Abstract
Objective. Treatment-resistant muscle wasting is an increasingly recognized problem in idiopathic inflammatory myopathy (IIM). TNF-α is thought to induce muscle catabolism via activation of nuclear factor-kappa B (NF-κB). Several genes share homology with the NF-κB family of proteins. This study investigated the role of NF-κB-related genes in disease susceptibility in UK Caucasian IIM.
Methods. Data from 362 IIM cases [274 adults, 49 (±14.0) years, 72% female; 88 juveniles, 6 (±3.6) years, 73% female) were compared with 307 randomly selected Caucasian controls. DNA was genotyped for 63 single nucleotide polymorphisms (SNPs) from NF-κB-related genes. Data were stratified by IIM subgroup/serotype.
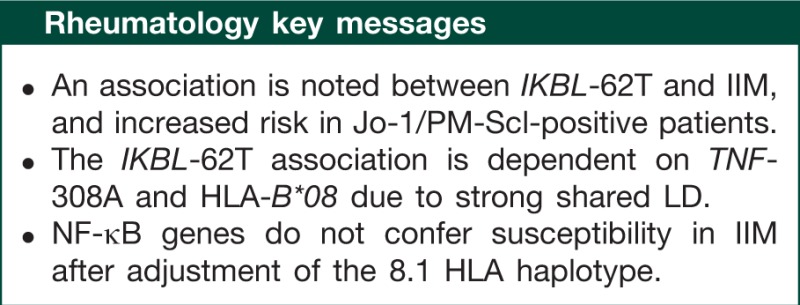
Results. A significant allele association was observed in the overall IIM group vs controls for the IKBL-62T allele (rs2071592, odds ratio 1.5, 95% CI 1.21, 1.89, corrected P = 0.0086), which strengthened after stratification by anti-Jo-1 or -PM-Scl antibodies. Genotype analysis revealed an increase for the AT genotype in cases under a dominant model. No other SNP was associated in the overall IIM group. Strong pairwise linkage disequilibrium was noted between IKBL-62T, TNF-308A and HLA-B*08 (D′ = 1). Using multivariate regression, the IKBL-62T IIM association was lost after adjustment for TNF-308A or HLA-B*08.
Conclusion. An association was noted between IKBL-62T and IIM, with increased risk noted in anti-Jo-1- and -PM-Scl antibody-positive patients. However, the IKBL-62T association is dependent on TNF-308A and HLA-B*08, due to strong shared linkage disequilibrium between these alleles. After adjustment of the 8.1 HLA haplotype, NF-κB genes therefore do not independently confer susceptibility in IIM.
Keywords: polymyositis, dermatomyositis, single nucleotide polymorphisms, immunogenetics, autoantibodies, NF-κB, TNF
Introduction
The idiopathic inflammatory myopathies (IIMs) represent a group of autoimmune muscle diseases characterized by muscle weakness, inflammatory muscle infiltrates in muscle biopsy samples and electromyographic abnormalities on neurophysiological testing. Although mortality rates are reportedly low [1, 2], IIM patients can suffer considerable disease-related morbidity or treatment-related complications. Thus, patients may become significantly disabled, with progressive weakness. Adults with IIM may suffer irreversible muscle wasting despite treatment and apparent resolution of inflammatory cell infiltrates [3]. Juvenile cases may additionally suffer specific complications including ongoing skin disease such as ulceration, calcinosis and joint contractures.
The cause of this irreversible muscle atrophy in adult IIM is unknown, although it is speculated that disease-related alteration of the endoplasmic reticulum stress response may cause metabolic changes to energy metabolism and fibre dysfunction [4]. The pro-inflammatory cytokine, TNF-α, is involved in muscle protein catabolic processes. TNF-α is thought to induce protein loss via oxidative activation of the myogenic transcription factor nuclear factor-kappa B (NF-κB). Furthermore, NF-κB p50 and p65 have been described within the inflammatory exudates of different IIM subtypes [5]. Several genes have been identified that share homology with the NF-κB family of proteins, including NFKB1, NFKB1A, NFKB1B, NFKB1E, IKBL (NFKBIL1), REL, RELB and BCL3. Current evidence for genetic risk in IIM arises from candidate gene studies comparing cases with controls. In a manner similar to other autoimmune diseases, the main IIM genetic risk factors lie within the HLA region, notably with components of the 8.1 common ancestral haplotype (8.1 haplotype) (HLA-B*08/DRB1*03/DQB1*02/DQA1*05) especially in the presence of certain myositis-specific/associated antibodies (MSAs/MAAs) [6–10]. Non-HLA genes are increasingly recognized as conferring a degree of risk [11]. In view of the apparently key role that NF-κB may play in skeletal muscle protein catabolism and the described clinical problem of muscle dysfunction and wasting in IIM, the study reported here investigated genes involved with the NF-κB pathway in adult and juvenile UK Caucasian IIM patients.
