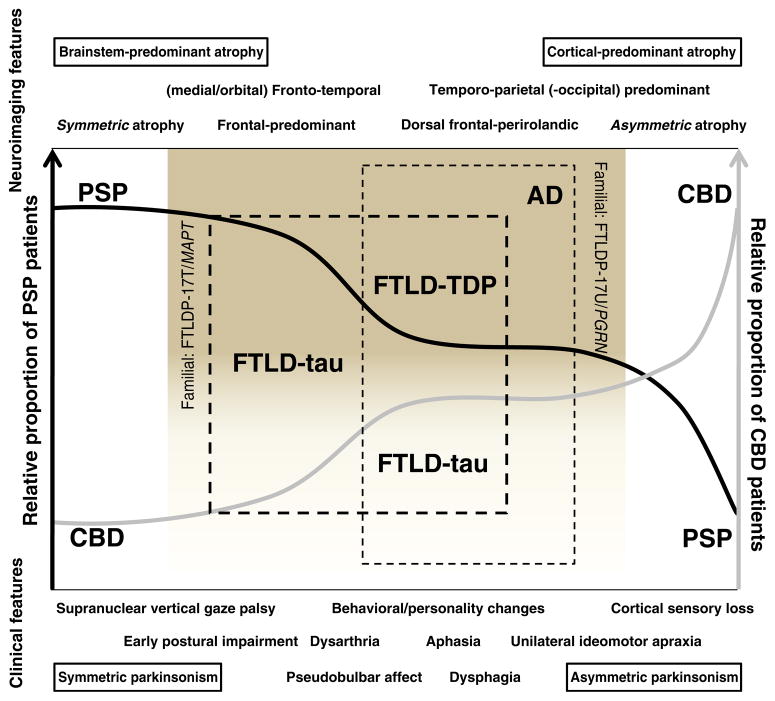
Fig. 1.
The overlap between PSP, CBD, and FTLD. The diagnostic certainty of PSP (black line) and CBD (gray line) varies depending on the relative presence or absence of clinical (bottom) and neuroimaging features (upper), and can be diagrammatically represented as belonging to a clinicopathologic spectrum. The “classical” clinical presentation of PSP (early falls, supranuclear vertical gaze palsy) can occur in a small proportion of patients with pathology-proven CBD (leftmost end of the proposed spectrum). Less characteristic presentations, or with co-occurrence of behavioral or personality changes or bulbar/pseudobulbar features may fall within the spectrum of FTLD, most often FTLD-tau (thick hashed line). Conversely, the typical phenotype of CBD (unilateral ideomotor apraxia, cortical sensory loss) can be present in a small proportion of patients with pathology proven PSP (right end of the diagram) or, particularly if behavioral or language abnormalities coexist, in patients with such pathologies as AD (the most common non-CBD etiology in CBS; thin hashed line), FTLD-tau, or FTLD-TDP. Neuroimaging patterns in the left end of the diagrammatic spectrum tend to show brainstem-predominant (PSP) and symmetric atrophy (FTLD-tau), whereas in the right end of the spectrum tend to show asymmetric (FTLD-TPD, particularly due to PGRN mutations) and posterior predominant patterns of atrophy (in particular, the posterior cortical atrophy pattern is a feature of some forms of CBD and AD). As a caveat, however, no pattern of atrophy can reliably distinguish FTLD-tau from FTLD-TDP