Abstract
Objectives
Describe the health status and risk indicator trends in a representative sample of US healthcare workers aged 45+ years.
Methods
Using pooled data from the 1997–2009 National Health Interview Survey (NHIS), logistic regression analyses were performed to determine if age-group specific morbidity risks differed within occupational subgroups of the healthcare workforce (N=6,509). Health and morbidity trends were examined via complex survey adjusted and weighted Chi-square tests.
Results
Rates of functional limitation and hypertension increased among diagnosing/assessing healthcare workers. The prevalence of hearing impairment, cancer, and hypertension was 2–3x greater in health diagnosing/assessing workers 60+ years versus younger workers. Healthcare service workers were up to 19x more likely to be obese, compared to workers who diagnose/assess health.
Conclusions
Healthier workplaces and targeted interventions are needed to optimize the ability to meet healthcare demands of this aging workforce.
Keywords: occupational health, healthcare industry, US workers
The US workforce is growing older as more people delay retirement or continue working in their later years.1,2 According to the Bureau of Labor Statistics, the proportion of workers 55 years and older is projected to increase from 18.1% of the labor force in 2008 to 23.9% in 2018.3 This phenomenon extends to the healthcare workforce, in which more workers will be needed to meet rising healthcare demands, both in terms of volume and the complexity of care.4 With few exceptions, little is known about the health status of older US healthcare workers.5 In general, older workers typically experience physical and cognitive changes due to aging.6 Examples of physical and cognitive changes that accelerate after middle age include: decline of visual and hearing acuity, overall decline in health, increase in BMI, and increased risk of hypertension and coronary artery disease.7–9 Healthcare workers are at an increased risk for a wide range of hazards and occupational injuries and illnesses due to these underlying physical and cognitive changes combined with physical job demands, extended work schedules, and exposure to chemicals and pathogens.10 Furthermore, healthcare workforce job-specific demands can vary considerably from sedentary to physically demanding work activities. The level of physical demands associated with a given job may therefore influence the likelihood of continued employment as workers age. For example, nurse’s aides often engage in physically demanding work, such as heavy lifting.10 Incidence rates of musculoskeletal disorders in these workers are among the highest in the US workforce, and have recently been increasing.11,12 The aim of the present study was to investigate health status and risk indicator trends in a large representative sample of US healthcare workers 45 years of age and older.
Methods
Description of Survey
The National Health Interview Survey (NHIS) is an annual multipurpose household survey designed to be representative of the US civilian non-institutionalized population.13 Annual response rates to the 1997–2009 adult core, in which information on health and occupational status was collected, averaged 71.3% (range = 62.6 – 80.4).14–26
Measures
Occupational Classification
Participants 18 years or older were asked about employment status during the week prior to their NHIS interview.27 Between 1997–2004, the NHIS used a 41-category recode of the 1990 Standard Occupational Classification (SOC) System Census codes for occupation, which permitted the classification of healthcare workers into four categories:28 (1) health diagnosing occupations (e.g., physicians); (2) health assessing and treating occupations (e.g., registered nurses); (3) health technologists and technician occupations (e.g., licensed practical nurses); and (4) health service occupations (e.g., health and nursing aides). Table 1 includes all of the classifications included in the four categories. In 2005, a revision of the 2000 SOC codes was used to classify occupations.29,30 This necessitated collapsing workers into two categories: “health diagnosing/assessing/treating occupations,” and “health technologists/technicians and service occupations,” to examine trends over the 1997–2009 study period.
Table 1.
Standard Occupational Classification Codes and Corresponding Health Occupationsa
| Health Diagnosing Occupations | Physicians |
| Dentists | |
| Veterinarians | |
| Optometrists | |
| Podiatrists | |
| Health Diagnosing Practitioners, not classified elsewhere | |
| Health Assessing and Treating Occupations | Registered Nurses |
| Pharmacists | |
| Dietitians | |
| Respiratory Therapists | |
| Occupational Therapists | |
| Physical Therapists | |
| Speech Therapists | |
| Therapists, not classified elsewhere | |
| Physicians’ Assistants | |
| Health Technologist and Technicians | Clinical Laboratory Technologists and Technicians |
| Dental Hygienists | |
| Health Record Technologists and Technicians | |
| Radiologic Technicians | |
| Licensed Practical Nurses | |
| Health Technologists and Technicians, not classified elsewhere | |
| Health Service | Dental Assistants |
| Health Aides, Except Nursing | |
| Nursing Aides, Orderlies, and Attendants |
Source: Chou & Johnson28
Health Status and Risk Indicators
All selected health status and risk indicator measures were consistently assessed from 1997–2009 and used in previous publications.5,31,32 These included 12 items assessing functional limitations (e.g., “walk a quarter mile” and “push or pull large objects”). In this study, the report of any limitation was coded as having “any limited functioning” and three or more limitations were coded as having “limited functioning in three or more domains,” respectively. Obesity was defined as a body mass index (BMI) ≥ 30.0 kg/m2, and severe obesity was defined as a body mass index of ≥ 35.0 kg/m2. Report of current visual or hearing impairment was coded as previously described.31 Lifetime histories of healthcare provider-diagnosed cancer and hypertension and overall health status were reported.
