Abstract
Background:
Ruptured uterus is a major life-threatening condition encountered mostly in developing countries and is an index of failure of obstetric care at a point in time in a woman's reproductive career. With worsening economic condition, increasing caesarean section rates, and patients’ aversion for operative delivery this condition would still remain a major obstetric matter for discussion.
Objective:
To identify the incidence, sociodemographic variables, clinical characteristics, causes, and outcome of ruptured uterus at the University of Port Harcourt Teaching Hospital.
Materials and Methods:
A 5-year retrospective study of cases of ruptured uterus at the University of Port Harcourt Teaching Hospital was carried out. The case notes of 40 patients with uterine rupture during the period 2003-2007 were analyzed. Data collected included sociodemographic characteristics, etiologic factors, clinical presentation, and outcome. Data were analyzed using Microsoft Excel version 2007 and SPSS 14.0 computer software.
Results:
The incidence of rupture of the gravid uterus was 1:258 deliveries. In patients with rupture of the gravid uterus, 65% (26) of patients were unbooked; 37.5% (15) were aged between 25 and 29 years. A total of 42.5% (17) of patients had secondary education and 21 (52.5%) were housewives. Rupture of a previous scar was the commonest etiologic factor accounting for 32.5% (11). The commonest presentation was abdominal pain in 92.5% of cases. Perinatal mortality and maternal mortality were 80% and 17.5% respectively.
Conclusion:
Rupture of the gravid uterus still remains a major cause of maternal mortality. Injudicious use of oxytocics should be discouraged in peripheral health facilities and reinforcement of the need for hospital based deliveries in patients with previous caesarean sections should also be intensified to improve outcome.
Keywords: Gravid uterus, rupture, UPTH, Nigeria
INTRODUCTION
Rupture of the pregnant uterus is a major contributor to the high maternal morbidity and mortality seen in developing countries.1–3 Regional variation occurs in the incidence of uterine rupture and is a reflection of the standard of obstetric care. Widespread poverty, low educational status, cultural constraints that underscore utilization of orthodox care, inadequate health facilities, poor transport system, poor communication facilities, and substandard health facilities are contributory factors in developing countries.2,4,5 It is therefore not surprising that most cases of ruptured uterus are in the unbooked patient1,5,6 This is different in developed countries where efficient antenatal and intrapartum care had almost eradicated this obstetric catastrophy.3,4,7
Most cases of uterine rupture in previous studies in this environment are due to rupture of the unscarred uterus secondary to neglected obstructed labor as against the backdrop of previous caesarean section scar rupture in developed countries.8–11
The magnitude of this preventable obstetric complication is enormous; thus it is imperative to evaluate periodically its impact and identify institutional problems that might compound its occurrence.
Various national studies have been done regarding uterine rupture1–3,5–7 but recent literature is replete in this region.
MATERIALS AND METHODS
A 5-year retrospective study of all cases of rupture of the gravid uterus between January 2004 and December 2007 was carried out. Records of the labor wards and theater were searched and the folder numbers of the patients with uterine rupture were retrieved. These numbers were used to get the folders of the patients from the archives of the hospital. The relevant information was extracted and placed on a spread sheet, namely sociodemographic variables, booking status, etiology of rupture, clinical presentation, points of referral, type of surgery done, sites of rupture, complications, fetal, and maternal outcome.
Analysis of data was done using appropriate computerized software packages (SPSS14 and Microsoft Excel 2007 version). Results were presented using percentages, tables, and charts.
RESULTS
From January 1, 2003 to December 31, 2007, there were a total of 10,337 deliveries of which 40 patients had rupture of the gravid uterus giving a ratio of 1: 258 deliveries.
The sociodemographic characteristics of patients are showed in Table 1, patients with uterine rupture, 15 (37.5%) patients were in the age group of 25-29 years, 13 (32.5%) patients were in the age group of 30-34 years, 7(17.5%) in the age group of 35-39 years while 1 (2.5%) in the age group of 40-44 years.
Table 1.
Socio-demographic characteristics
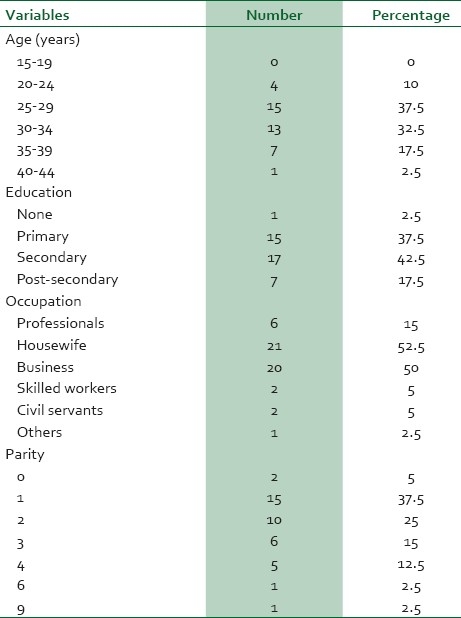
Secondary education was attained by 17 (42.5%) patients, 15 (37.5%) had primary education, 7 (17.5%) patients had tertiary education, and 1 (2.5%) had no formal education. Other sociodemographic variables are as shown in Table 1.
