, Paskett ED, Raich PC Patient Navigation Research Program. Patient navigation: state of the art or is it science? Cancer. 2008;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heisler M, Spencer M, Forman J, Robinson C, Shultz C, Palmisano G, Graddy-Dansby G, Kieffer E. Participants' assessments of the effects of a community health worker intervention on their diabetes self-management and interactions with healthcare providers. Am J Prev Med. 2009;37(6 Suppl 1):S270–S279. doi: 10.1016/j.amepre.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corkery E, Palmer C, Foley ME, Schechter CB, Frisher L, Roman SH. Effect of a bicultural community health worker on completion of diabetes education in a Hispanic population. Diabetes Care. 1997;20(3):254–257. doi: 10.2337/diacare.20.3.254. [DOI] [PubMed] [Google Scholar]
- 40.Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64(5 Suppl):101S–156S. doi: 10.1177/1077558707305409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Glazier RH, Bajcar J, Kennie NR, Willson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care. 2006;29(7):1675–1688. doi: 10.2337/dc05-1942. [DOI] [PubMed] [Google Scholar]
- 42.Cho JH, Chang SA, Kwon HS, Choi YH, Ko SH, Moon SD, Yoo SJ, Song KH, Son HS, Kim HS, Lee WC, Cha BY, Son HY, Yoon KH. Long-term effect of the Internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with a ubiquitous medical care system. Diabetes Care. 2006;29(12):2625–2631. doi: 10.2337/dc05-2371. [DOI] [PubMed] [Google Scholar]
- 43.Azar M, Gabbay R. Web-based management of diabetes through glucose uploads: has the time come for telemedicine? Diabetes Res Clin Pract. 2009;83(1):9–17. doi: 10.1016/j.diabres.2008.09.055. [DOI] [PubMed] [Google Scholar]
- 44.Kwon HS, Cho JH, Kim HS, Song BR, Ko SH, Lee JM, Kim SR, Chang SA, Kim HS, Cha BY, Lee KW, Son HY, Lee JH, Lee WC, Yoon KH. Establishment of blood glucose monitoring system using the internet. Diabetes Care. 2004;27(2):478–483. doi: 10.2337/diacare.27.2.478. [DOI] [PubMed] [Google Scholar]
- 45.Costa BM, Fitzgerald KJ, Jones KM, Dunning Am T. Effectiveness of IT-based diabetes management interventions: a review of the literature. BMC Fam Pract. 2009;10:72. doi: 10.1186/1471-2296-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Holbrook A, Thabane L, Keshavjee K, Dolovich L, Bernstein B, Chan D, Troyan S, Foster G, Gerstein H COMPETE II Investigators. Individualized electronic decision support and reminders to improve diabetes care in the community: COMPETE II randomized trial. CMAJ. 2009;181(1–2):37–44. doi: 10.1503/cmaj.081272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Grant RW, Middleton B. Improving primary care for patients with complex chronic diseases: can health information technology play a role? CMAJ. 2009;181(1–2):17–18. doi: 10.1503/cmaj.091101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grant RW, Wald JS, Schnipper JL, Gandhi TK, Poon EG, Orav EJ, Williams DH, Volk LA, Middleton B. Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2008;168(16):1776–1782. doi: 10.1001/archinte.168.16.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brodie M, Flournoy RE, Altman DE, Blendon RJ, Benson JM, Rosenbaum MD. Health information, the Internet, and the digital divide. Health Aff (Millwood). 2000;19(6):255–265. doi: 10.1377/hlthaff.19.6.255. [DOI] [PubMed] [Google Scholar]
- 50.Wagner TH, Bundorf MK, Singer SJ, Baker LC. Free internet access, the digital divide, and health information. Med Care. 2005;43(4):415–420. doi: 10.1097/01.mlr.0000156857.14152.6e. [DOI] [PubMed] [Google Scholar]
- 51.National Telecommunications and Information Administration and US Department of Commerce. Falling Through the Net: Defining the Digital Divide. Washington, DC: Government Printing Office; 1999. [Google Scholar]
- 52.Pew Hispanic Center. Washington, DC: Pew Research Center; c2011. Latinos Online, 2006-2008: Narrowing the Gap; 2009 Dec 22. Available from: http://pewhispanic.org/files/reports/119.pdf. Accessed on August 28, 2011. [Google Scholar]
- 53.Watson AJ, Bell AG, Kvedar JC, Grant RW. Reevaluating the digital divide: current lack of internet use is not a barrier to adoption of novel health information technology. Diabetes Care. 2008;31(3):433–435. doi: 10.2337/dc07-1667. Epub 2007 Dec 4. [DOI] [PubMed] [Google Scholar]