Statistical Analysis
Analyses were completed with adjustments for sample weights and design effects using SUDAAN and SAS to obtain standard errors (SUDAAN, Language Manual, Release 9.0; SAS version 9.2). The pooled analyses across years 1997–2004 were performed in the four occupation groups for workers 45–59 years and 60 years and older (n = 4,149), with adjustments for survey weights.13,33 Chi-square tests were performed to determine if age-group specific morbidity risk estimates differed within occupational subgroups. Prevalence estimates for workers employed in the occupational subgroups were considered significantly different from the prevalence for all workers employed in the healthcare service sector if the corresponding subgroup 95% confidence interval did not include the overall sector prevalence rate estimate.34 Health and morbidity trends were examined from 1997 to 2009 via weighted linear regression models (including the intercept, occupational group, year, and the group-year interaction) and fit to the annual design-adjusted rates for the two collapsed healthcare occupational groups 45 years of age and older (n = 6,509). The weight used for each annual rate was the inverse of its variance. Respondents with missing information for a particular variable were excluded from these analyses.
Results
Workforce Age Trend Analyses: 1997–2009
The average age of the U.S. healthcare workforce 45 years of age and older significantly increased at an annual rate of 0.15 years among health diagnosing/assessing/treating workers (SE = 0.05; p = 0.005) and 0.12 years among workers employed in the health technologists/technicians and service occupations (SE = 0.05; p = 0.021). In 2009, the average age of workers 45 years and older in these two collapsed occupational categories was 54.1 and 54.9 years, respectively.
Demographic Characteristics of the US Healthcare Workforce: 1997–2004
In comparison to other workers in this sector, bivariate analyses reported in Table 2 reveal that those employed in the health diagnosing occupations were much more likely to be male (81% versus 9%–19%) and were more likely to be 60 years of age and older (26% versus 13%–21%). The demographic characteristics of the health assessing and treating occupations were similar to those employed in the health technologist/technician occupations, with the exception of a lower proportion of workers in this latter category with at least some college education (81% versus 97%). In comparison to other workers in this sector, those employed in the health service occupations were more likely to be female (92% vs. 19%–86%), report their race as Black (28% vs. 2%–13%), have less than a high school education (21% vs. 1%), and were living below the federal poverty line (10% vs. 1–2%).
Table 2.
Demographic Characteristics of the US Healthcare Sector Workforce Ages 45 and Older: Pooled Data, 1997–2004 National Health Interview Surveys
| Health Diagnosing Occupations (n=474) | Health Assessing and Treating Occupations (n=1,621) | Health Technologist/ Technician Occupations (n=699) | Health Service Occupations (n=1,341) | |
|---|---|---|---|---|
| Demographic Indicator | Percenta (SE) | Percenta (SE) | Percenta (SE) | Percenta (SE) |
| Age group | ||||
| 45–59 years | 73.8 (2.11) | 87.3 (0.86) | 86.9 (1.36) | 79.2 (1.22) |
| 60 and older | 26.2 (2.11) | 12.7 (0.86) | 13.1 (1.36) | 20.8 (1.22) |
| Gender | ||||
| Male | 80.6 (2.05) | 13.9 (1.07) | 19.3 (1.86) | 8.5 (1.00) |
| Female | 19.4 (2.05) | 86.1 (1.07) | 80.7 (1.86) | 91.5 (1.00) |
| Race | ||||
| White | 87.7 (1.88) | 86.2 (0.91) | 80.1 (1.77) | 66.0 (1.54) |
| Black | 2.4 (0.63) | 9.4 (0.67) | 12.6 (1.17) | 28.1 (1.49) |
| Other | 9.9 (1.81) | 4.4 (0.68) | 7.7 (1.45) | 5.8 (0.73) |
| Ethnicity | ||||
| Hispanic | 3.1 (0.88) | 3.1 (0.45) | 5.0 (0.83) | 9.8 (0.87) |
| Non-Hispanic | 96.9 (0.88) | 97.0 (0.45) | 95.0 (0.83) | 90.2 (0.87) |
| Educational attainment | ||||
| Less than high school | 0.5 (0.35) | 0.5 (0.17) | 1.3 (0.46) | 21.1 (1.28) |
| High school/GED | 0.9 (0.40) | 2.8 (0.46) | 17.8 (1.53) | 42.4 (1.47) |
| Some college or higher | 98.6 (0.53) | 96.7 (0.50) | 80.9 (1.60) | 36.5 (1.62) |
| Poverty statusb | ||||
| Not poor | 97.0 (0.92) | 97.5 (0.40) | 93.5 (1.06) | 65.5 (1.65) |
| Near poor | 1.8 (0.69) | 1.8 (0.32) | 5.0 (0.93) | 24.2 (1.43) |
| Poor | 1.2 (0.62) | 0.8 (0.25) | 1.6 (0.60) | 10.3 (0.95) |
Column totals for each demographic indicator do not always total 100% due to rounding error.