Patients and methods
Subjects
DNA was available from 362 UK Caucasian IIM cases. Adult IIM patients (n = 274), aged ⩾18 years of age at disease onset, were recruited through the UK Adult Onset Myositis Immunogenetic Collaboration (AOMIC) [10]. JDM patients (n = 88) were recruited via the UK Juvenile Dermatomyositis National (UK and Ireland) Cohort Biomarker Study and Repository [12–14]. Patients with PM, DM or JDM had probable or definite myositis, based on the Bohan and Peter criteria [15, 16]. Myositis/CTD-overlap patients were included if they fulfilled all of the following: (i) met published criteria for their primary CTD [17–21] or MCTD [22]; (ii) possessed at least two of four Bohan and Peter criteria (proximal muscle weakness, elevated muscle enzymes, characteristic myopathic EMG changes and diagnostic muscle biopsy); and (iii) possessed at least one MSA/MAA. A standardized clinical data collection form detailed demographics and individual clinical details.
Controls
Three hundred and seven UK Caucasian control subjects were recruited from blood donors and general practitioner registers as described [10]. The study was approved by local research ethics committees [Northern and Yorkshire Multi-centre Research Ethics Committee (juvenile cases MREC 1/3/22); North West Research Multi-centre Research Ethics Committee (adult cases MREC 98/8/86)] and full informed consent was obtained according to the Declaration of Helsinki.
Autoantibody typing
Serum was obtained from patients for determination of MSAs: anti-synthetases: -Jo-1, -PL-7, -PL-12, -EJ, -OJ, -KS; anti-Mi-2, anti-SRP, anti-155/140; and MAAs: anti-PM-Scl, anti-Ku, anti-U1-RNP, anti-U3-RNP using radioimmunoprecipitation, as previously described in adult [10, 23] and juvenile IIM [13].
Genotyping
DNA samples were extracted from a peripheral blood sample obtained from both cases and controls using a standard phenol–chloroform method. Single nucleotide polymorphisms (SNPs) were genotyped using the Sequenom MassArray iPLEX platform, as per the manufacturer's instructions (http://www.sequenom.com/seq-genotyping.html). HLA Class I and TNF typing have been described previously [10, 24].
NF-κB SNPs
Sixty-three SNPs within the NF-κB family were initially selected from the following genes: NFKB1, NFKB1A, NFKB1B, NFKB1E, IKBL (NFKBIL1), REL, RELB and BCL3. Thirty-eight haplotype tagging (ht) SNPs were selected for genotyping using the Hapmap CEU population (release 20, National Center for Biotechnology Information B35 assembly, online at www.ncbi.nlm.nih.gov) by pairwise tagging, r2 cut-off ≥0.8 and a minor allele frequency (MAF) of 10%. The remainder of the SNPs were selected on the basis of being synonymous, non-synonymous, 3′-untranslated region or in the 5′-upstream region. Conserved non-coding SNPs were also selected using an approach outlined by Bejerano et al. [25], to obtain sequences of conserved non-coding regions from a wide range of organisms, using the UCSC Genome Browser database (http://genome.ucsc.edu/cgi-bin/hgGateway). Fourteen SNPs were removed as they were rejected by Sequenom assay design, three SNPs were removed as they were not compatible with the plexes created and three SNPs were rejected where the sample genotyping success rate was <85%. For the purposes of analysis, assay success cut-off was set at 90%. Thus, a remainder of 43 SNPs were available for the final analysis (a summary of the SNPs is available in the supplementary Table 1, available as supplementary data at Rheumatology online). A power calculation was applied to the SNP with the lowest MAF (rs4648127, 10%). For 95% power to detect an effect size of 2.0 at a 95% significance level, a sample size of 338 cases and 282 controls would be required.