The booking status of patients indicated that 26 (65%) were unbooked as against 14 (35%) who are booked.
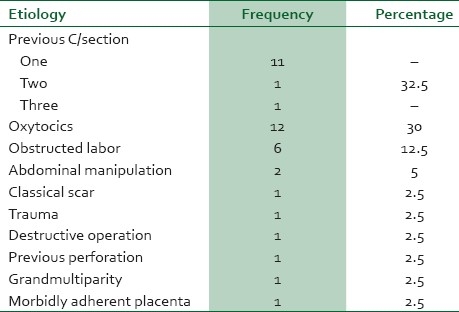
In patients with uterine rupture, 13 (32.5%) patients had previous lower segment caesarean section, 12 (30%) had background use of oxytocics, 6 (15%) had obstructed labor, 2 (5%) each had previous classical caesarean section, and manipulative operations done by traditional birth attendants to achieve vaginal delivery. Others are as shown in Table 2.
Table 2.
Etiologic factors for uterine rupture
The clinical presentation of patients with uterine rupture is illustrated in Table 3, 37 (92.5%) patients presented with abdominal pain, 26 (65%) had features of shock, vaginal bleeding occurred in 12 (30%) cases with 5 (12.5%) cases presenting with distorted uterine contour.
Table 3.
Clinical presentation of patients with rupture of the gravid uterus
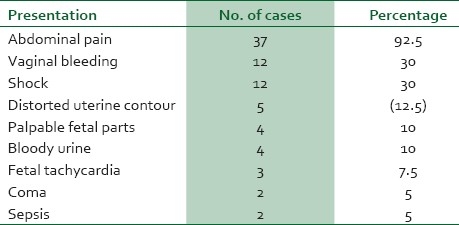
Figure 1 highlights the relationship between the first point of call and the booking status of patients, 14 patients that were booked in University of Port Harcourt Teaching Hospital (UPTH), 10 (71.43%) were first attended to at the UPTH while 2 (14.29%) presented to a private clinical before referral, 1 each (7.14%) first presented to the maternity, and health center respectively. Of the unbooked patients, 11 (42.31%) first presented at a maternity, 8 (30.76%) were first attended to at a private clinic, and 2 (7.69%) first presented at a traditional birth attendant's place, 1 (3.85%) each presented to a general hospital and health center respectively.
Figure 1.
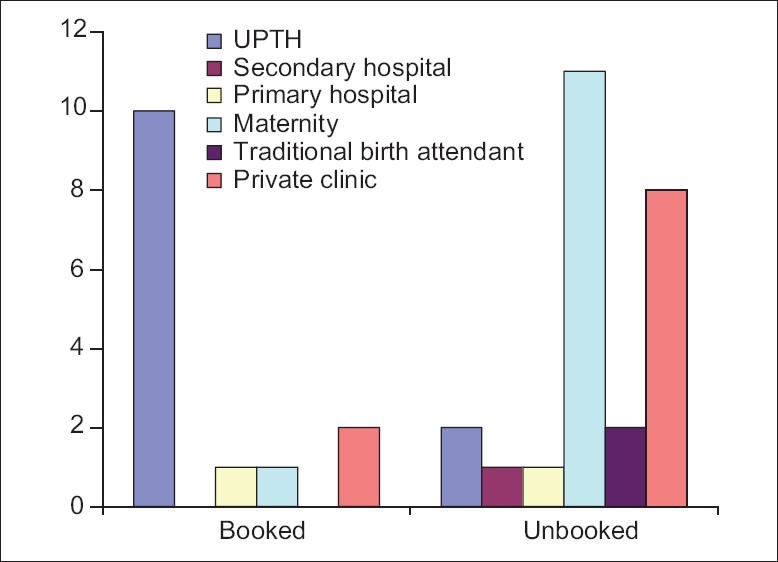
Booking status and first point of presentation at onset of labor
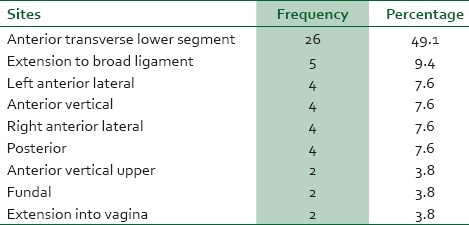
The various sites of rupture of the gravid uterus were as follows: anterior transverse lower segment rupture occurred in 26 (49.1%) cases. Five (9.4%) patients had extension into the broad ligament. Posterior, right anterior-lateral, left anterior-lateral, and anterior-vertical rupture had 4 (3.8%) cases each. Extension into the vagina and fundal ruptures occurred in two (3.8%) patients respectively Table 4.