Based on ratio of family income to census-derived poverty threshold: not poor= 200% or higher; near poor= 100%-less than 200%; poor= less than 100%.
Pooled Morbidity Analyses: 1997–2004
The prevalence of morbidity indicators was often greater among older versus younger healthcare workers, although differences varied as a function of employment within each of the four healthcare occupational groups (Table 3). For example, there was a nearly two-fold difference in the prevalence of any functional limitation in older versus younger health diagnosing professions (22.6% versus 11.5%), with smaller age group differences observed in the other worker groups. The prevalence of hearing impairment, cancer, and hypertension was 2–3 times greater in the health diagnosing and among the health assessing/treating workers 60+ years relative to workers 45–59 years (all p-values <0.05). Prevalence rate differences in older versus younger health technologist/technician workers were not as large. The prevalence of hypertension, however, and of having three or more functional limitations were significantly higher in older versus younger workers. Prevalence rates were significantly larger in older versus younger service workers for reports of any functional limitations, reported hearing impairment and history of hypertension and coronary heart disease. However, rates of severe obesity were significantly lower in older versus younger health care service workers (8.5% versus 15.2%).
Table 3.
Prevalence of Health Status Indicators within Healthcare Occupations: Pooled Data, 1997–2004 National Health Interview Surveys
| Healthcare Service Sector Occupations | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All Healthcare Sector Workersa | Health Diagnosing Occupationsa,b | Health Assessing and Treating Occupationsa,b | Health Technologist/Technician Occupationsa,b | Health Service Occupationsa,b | ||||||
| 45–59 years (n=3,347) | 60 and older (n=802) | 45–59 years (n=343) | 60 and older (n=131) | 45–59 years (n=1,382) | 60 and older (n=239) | 45–59 years (n=590) | 60 and older (n=109) | 45–59 years (n=1,032) | 60 and older (n=323) | |
| Health Status/Risk Indicator | percent (95% CI) | percent (95% CI) | percent (95% CI) | percent (95% CI) | percent (95% CI) | percent (95% CI) | percent (95% CI) | percent (95% CI) | percent (95% CI) | percent (95% CI) |
| Any limited functioning | 28.9 (27.1–30.7) | 38.1 (34.3–42.0) | 11.5 (8.3–15.9) | 22.6 (15.3–32.0) | 26.6 (24.0–29.4) | 35.0 (28.6–42.0) | 32.5 (28.2–37.2) | 40.4 (29.7–52.1) | 37.9 (34.5–41.4) | 49.3 (43.2–55.4) |
| Limited functioning in ≥3 domains | 14.1 (12.9–15.5) | 19.3 (16.3–22.6) | 4.2 (2.5–7.2) | 11.1 (5.9–19.9) | 11.6 (9.9–13.5) | 14.5 (10.2–20.2) | 15.3 (12.5–18.7) | 24.3 (16.1–35.0) | 21.8 (18.9–25.0) | 26.4 (21.2–32.4) |
| BMI ≥30 | 25.5 (23.6–27.5) | 22.6 (19.3–26.3) | 10.0 (6.8–14.7) | 9.2 (5.0–16.2) | 23.0 (20.3–25.8) | 24.5 (18.6–31.5) | 26.9 (22.9–31.3) | 22.6 (15.1–32.5) | 35.8 (32.3–39.4) | 29.1 (23.6–35.3) |
| BMI ≥35 | 9.7 (8.6–11.0) | 6.9 (5.0–9.4) | 0.8 (0.2–2.9) | 0.5 (0.1–3.1) | 8.4 (6.8–10.3) | 8.0 (4.7–13.1) | 11.0 (8.6–14.0) | 10.2 (5.6–17.6) | 15.2 (12.8–17.9) | 8.5 (5.3–13.4) |
| Visual impairment | 9.2 (8.1–10.4) | 9.4 (7.5–11.7) | 3.5 (2.0–6.0) | 6.3 (3.2–11.7) | 7.3 (6.0–9.0) | 6.4 (3.7–11.0) | 9.2 (7.0–12.0) | 13.9 (8.2–22.8) | 14.7 (12.2–17.5) | 12.2 (8.8–16.6) |