Statistical analyses
Genotype frequencies for each NF-κB SNP were tested for Hardy–Weinberg equilibrium (HWE) in each group. Allele and genotype frequencies of these NF-κB SNPs were compared between myositis cases and controls, using Fisher's exact test or chi-square test, as appropriate. Where significant, data were expressed as odds ratios (ORs) with exact 95% CIs and pointwise P-values were corrected using Bonferroni. Linkage disequilibrium (LD) was calculated using the measure of D′. The analyses were also repeated after stratification by clinical and serological subgroup. Unless otherwise stated, the statistical package Stata (release 9.2, Stata Corp., College Station, TX, USA) was used to perform statistical analysis.
Results
The breakdown of the IIM groups was as follows: 274 adults, 49 (±14.0) years, 72% female; 88 juvenile, 6 (±3.6) years, 73% female. All 43 SNPs conformed to HWE. The frequency of the IKBL-62T allele (rs2071592) was significantly increased in the overall IIM group vs controls (Table 1). This association persisted after stratification by clinical subgroup, and no significant difference was observed between the subgroup frequencies of IKBL-62T. The data were then further stratified by serological subgroup. The IKBL-62T association was strengthened after stratification by either anti-Jo-1 or -PM-Scl antibody (Table 1). Genotype analysis of the overall IIM group revealed an increase of the AT genotype in cases (Table 2), with a significant association noted under a dominant model of inheritance (Table 3). No other SNP was significantly increased in the overall IIM group or clinical/serological subgroups. The relationship between IKBL-62T, TNF-α and HLA Class I was then examined. The relationship between TNF-308A and HLA-B*08 in adult IIM has previously been described [24]. Strong pairwise LD was noted between IKBL-62T, TNF-308A and HLA-B*08 (D′ = 1). Using multivariate logistic regression, the IKBL-62T association with IIM was lost after adjusting for the presence of either TNF-308A or HLA-B*08.
Table 1.
IKBL-62T allele associations in clinical and antibody IIM subgroups
| n | Minor allele (T) frequency (%) | OR (95% CI) | P-value | Bonferroni-corrected P-value | |
|---|---|---|---|---|---|
| Controls | 307 | 34.4 | |||
| Overall | 362 | 44.3 | 1.5 (1.21, 1.89) | 0.0002 | 0.0086 |
| PM | 112 | 44.6 | 1.5 (1.12, 2.10) | 0.004 | 0.17 |
| DM | 98 | 42.9 | 1.4 (1.03, 1.99 | 0.03 | 1.29 |
| CTD/overlap | 64 | 47.7 | 1.7 (1.18, 2.55) | 0.006 | 0.26 |
| JDM | 88 | 42.6 | 1.4 (1.01, 2.0) | 0.05 | 2.15 |
| Jo-1 | 50 | 58.0 | 2.6 (1.72, 4.05) | 0.00001 | 0.0004 |
| PM-Scl | 36 | 59.7 | 2.8 (1.72, 4.65) | 0.00005 | 0.002 |
Significant antibody associations are shown in bold. Associations are presented assuming a dominant mode of inheritance.
Table 2.
IKBL62 SNP genotype frequencies in combined IIM cases compared with controls
| Genotype | Controls (n = 307) | IIM (n = 362) |
|---|---|---|
| n (%) | n (%) | |
| AA | 134 (43.6) | 101 (27.9) |
| AT | 135 (44.0) | 202 (55.8) |
| TT | 38 (12.4) | 59 (16.3) |
Table 3.
IKBL62 SNP genotype associations in overall IIM cases vs controls
| Genotype test | P | OR (95% CI) |
|---|---|---|
| AT + TT vs AA | 0.00002 | 2.0 (1.45, 2.76) |
| TT vs AT + AA | 0.15 | 1.38 (0.89, 2.14) |
| TT vs AA | 0.003 | 2.06 (1.27, 3.34) |
| AT vs AA | 0.88 | 0.96 (0.61, 1.53) |
P-values are uncorrected.
Discussion
This candidate gene study tested the hypothesis that NF-κB-related genes may confer susceptibility in IIM. An SNP, rs2071592 (IKBL-62T), was found to be significantly increased in IIM, especially in anti-Jo-1- and PM-Scl-positive cases when compared with controls. However, a strong LD relationship was confirmed between IKBL-62T and alleles forming part of the HLA 8.1 ancestral haplotype, and indeed after adjusting for TNF-308A and HLA-B*08, the association of IKBL-62T with IIM was lost.