- 54.Pew Internet. Washington, DC: Pew Research Center; c2011. E-patients With a Disability or Chronic Disease; 2007 Oct 8. Available from: www.pewinternet.org/PPF/r/222/report_display.asp. Accessed on August 28, 2011. [Google Scholar]
- 55.Ancker JS, Barrón Y, Rockoff ML, Hauser D, Pichardo M, Szerencsy A, Calman N. Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med. 2011;26(10):1117–1123. doi: 10.1007/s11606-011-1749-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 57.Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, Sam J, Haynes RB. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;293(10):1223–1238. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- 58.Villagra VG, Ahmed T. Effectiveness of a disease management program for patients with diabetes. Health Aff (Millwood). 2004;23(4):255–266. doi: 10.1377/hlthaff.23.4.255. [DOI] [PubMed] [Google Scholar]
- 59.Grant RW, Wald JS, Schnipper JL, Gandhi TK, Poon EG, Orav EJ, Williams DH, Volk LA, Middleton B. Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2008;168(16):1776–1782. doi: 10.1001/archinte.168.16.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mathur A, Kvedar JC, Watson AJ. Connected health: a new framework for evaluation of communication technology use in care improvement strategies for type 2 diabetes. Curr Diabetes Rev. 2007;3(4):229–234. doi: 10.2174/157339907782330003. [DOI] [PubMed] [Google Scholar]
- 61.Jaana M, Paré G. Home telemonitoring of patients with diabetes: a systematic assessment of observed effects. J Eval Clin Pract. 2007;13(2):242–253. doi: 10.1111/j.1365-2753.2006.00686.x. [DOI] [PubMed] [Google Scholar]
- 62.Farmer A, Gibson OJ, Tarassenko L, Neil A. A systematic review of telemedicine interventions to support blood glucose self-monitoring in diabetes. Diabet Med. 2005;22(10):1372–1378. doi: 10.1111/j.1464-5491.2005.01627.x. [DOI] [PubMed] [Google Scholar]
- 63.Bull SS, Gaglio B, McKay HG, Glasgow RE. Harnessing the potential of the internet to promote chronic illness self-management: diabetes as an example of how well we are doing. Chronic Illn. 2005;1(2):143–155. doi: 10.1177/17423953050010021101. [DOI] [PubMed] [Google Scholar]
- 64.Shea S, Weinstock RS, Teresi JA, Palmas W, Starren J, Cimino JJ, Lai AM, Field L, Morin PC, Goland R, Izquierdo RE, Ebner S, Silver S, Petkova E, Kong J, Eimicke JP IDEATel Consortium. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16(4):446–456. doi: 10.1197/jamia.M3157. Epub 2009 Apr 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Moreno L, Dale SB, Chen AY, Magee CA. Costs to Medicare of the Informatics for Diabetes Education and Telemedicine (IDEATel) home telemedicine demonstration: findings from an independent evaluation. Diabetes Care. 2009;32(7):1202–1204. doi: 10.2337/dc09-0094. Epub 2009 Apr 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Watson AJ, Kvedar JC, Rahman B, Pelletier AC, Salber G, Grant RW. Diabetes connected health: a pilot study of a patient- and provider-shared glucose monitoring web application. J Diabetes Sci Technol. 2009;3(2):345–352. doi: 10.1177/193229680900300216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 68.Hibbard JH, Greene J, Becker ER, Roblin D, Painter MW, Perez DJ, Burbank-Schmitt E, Tusler M. Racial/ethnic disparities and consumer activation in health. Health Aff (Millwood). 2008;27(5):1442–1453. doi: 10.1377/hlthaff.27.5.1442. [DOI] [PubMed] [Google Scholar]
- 69.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007;42(4):1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Becker ER, Roblin DW. Translating primary care practice climate into patient activation: the role of patient trust in physician. Med Care. 2008;46(8):795–805. doi: 10.1097/MLR.0b013e31817919c0. [DOI] [PubMed] [Google Scholar]
- 71.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15(3):231–240. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 72.Downer SR, Meara JG, Da Costa AC, Sethuraman K. SMS text messaging improves outpatient attendance. Aust Health Rev. 2006;30(3):389–396. doi: 10.1071/ah060389. [DOI] [PubMed] [Google Scholar]
- 73.Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23(12):1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 74.National Health Interview Survey. Atlanta: Centers for Disease Control and Prevention. Wireless substitution: Early release of estimates based on data from the National Health Interview Survey, July-December 2010; 2011 June. Available from: http://www.cdc.gov/nchs/data/nhis/earlyrelease/wireless201106.htm. Accessed February 19, 2011.