| Hearing impairment | 13.2 (11.9–14.5) | 21.9 (18.7–25.6) | 15.6 (11.9–20.3) | 29.7 (22.5–38.1) | 10.7 (9.1–12.6) | 19.7 (14.5–26.2) | 13.1 (10.3–16.6) | 11.6 (5.9–21.3) | 16.0 (13.4–18.9) | 23.2 (18.3–28.9) |
| History of cancer | 7.0 (6.1–8.1) | 12.1 (9.6–15.2) | 7.2 (5.0–10.4) | 16.1 (10.6–23.7) | 7.1 (5.8–8.8) | 16.6 (11.3–23.7) | 6.9 (5.0–9.4) | 10.6 (6.1–18.0) | 7.0 (5.3–9.1) | 6.3 (4.0–9.8) |
| History of hypertension | 26.6 (24.8–28.4) | 47.1 (42.7–51.5) | 14.1 (10.8–18.3) | 42.9 (33.7–52.6) | 23.6 (21.1–26.4) | 48.0 (39.9–56.2) | 27.7 (23.9–31.9) | 41.3 (30.8–52.6) | 36.2 (32.9–39.6) | 51.0 (44.6–57.4) |
| History of coronary heart disease | 6.2 (5.4–7.2) | 11.5 (9.1–14.4) | 4.0 (2.1–7.5) | 14.7 (9.3–22.6) | 6.8 (5.5–8.3) | 11.1 (6.4–18.5) | 6.9 (5.0–9.4) | 10.7 (5.7–19.4) | 5.9 (4.4–8.0) | 10.1 (6.7–14.9) |
| History of asthma | 9.8 (8.6–11.2) | 7.0 (5.3–9.2) | 7.6 (4.8–11.9) | 6.4 (3.0–12.9) | 10.4 (8.7–12.4) | 5.5 (3.1–9.5) | 10.1 (7.7–13.1) | 8.5 (4.2–16.4) | 9.7 (7.7–12.3) | 8.2 (5.5–12.2) |
| Current fair/poor health rating | 7.3 (6.3–8.4) | 9.3 (7.3–11.8) | 2.3 (0.9–5.9) | 4.7 (1.7–12.4) | 3.9 (3.0–5.2) | 4.9 (2.5–9.3) | 6.4 (4.4–9.2) | 5.2 (2.3–11.5) | 15.6 (13.2–18.3) | 17.7 (13.7–22.7) |
Abbreviations: CI, confidence internal; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Within occupational sub-group category bolded prevalence estimates for 40–59 year old and 60 and older workers are significantly different at the p<0.05 level.
Italicized healthcare service sector occupational sub-group prevalence estimates are significantly lower or higher than the age-group specific estimates for the entire healthcare service sector workforce (p<0.05 level).
When making age-group specific comparisons across the occupational groups, health service workers were more likely to report functional limitations (up to a 3.3 fold difference), hypertension (up to a 2.6 fold difference), poor overall health (up to a 6.8 fold difference), and be obese (up to a 3.6 fold difference) relative to other healthcare worker groups. Rates of severe obesity were 19 times greater in younger health service workers relative to younger health-diagnosing workers (15.2% vs. 0.8%, respectively). Health diagnosing workers tended to report the lowest prevalence of health status and risk indicators, although workers 60+ years reported the highest prevalence of hearing impairment (29.7%) and heart disease (14.7%) relative to all other sub-groups.
Morbidity Trend Analyses: 1997–2009
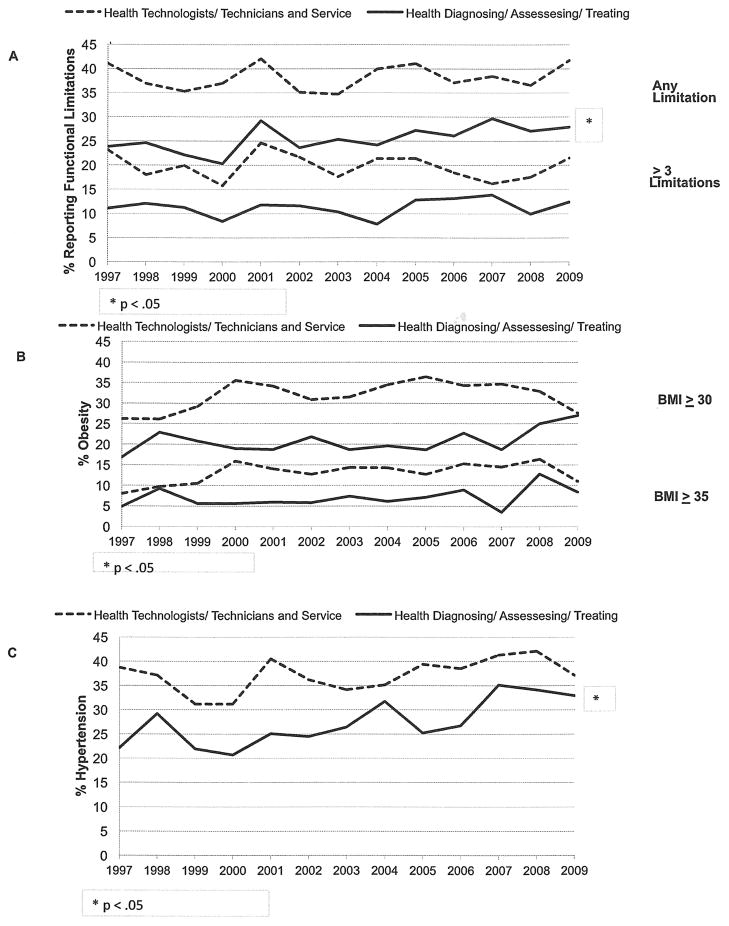
As shown in Figure 1 (Panel a), health diagnosing/assessing/treating occupations experienced a significant annual average increase in the prevalence of any functional limitation 0.46% (SE = 0.18; p = 0.021) from 1997 to 2009, but no increase was observed for health technologists/technicians and service workers 0.13% (SE = 0.20; p = 0.513). The prevalence of obesity and severe obesity varied between 1997 to 2009, with obesity rising for the health diagnosing/assessing/treating occupations from 17% in 1997 to 27% in 2009, but none of these trends were significant at the p < 0.05 level (Figure 1, Panel b). Panel c of Figure 1, however, reveals significant average annual increases in the prevalence of reported hypertension for health diagnosing/assessing/treating workers (0.89%; SE = 0.25; p = 0.002), but not for health technologists/technicians and service workers (0.42%; SE = 0.25; p = 0.108).