The IKBL-62T SNP implicated in this study is in the promoter region of the IKBL gene, which is located on the telomeric end of the MHC on Chromosome 6, and codes for a member of the IκB family. IκB proteins have a regulatory role, through binding and then sequestration of NF-κB in the cytoplasm, thus inhibiting translocation to the nucleus [26]. Polymorphisms within genes encoding IκB proteins have been investigated in a number of other autoimmune conditions including multiple sclerosis, RA, type 1 diabetes mellitus, SLE and Grave's disease in different populations [27–33].
Data surrounding the IKBL-62T SNP remain conflicting. Disruption of an E-box binding element in the IKBL promoter by the IKBL-62T SNP has been described in binding studies [34], which of interest is a sequence shared in many B- and T-cell lineage-specific genes. Decreased IKBL promoter activity has also been functionally associated with the IKBL-62A allele, culminating in an exaggerated NF-κB-mediated inflammatory response [35]. A study of subjects with Grave's disease identified a higher frequency of IKBL-62A when compared with healthy controls [33]. In contrast, IKBL-62T was found to be linked to RA in a Japanese population study [29], then known as SNP96452 (OR 2.08, P = 0.0088). This study did not, however, report on LD effects with HLA-DRB1 alleles, nor was the effect replicated in a UK family-based study [30] or a Spanish case–control study [31].
There is increasing evidence for a role of the NF-κB in alteration of normal muscle physiology. Transgenic overexpression of NF-κB (via activated IKB kinase b) causes profound muscle wasting in mice via accelerated protein breakdown through ubiquitin-dependent proteolysis [36]. In a mechanistically reverse experiment, Mourkioti et al. [37] demonstrated that suppression of NF-κB response by IKK2 muscle-specific deletion protected skeletal muscle from atrophy despite denervation injury via both enhanced regeneration (satellite cell activation) and reduced fibrosis. In human IIM, NF-κB activation has been demonstrated by western blot analysis and electrophoretic mobility shift assays on muscle biopsies in patients with PM and DM [38]. Furthermore, NF-κB p50 and p65 is found in CD4+ T cells in muscle biopsies from both PM and IBM [5]. In human IBM and a myositis mouse model, overexpression of MHC Class I on muscle fibres results in activation of NF-κB and an endoplasmic reticulum stress response [4, 39, 40]. LEF, among its many actions, is a potent NF-kB inhibitor and has been reported to be effective in resistant cases of PM and DM [41, 42].
Alleles forming part of the 8.1 Caucasian MHC common ancestral haplotype (HLA-A1-B8-Cw7-DRB1*0301-DQA1*0501-C4A*Q0) occur in strong LD within Caucasian populations in northern and western Europe, and represent risk factors for a large number of immunopathological diseases [43]. To date, the 8.1 haplotype has also been identified as a major risk factor in IIM [44, 45]. Thus, IKBL-62T confers risk for IIM as this allele forms part of the 8.1 haplotype where it shares strong LD with other alleles. We hypothesize that an altered NF-κB response and cytokine profile could relate to previous observations that the 8.1 haplotype confers an immune hyperresponsiveness [46, 47].
Due to the rarity of IIM, difficulties will always be encountered when trying to recruit a sufficient number of cases for analysis in genetic association studies that examine SNPs with a modest effect size. The present study was not powered to detect associations after stratification by disease or serological subgroups. This may also explain why no significant associations were observed for the other SNPs with a low MAF. The SNPs tested were htSNPs, which means that the true causal SNP may not have been tested directly in the current study. Due to the limited number of SNPs tested and assay design failure, there will be incomplete coverage of the tested regions. Furthermore, we have not corroborated our findings with functional data. Finally, clinical associations with these SNPs may be due to factors other than irreversible muscle atrophy, certainly within the juvenile cohort where this clinical feature is generally not typical.
To conclude, these findings describe the association of IKBL-62T with IIM susceptibility in a large cohort of adult and juvenile UK Caucasians. Significant differences are not apparent between IIM subgroups and the risk appears strongest in anti-Jo-1 and -PM-Scl cases, where the 8.1 haplotype association is the strongest. This study furthers our understanding of the 8.1 haplotype in IIM and should trigger off more detailed and functional studies into NF-κB-related pathways.
Supplementary data
Supplementary data are available at Rheumatology Online.
Acknowledgements
We wish to thank the UK physicians who contributed to UK AOMIC. Their names and affiliations are cited in Ref. [10].