Figure 1.
Trends in the prevalence of functional limitations (panel a), obesity (panel b), and hypertension (panel c), in US healthcare workers 45 years of age and older: The 1997–2009 National Health Interview Surveys
Discussion
The present findings provide evidence that the proportion of workers reporting any difficulty with one or more activities (such as walking, stooping, or bending) has significantly increased over time among health diagnosing/assessing/treating workers aged 45 years and older. Additionally, the proportion of diagnosing/assessing/treating workers who reported being hypertensive also rose significantly over time. These trends foreshadow important resource needs for health care workers in the coming decade.
Similar to the U.S. workforce in general,27 the prevalence of obesity was significantly different by occupational grouping; it was lowest among health diagnosing occupations and highest among health service occupations. The proportion of older health service workers with severe obesity was significantly lower than in younger workers employed in the same sector (8.5% vs. 15.2%). This age-group pattern is generally opposite of that noted for other health status and risk indicators, irrespective of healthcare sector, and may be a reflection of work-selection processes, since severe obesity is associated with early retirement in the US workforce (Table 3).35 Given the documented association between mobility limitations and severe obesity levels in older adults,36 it is likely that the job demands inherent in many health service occupations only increase the risk of early retirement. Employment growth in the healthcare service sector is projected to be the greatest among health service occupations (e.g., home health aides and medical assistants),4 yet as noted in Table 3, the health status of this sector is substantially worse relative to those employed in other healthcare sectors. These traditionally poorly paid occupations often have limited employee benefits and are also characterized by high employee turnover, which adversely affects patient care. Work-related emotional strain also places an additional burden on many workers in this sector37.
As shown in Table 2, there is more demographic diversity among workers employed in the health service occupations. This diversity includes educational attainment from less than a high school education (21%) to some college or higher (37%). Such a range of educational levels can present challenges in the design and delivery of health education messaging and targeted health promotion interventions in older populations.38–40 Additionally, 10% of this workforce resides in households living below the poverty line. Health promotion activities are even more challenging among those living with limited financial resources.40 Although the research is limited, successful health promotion interventions in older workers in general,41 and specifically among health service workers and other nursing personnel,42,43 have been reported. Yet, most of these interventions have focused on improving physical fitness, teaching patient transfer skills and use of lift assist equipment,42–44 with only one reported intervention designed to reduce stress levels.45 The present research reveals the need for further development of a broad range of intervention strategies, which can reach this diverse and important workforce.
Limitations
The present analysis suffers from many of the limitations seen in large population-based studies including less than optimal response rates (pooled average=71%),5 and a limited selection of health indicators. For example, the NHIS does not include detailed questions on musculoskeletal injuries on an annual basis. The data are self-reported, and the degree of under-and over-reporting may vary as a function of age, gender, and socioeconomic indicators.46 Classification of occupation changed in 2005, which required us to collapse healthcare workers from four groups into two, possibly obscuring important differences in the changes in worker health in these two rather board categories. Sample sizes varied across the healthcare worker groups leading to differential power to detect statistically significant differences across these groups (Table 3). The strength of this study lies in the use of the NHIS, a nationally representative sample of the entire US population, which yielded a pooled sample of over 6,500 older healthcare workers available for analysis.
Recommendations
In addition to improving overall working conditions and benefits, targeted and integrated efforts are needed to address the impact of obesity on worker health across the life course. Only 18%–44% of employers have implemented programs to address older workers, 47 but interventions can begin early in the worker’s career with lasting impact on their lifestyle as they age.48 Previous literature has emphasized that the physical and psychosocial work environments should be adjusted to improve the work ability of older workers.49,50 Provision of workplace accommodations for health impairment has been shown to slow retirement, thus delaying Social Security payments.51,52 Such efforts will not only serve to stabilize and grow a vital sector of the US healthcare workforce, but may also address the large health inequalities presently seen in the US workforce.53
Acknowledgments
Source of Funding: National Institute of Occupational Safety and Health, 2R01OH003915
Footnotes
Conflicts of Interest: None declared
Contributor Information
David J. Lee, Email: DLee@med.miami.edu, Department of Epidemiology & Public Health, University of Miami Miller School of Medicine, 1120 NW 14th St, Room #1530, Miami, FL 33136, Tel: (305) 243-6980.
Lora E. Fleming, Email: LFleming@med.miami.edu, Department of Epidemiology & Public Health, University of Miami Miller School of Medicine, 1120 NW 14th Street, Room #1074, Miami, FL 33136, Tel: (305) 243-5912.