Funding: Supported by the Arthritis Research UK (16 082 to H.C., 18 136 to H.G.) and the UK Myositis Support Group (Letitia Rawson Fellowship to Z.B.). The Juvenile Dermatomyositis Registry and Repository (UK and Ireland) was supported by generous funding from the UK Raynaud's and Scleroderma Association (AH1), Cathal Hayes Research Foundation and Action Medical Research (SP4252).
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.Danko K, Ponyi A, Constantin T, et al. Long-term survival of patients with idiopathic inflammatory myopathies according to clinical features: a longitudinal study of 162 cases. Medicine. 2004;83:35–42. doi: 10.1097/01.md.0000109755.65914.5e. [DOI] [PubMed] [Google Scholar]
- 2.Lundberg IE, Forbess CJ. Mortality in idiopathic inflammatory myopathies. Clin Exp Rheumatol. 2008;26:S109–14. [PubMed] [Google Scholar]
- 3.Englund P, Lindroos E, Nennesmo I, et al. Skeletal muscle fibers express major histocompatibility complex class II antigens independently of inflammatory infiltrates in inflammatory myopathies. Am J Pathol. 2001;159:1263–73. doi: 10.1016/S0002-9440(10)62513-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nagaraju K, Casciola-Rosen L, Lundberg I, et al. Activation of the endoplasmic reticulum stress response in autoimmune myositis: potential role in muscle fiber damage and dysfunction. Arthritis Rheum. 2005;52:1824–35. doi: 10.1002/art.21103. [DOI] [PubMed] [Google Scholar]
- 5.Creus KK, De PB, Werbrouck BF, et al. Distribution of the NF-kappaB complex in the inflammatory exudates characterizing the idiopathic inflammatory myopathies. Ann N Y Acad Sci. 2009;1173:370–7. doi: 10.1111/j.1749-6632.2009.04874.x. [DOI] [PubMed] [Google Scholar]
- 6.Love LA, Leff RL, Fraser DD, et al. A new approach to the classification of idiopathic inflammatory myopathy: myositis-specific autoantibodies define useful homogeneous patient groups. Medicine. 1991;70:360–74. doi: 10.1097/00005792-199111000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Arnett FC, Targoff IN, Mimori T, et al. Interrelationship of major histocompatibility complex class II alleles and autoantibodies in four ethnic groups with various forms of myositis. Arthritis Rheum. 1996;39:1507–18. doi: 10.1002/art.1780390910. [DOI] [PubMed] [Google Scholar]
- 8.Hausmanowa-Petrusewicz I, Kowalska-Oledzka E, Miller FW, et al. Clinical, serologic, and immunogenetic features in Polish patients with idiopathic inflammatory myopathies. Arthritis Rheum. 1997;40:1257–66. doi: 10.1002/1529-0131(199707)40:7<1257::AID-ART10>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 9.O'Hanlon TP, Carrick DM, Arnett FC, et al. Immunogenetic risk and protective factors for the idiopathic inflammatory myopathies: distinct HLA-A, -B, -Cw, -DRB1 and -DQA1 allelic profiles and motifs define clinicopathologic groups in caucasians. Medicine. 2005;84:338–49. doi: 10.1097/01.md.0000189818.63141.8c. [DOI] [PubMed] [Google Scholar]
- 10.Chinoy H, Salway F, Fertig N, et al. In adult onset myositis, the presence of interstitial lung disease and myositis specific/associated antibodies are governed by HLA class II haplotype, rather than by myositis subtype. Arthritis Res Ther. 2006;8:R13. doi: 10.1186/ar1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chinoy H, Lamb JA, Ollier WE, et al. An update on the immunogenetics of idiopathic inflammatory myopathies: major histocompatibility complex and beyond. Curr Opin Rheumatol. 2009;21:588–93. doi: 10.1097/BOR.0b013e3283315a22. [DOI] [PubMed] [Google Scholar]
- 12.McCann LJ, Juggins AD, Maillard SM, et al. The Juvenile Dermatomyositis National Registry and Repository (UK and Ireland)–clinical characteristics of children recruited within the first 5 yr. Rheumatology. 2006;45:1255–60. doi: 10.1093/rheumatology/kel099. [DOI] [PubMed] [Google Scholar]