William G. LeBlanc, Email: thedatadoctor@gmail.com, Department of Epidemiology & Public Health, University of Miami Miller School of Medicine, 1120 NW 14th Street, Room #1075, Miami, FL 33136, Tel: (305) 243-3222.
Kristopher L. Arheart, Email: KArheart@biostat.med.miami.edu, Department of Epidemiology & Public Health, University of Miami Miller School of Medicine, 1120 NW 14th Street, Room #1067, Miami, FL 33136, Tel: (305) 243-3488.
Kenneth F. Ferraro, Email: Ferraro@purdue.edu, Center on Aging and the Life Course, Purdue University, 155 S. Grant Street, Young Hall, West Lafayette, IN 47907-2114, Tel: (765) 494-4707.
Marcie Pitt-Catsouphes, Email: Pittcats@bc.edu, Center on Aging & Work/Workplace Flexibility, Boston College, 308 McGuinn Hall, 140 Commonwealth Avenue, Chestnut Hill, MA 02467, Tel: (617) 552-4033.
Carles Muntaner, Email: carles_muntaner@camh.net, Department of Nursing, University of Toronto, 155 College Street, Rm. 386, Toronto ON M5T 1P8 Canada, Tel: (416) 978-5502.
Cristina A. Fernandez, Email: CFernandez5@med.miami.edu, 1120 NW 14th Street, Room #1074, Miami, FL 33136, Tel: (305) 243-3222
Alberto J. Caban-Martinez, Email: ACaban@med.miami.edu, Department of Epidemiology & Public Health, University of Miami Miller School of Medicine, 1120 NW 14th Street, Room #1075, Miami, FL 33136, Tel: (305) 243-7565.
Evelyn P. Davila, Email: miss_evelynda@yahoo.com, Department of Epidemiology & Public Health, University of Miami Miller School of Medicine, 1120 NW 14th Street, Room #1073, Miami, FL 33136, Tel: (305) 243-3222.
Frank C. Bandiera, Email: FBandiera@med.miami.edu, Department of Epidemiology & Public Health, University of Miami Miller School of Medicine, 1120 NW 14th Street, Room #1073, Miami, FL 33136, Tel: (305) 243-3222.
John E. Lewis, Email: jelewis@miami.edu, Department of Psychiatry & Behavioral Sciences, University of Miami Miller School of Medicine, 1120 NW 14th Street, Room #1474, Miami, FL 33136, Tel: (305) 243-6227.
Diana Kachan, Email: DKachan@med.miami.edu, Department of Epidemiology & Public Health, University of Miami Miller School of Medicine, 1120 NW 14th Street, Room #1073, Miami, FL 33136, Tel: (305) 243-3222
References
- 1.Wegman DH. Older workers. Occup Med. 1999 Jul-Sep;14(3):537–557. [PubMed] [Google Scholar]
- 2.Wegman DH, McGee JP. Health and Safety Needs of Older Workers. Washington, D.C: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 3.BLS. [Accessed November 10, 2011];Occupational outlook handbook. (2011). 2010–2011 http://www.bls.gov/oco/oco2003.htm.
- 4.IOM. Retooling for an aging America: Building the health care workforce. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 5.Fleming LE, Lee DJ, Martinez AJ, et al. The health behaviors of the older US worker. Am J Ind Med. 2007 Jun;50(6):427–437. doi: 10.1002/ajim.20468. [DOI] [PubMed] [Google Scholar]
- 6.Silverstein M. Meeting the challenges of an aging workforce. Am J Ind Med. 2008 Apr;51(4):269–80. doi: 10.1002/ajim.20569. [DOI] [PubMed] [Google Scholar]
- 7.Savinainen M, Nygard CH, Ilmarinen J. A 16-year follow-up study of physical capacity in relation to perceived workload among ageing employees. Ergonomics. 2004 Aug 15;47(10):1087–1102. doi: 10.1080/00140130410001686357. [DOI] [PubMed] [Google Scholar]
- 8.Virdis A, Bruno RM, Neves MF, Taddei S, Ghiadoni L. Hypertension in the Elderly: An Evidence-Based Review. Curr Pharm Des. 2011 Aug 24;17(28):3020–3031. doi: 10.2174/138161211798157711. [DOI] [PubMed] [Google Scholar]
- 9.Pew RW, Van Hemel SB, National Research Council (U.S.) Technology for adaptive aging. Washington, D.C: National Academies Press; 2004. Steering Committee for the Workshop on Technology for Adaptive Aging., National Research Council (U.S.). Board on Behavioral Cognitive and Sensory Sciences. [PubMed] [Google Scholar]
- 10.CDC. [Accessed August 25, 2011];Health care workers - NIOSH workplace safety and health topics. 2009 http://www.cdc.gov/niosh/topics/healthcare/
- 11.Wunderlich GS, Sloan FA, Davis CK Institute of Medicine (U.S.) Nursing staff in hospitals and nursing homes : is it adequate? Washington, D.C: National Academy Press; 1996. Committee on the Adequacy of Nurse Staffing in Hospitals and Nursing Homes. [PubMed] [Google Scholar]
- 12.BLS. [Accessed November 10, 2011];WORK, 2010 Non-Fatal Occupational Injuries and Illnesses Requiring Days Away from Work, 2010. 2011 http://www.bls.gov/news.release/pdf/osh2.pdf.