- 13.Wedderburn LR, McHugh NJ, Chinoy H, et al. HLA class II haplotype and autoantibody associations in children with juvenile dermatomyositis and juvenile dermatomyositis-scleroderma overlap. Rheumatology. 2007;46:1786–91. doi: 10.1093/rheumatology/kem265. [DOI] [PubMed] [Google Scholar]
- 14.Martin N, Krol P, Smith S, et al. A national registry for juvenile dermatomyositis and other paediatric idiopathic inflammatory myopathies: 10 years’ experience; the Juvenile Dermatomyositis National (UK and Ireland) Cohort Biomarker Study and Repository for Idiopathic Inflammatory Myopathies. Rheumatology. 2011;50:137–45. doi: 10.1093/rheumatology/keq261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts) N Engl J Med. 1975;292:344–7. doi: 10.1056/NEJM197502132920706. [DOI] [PubMed] [Google Scholar]
- 16.Bohan A, Peter JB. Polymyositis and dermatomyositis (second of two parts) N Engl J Med. 1975; 292:403–7. doi: 10.1056/NEJM197502202920807. [DOI] [PubMed] [Google Scholar]
- 17.Tan EM, Cohen AS, Fries JF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–7. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 18.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40:1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 19.Preliminary criteria for the classification of systemic sclerosis (scleroderma) Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1980;23:581–90. doi: 10.1002/art.1780230510. [DOI] [PubMed] [Google Scholar]
- 20.Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 21.Vitali C, Bombardieri S, Moutsopoulos HM, et al. Preliminary criteria for the classification of Sjogren's syndrome. Results of a prospective concerted action supported by the European Community. Arthritis Rheum. 1993;36:340–7. doi: 10.1002/art.1780360309. [DOI] [PubMed] [Google Scholar]
- 22.Alarcon-Segovia D. Mixed connective tissue disease and overlap syndromes. Clin Dermatol. 1994;12:309–16. doi: 10.1016/s0738-081x(94)90336-0. [DOI] [PubMed] [Google Scholar]
- 23.Chinoy H, Fertig N, Oddis CV, et al. The diagnostic utility of myositis autoantibody testing for predicting the risk of cancer-associated myositis. Ann Rheum Dis. 2007;66:1345–9. doi: 10.1136/ard.2006.068502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chinoy H, Salway F, John S, et al. Tumour necrosis factor-alpha single nucleotide polymorphisms are not independent of HLA class I in UK Caucasians with adult onset idiopathic inflammatory myopathies. Rheumatology. 2007;46:1411–6. doi: 10.1093/rheumatology/kem145. [DOI] [PubMed] [Google Scholar]
- 25.Bejerano G, Siepel AC, Kent WJ, et al. Computational screening of conserved genomic DNA in search of functional noncoding elements. Nat Methods. 2005;2:535–45. doi: 10.1038/nmeth0705-535. [DOI] [PubMed] [Google Scholar]
- 26.Hayden MS, Ghosh S. Shared principles in NF-kappaB signaling. Cell. 2008;132:344–62. doi: 10.1016/j.cell.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 27.Price P, Cheong KY, Boodhoo A, et al. Can MHC class II genes mediate resistance to type 1 diabetes? Immunol Cell Biol. 2001;79:602–6. doi: 10.1046/j.1440-1711.2001.01043.x. [DOI] [PubMed] [Google Scholar]
- 28.Miterski B, Bohringer S, Klein W, et al. Inhibitors in the NFkappaB cascade comprise prime candidate genes predisposing to multiple sclerosis, especially in selected combinations. Genes Immun. 2002;3:211–9. doi: 10.1038/sj.gene.6363846. [DOI] [PubMed] [Google Scholar]
- 29.Okamoto K, Makino S, Yoshikawa Y, et al. Identification of I kappa BL as the second major histocompatibility complex-linked susceptibility locus for rheumatoid arthritis. Am J Hum Genet. 2003;72:303–12. doi: 10.1086/346067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kilding R, Iles MM, Timms JM, et al. Additional genetic susceptibility for rheumatoid arthritis telomeric of the DRB1 locus. Arthritis Rheum. 2004;50:763–9. doi: 10.1002/art.20043. [DOI] [PubMed] [Google Scholar]
- 31.Collado L, Rueda B, Caliz R, et al. Lack of association between the I kappa BL promoter polymorphism and rheumatoid arthritis. Arthritis Rheum. 2004;50:2032–3. doi: 10.1002/art.20215. [DOI] [PubMed] [Google Scholar]