- 13.Botman SL, Moore TF, Moriarty CL, Parsons VL. Design and estimation for the National Health Interview Survey, 1995–2004. Vital Health Stat. 2000 Jun;2(130):1–31. [PubMed] [Google Scholar]
- 14.Division of Health Interview Statistics, National Center for Health Statistics. 2008 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, Maryland: Centers for Disease Control and Prevention. U.S. Department of Health and Human Services; Jun, 2009. [accessed October 19, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2008/srvydesc.pdf. [Google Scholar]
- 15.Division of Health Interview Statistics, National Center for Health Statistics. 2007 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, Maryland: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Jun, 2008. [accessed October 20, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2007/srvydesc.pdf. [Google Scholar]
- 16.Division of Health Interview Statistics, National Center for Health Statistics. 2006 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, Maryland: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Jun, 2007. [accessed October 30, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2006/srvydesc.pdf. [Google Scholar]
- 17.Division of Health Interview Statistics, National Center for Health Statistics. 2005 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, Maryland: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Jun, 2006. [accessed October 20, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2005/srvydesc.pdf. [Google Scholar]
- 18.Division of Health Interview Statistics, National Center for Health Statistics. 2004 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, Maryland: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Jul, 2005. [accessed October 20, 2009]. http://www.cdc.gov/nchs/data/nhis/srvydesc.pdf. [Google Scholar]
- 19.Division of Health Interview Statistics, National Center for Health Statistics. 2003 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Dec, 2004. [accessed October 20, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2003/srvydesc.pdf. [Google Scholar]
- 20.Division of Health Interview Statistics, National Center for Health Statistics. 2002 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Dec, 2003. [accessed October 20, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2002/srvydesc.pdf. [Google Scholar]
- 21.Division of Health Interview Statistics, National Center for Health Statistics. 2001 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Jan, 2003. [accessed October 20, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2001/srvydesc.pdf. [Google Scholar]
- 22.Division of Health Interview Statistics, National Center for Health Statistics. 2000 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: Centers for Disease Control and Prevention U.S. Department of Health and Human Services; Mar, 2002. [accessed October 20, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2000/srvydesc.pdf. [Google Scholar]
- 23.Division of Health Interview Statistics, National Center for Health Statistics. 1999 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: Centers for Disease Control and Prevention U.S. Department of Health and Human Services; Feb, 2002. [accessed October 20, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/1999/srvydesc.pdf. [Google Scholar]
- 24.Division of Health Interview Statistics, National Center for Health Statistics. 1998 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Oct, 2000. [accessed October 20, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/1998/srvydesc.pdf. [Google Scholar]
- 25.Division of Health Interview Statistics, National Center for Health Statistics. 1997 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, MD: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Feb, 2000. [accessed October 20, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/1997/srvydesc.pdf. [Google Scholar]
- 26.Division of Health Interview Statistics, National Center for Health Statistics. 2008 National Health Interview Survey (NHIS) Public Use Data Release. Hyattsville, Maryland: Centers for Disease Control and Prevention. U.S. Department of Health and Human Services; Jun, 2009. [accessed August 9, 2010]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2009/srvydesc.pdf. [Google Scholar]
- 27.Caban AJ, Lee DJ, Fleming LE, Gomez-Marin O, LeBlanc W, Pitman T. Obesity in US workers: The National Health Interview Survey, 1986 to 2002. Am J Public Health. 2005 Sep;95(9):1614–1622. doi: 10.2105/AJPH.2004.050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chou CF, Johnson PJ. Health disparities among America’s health care providers: evidence from the Integrated Health Interview Series, 1982 to 2004. J Occup Environ Med. 2008 Jun;50(6):696–704. doi: 10.1097/JOM.0b013e31816515b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.NHIS. 2005 NHIS Data Release. SOC Major Groups; [accessed November 1, 2009]. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2005/SOC_Major_Groups05.pdf. [Google Scholar]
- 30.Scopp TS. Technical Paper #65. U.S. Census Bureau; 2003. The Relationship between the 1990 Census and Census 2000 Industry and Occupation Classification Systems. [Google Scholar]
- 31.Davila EP, Caban-Martinez AJ, Muennig P, et al. Sensory impairment among older US workers. Am J Public Health. 2009 Aug;99(8):1378–1385. doi: 10.2105/AJPH.2008.141630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fleming LE. [accessed April 28, 2007];Interactive Monograph of Occupation, Disability, and Self-reported Health: The National Health Interview Survey (NHIS) 1986–1994 http://www.rsmas.miami.edu/groups/niehs/niosh/monographs.html.