- 32.Lin CH, Wang SC, Ou TT, et al. I kappa B alpha promoter polymorphisms in patients with systemic lupus erythematosus. J Clin Immunol. 2008;28:207–13. doi: 10.1007/s10875-007-9156-1. [DOI] [PubMed] [Google Scholar]
- 33.Kurylowicz A, Miskiewicz P, Bar-Andziak E, et al. Association of polymorphism in genes encoding kappaB inhibitors (IkappaB) with susceptibility to and phenotype of Graves’ disease: a case-control study. Thyroid Res. 2009;2:10. doi: 10.1186/1756-6614-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Allcock RJ, Baluchova K, Cheong KY, et al. Haplotypic single nucleotide polymorphisms in the central MHC gene IKBL, a potential regulator of NF-kappaB function. Immunogenetics. 2001;52:289–93. doi: 10.1007/s002510000280. [DOI] [PubMed] [Google Scholar]
- 35.Ozaki K, Ohnishi Y, Iida A, et al. Functional SNPs in the lymphotoxin-alpha gene that are associated with susceptibility to myocardial infarction. Nat Genet. 2002;32:650–4. doi: 10.1038/ng1047. [DOI] [PubMed] [Google Scholar]
- 36.Cai D, Frantz JD, Tawa NE, Jr, et al. IKKbeta/NF-kappaB activation causes severe muscle wasting in mice. Cell. 2004;119:285–98. doi: 10.1016/j.cell.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 37.Mourkioti F, Kratsios P, Luedde T, et al. Targeted ablation of IKK2 improves skeletal muscle strength, maintains mass, and promotes regeneration. J Clin Invest. 2006;116:2945–54. doi: 10.1172/JCI28721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Monici MC, Aguennouz M, Mazzeo A, et al. Activation of nuclear factor-kappaB in inflammatory myopathies and Duchenne muscular dystrophy. Neurology. 2003;60:993–7. doi: 10.1212/01.wnl.0000049913.27181.51. [DOI] [PubMed] [Google Scholar]
- 39.Vattemi G, Engel WK, McFerrin J, et al. Endoplasmic reticulum stress and unfolded protein response in inclusion body myositis muscle. Am J Pathol. 2004;164:1–7. doi: 10.1016/S0002-9440(10)63089-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li CK, Knopp P, Moncrieffe H, et al. Overexpression of MHC class I heavy chain protein in young skeletal muscle leads to severe myositis: implications for juvenile myositis. Am J Pathol. 2009;175:1030–40. doi: 10.2353/ajpath.2009.090196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lange U, Piegsa M, Muller-Ladner U, et al. Anti-Jo-1 antibody positive polymyositis–successful therapy with leflunomide. Autoimmunity. 2006;39:261–4. doi: 10.1080/08916930600623874. [DOI] [PubMed] [Google Scholar]
- 42.Sangle VS, Sangle SR, D'Cruz DP. Leflunomide as a remission-maintaining therapy in difficult-to-treat dermatomyositis. Ann Rheum Dis. 2008;67:723. doi: 10.1136/ard.2007.073221. [DOI] [PubMed] [Google Scholar]
- 43.Price P, Witt C, Allcock R, et al. The genetic basis for the association of the 8.1 ancestral haplotype (A1, B8, DR3) with multiple immunopathological diseases. Immunol Rev. 1999;167:257–74. doi: 10.1111/j.1600-065x.1999.tb01398.x. [DOI] [PubMed] [Google Scholar]
- 44.Shamim EA, Rider LG, Miller FW. Update on the genetics of the idiopathic inflammatory myopathies. Curr Opin Rheumatol. 2000;12:482–91. doi: 10.1097/00002281-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 45.Chinoy H, Ollier WE, Cooper RG. Have recent immunogenetic investigations increased our understanding of disease mechanisms in the idiopathic inflammatory myopathies? Curr Opin Rheumatol. 2004;16:707–13. doi: 10.1097/01.bor.0000142339.24380.b7. [DOI] [PubMed] [Google Scholar]
- 46.Parham P. Virtual reality in the MHC. Immunol Rev. 1999;167:5–15. doi: 10.1111/j.1600-065x.1999.tb01378.x. [DOI] [PubMed] [Google Scholar]
- 47.Candore G, Lio D, Colonna Romano G, et al. Pathogenesis of autoimmune diseases associated with 8.1 ancestral haplotype: effect of multiple gene interactions. Autoimmunity Reviews. 2002;1:29–35. doi: 10.1016/s1568-9972(01)00004-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