- 33.Botman SL, Jack SS. Combining National Health Interview Survey Datasets: issues and approaches. Stat Med. 1995 Mar 15-Apr 15;14(5–7):669–677. doi: 10.1002/sim.4780140523. [DOI] [PubMed] [Google Scholar]
- 34.Rosner BA. Fundamentals of Biostatistics. 5. Pacific Grove, CA: Duxbury; 2000. [Google Scholar]
- 35.Renna F, Thakur N. Direct and indirect effects of obesity on U.S. labor market outcomes of older working age adults. Soc Sci Med. 2010 Jul;71(2):405–413. doi: 10.1016/j.socscimed.2010.03.038. [DOI] [PubMed] [Google Scholar]
- 36.Vincent HK, Vincent KR, Lamb KM. Obesity and mobility disability in the older adult. Obes Rev. 2010 Aug;11(8):568–579. doi: 10.1111/j.1467-789X.2009.00703.x. [DOI] [PubMed] [Google Scholar]
- 37.Muntaner C, Li Y, Xue X, Thompson T, Chung H, O’Campo P. County and organizational predictors of depression symptoms among low-income nursing assistants in the USA. Soc Sci Med. 2006 Sep;63(6):1454–1465. doi: 10.1016/j.socscimed.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 38.Institute of Medicine (U.S.) Speaking of health : assessing health communication strategies for diverse populations. Washington, D.C: National Academies Press; 2002. Committee on Communication for Behavior Change in the 21st Century: Improving the Health of Diverse Populations. [PubMed] [Google Scholar]
- 39.United States. Agency for Healthcare Research and Quality., Research Triangle Institute-University of North Carolina Evidence-based Practice Center. Literacy and health outcomes. Rockville, MD: The Agency; 2004. [Google Scholar]
- 40.Thompson SE, Smith BA, Bybee RF. Factors influencing participation in worksite wellness programs among minority and underserved populations. Fam Community Health. 2005 Jul-Sep;28(3):267–273. doi: 10.1097/00003727-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Crawford JO, Graveling RA, Cowie HA, Dixon K. The health safety and health promotion needs of older workers. Occup Med (Lond) 2010 May;60(3):184–192. doi: 10.1093/occmed/kqq028. [DOI] [PubMed] [Google Scholar]
- 42.Dawson AP, McLennan SN, Schiller SD, Jull GA, Hodges PW, Stewart S. Interventions to prevent back pain and back injury in nurses: a systematic review. Occup Environ Med. 2007 Oct;64(10):642–650. doi: 10.1136/oem.2006.030643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Skargren E, Oberg B. Effects of an exercise program on musculoskeletal symptoms and physical capacity among nursing staff. Scand J Med Sci Sports. 1996 Apr;6(2):122–130. doi: 10.1111/j.1600-0838.1996.tb00079.x. [DOI] [PubMed] [Google Scholar]
- 44.Evanoff B, Wolf L, Aton E, Canos J, Collins J. Reduction in injury rates in nursing personnel through introduction of mechanical lifts in the workplace. Am J Ind Med. 2003 Nov;44(5):451–457. doi: 10.1002/ajim.10294. [DOI] [PubMed] [Google Scholar]
- 45.Horneij E, Hemborg B, Jensen I, Ekdahl C. No significant differences between intervention programmes on neck, shoulder and low back pain: a prospective randomized study among home-care personnel. J Rehabil Med. 2001 Jul;33(4):170–176. [PubMed] [Google Scholar]
- 46.Engstrom JL, Paterson SA, Doherty A, Trabulsi M, Speer KL. Accuracy of self-reported height and weight in women: an integrative review of the literature. J Midwifery Womens Health. 2003 Sep-Oct;48(5):338–345. doi: 10.1016/s1526-9523(03)00281-2. [DOI] [PubMed] [Google Scholar]
- 47.AARP. [Accessed November 11, 2011];American business and older employees: A summary of findings. 2000 http://assets.aarp.org/rgcenter/econ/amer_bus_findings.pdf.
- 48.Capodaglio P. Physical exercise in the prevention of musculoskeletal diseases in the elderly worker. Med Lav. 2000 Jul-Aug;91(4):379–386. [PubMed] [Google Scholar]
- 49.Ilmarinen J, Rantanen J. Promotion of work ability during ageing. Am J Ind Med. 1999 Sep;(Suppl 1):21–23. doi: 10.1002/(sici)1097-0274(199909)36:1+<21::aid-ajim8>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 50.Ilmarinen J, Tuomi K, Klockars M. Changes in the work ability of active employees over an 11-year period. Scand J Work Environ Health. 1997;23( Suppl 1):49–57. [PubMed] [Google Scholar]
- 51.Burkhauser RV, Butler JS, Kim YM. The impairment of employer accommodation on job duration of workers with disabilities: A hazard model approach. Labor Economics. 1995;3(1):1–22. [Google Scholar]
- 52.Burkhauser RV, Butler JS, Kim YM, Weathers RR. The importance of accommodation on the timing of male disability insurance application: Results from the survey of disability and work and the health and retirement survey. Journal Human Resources. 1999;34(3):589–611. [Google Scholar]
- 53.Krieger N. Workers are people too: societal aspects of occupational health disparities--an ecosocial perspective. Am J Ind Med. 2010 Feb;53(2):104–115. doi: 10.1002/ajim.20759. [DOI] [PubMed] [Google Scholar]