Table 4.
Sites of rupture
The kind of surgeries performed: 42% had repair alone, 25% had repair and bilateral tubal ligation, 23% had total abdominal hysterectomy, and 10% had subtotal abdominal hysterectomy.
The fetal and maternal outcome in patients with rupture of the uterus is as follows: 33 (82.5%) mothers were alive while 7 (17.5%) died during and after surgery, 32 (80%) fetuses died while 8 (20%) of the fetuses were born alive.
The observed morbidities are as follows: 24 (42.1%) had anemia, 11 (19.3%) had puerperal sepsis, 8 (14%) had wound sepsis, and 7 (12.3%) with wound dehiscence. Two (3.5%) each vesico-vaginal fistulae and ureteric fistulae and one (1.75%) each had complications of renal failure, wound dehiscence, and subacute intestinal obstruction respectively.
DISCUSSION
The incidence of rupture of the gravid uterus is 1:258 deliveries. This incidence is similar to other series in Africa.2,5,12 Much higher incidence has been documented in other parts of Africa such as Uganda where values of 1:96 deliveries had been noted.13 Studies in Singapore noted lesser incidence of 1:6331 deliveries.14 The high incidence in some of these centers is not surprising because of the rapid deterioration in the quality of obstetric care offered to patients as a result of economic depression in most of these countries.15,16
The fact that, 65% of patients in this study were unbooked is a reflection of what is obtained in most developing countries as against that in developed countries where most patients had qualitative obstetric care.5,8,17–19
The age group largely affected by this obstetric catastrophic in this study were patients in their reproductive peak 25-29 years. This study however differs from that of Ezechi et al. who noted a high incidence amongst the age group 30-34 years and lowest amongst patients in the 25-29 years.2
Grandmultiparity, which had been identified by other studies as a high risk factor,20–22 was not observed in this study; instead primiparous patients were noted to have a higher incidence.
The attainment of at least a secondary school education was noted to encourage antenatal booking and hence reduce the risk of rupture whereas illiteracy encouraged nonantenatal clinic registration and likelihood of unsupervised deliveries and higher rate of uterine rupture.19,23 In this study, most patients had at least a secondary education; this did not however, translate to a reduction in the rate of rupture of the gravid uterus amongst them. This may bring to question the quality of education received by these patients. In addition, these patients though having secondary education may not had been financially empowered to seek qualitative care since most were housewives.
The rupture of the unscarred uterus had been well documented as common in developing countries.1,3 This study however identified rupture to be more in patients with previously scarred uterus as had been noted in other studies.3,24–26
This can be attributed to increasing caesarean section rate in the country, aversion for a repeat caesarean section by most women in Nigeria and the tendency to seek unskilled intervention in the event of another pregnancy, falsely assuming that the reason for the initial caesarean section was that they presented to a health facility.27–30
In addition, injudicious use of oxytocics was also noted to be contributory to rupture of the gravid uterus especially in patients with previous caesareans section. This etiological base was also brought into focus by various studies.2,8,31 Most unbooked patients presented at maternities run by unskilled personnel with little or no knowledge of basic obstetric care and also private clinics that use oxytocics on patients with previous caesarean section scar without adequate monitoring of these patients in labor. The points of referral had been implicated, with increased incidence of rupture amongst maternities run by Christian missions and the health centers run by the community health workers without adequate knowledge of the use of oxytocics.2
The commonest site of rupture was the anterior lower segment as had been observed in other studies.8,18,20 The repair of rupture site was the commonest procedure offered patients and this may not be unconnected to the fact that most ruptures occur over the previous caesarean section scar and during the call periods were only residents were present to handle the cases. This particular measure of repair alone puts the patients at higher reproductive risk if they fail to present themselves for supervised delivery at a centre where surgical intervention is possible.
The perinatal and maternal mortalities of 17.5% and 80%, respectively, depict the grave nature of the problem. These figures are similar to findings in most of the series12,17,20,31 but higher than those of Lema and Chen.24,32 The variations signify the quality of obstetric care in the areas reviewed. Morbidities such as anemia, puerperal sepsis, and prolonged hospital stay are corroborated by similar finding in Ibadan, Sagamu, and Ethopia.6,12,17
CONCLUSION
It is obvious that rupture of the gravid uterus still constitutes a major obstetric complication in this environment. Thus concreted efforts need to be made to improve utilization of health facilities, by increasing socioeconomic status of woman, easy access to emergency obstetrics care, improving the communication and transport systems. There is also need for proper education of females about the associated risk after a previous caesarean section if pregnancy and labor is unsupervised in the next confinement. In addition, regulation of the injudicious use of oxytocics by unskilled personnel is advocated with increased vigilance among skilled personnel during the use of oxytocics in patients with previous caesarean section scars.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Falaemu DL, Ogunniyi SO, Makinde OO. Rupture of the gravid uterus in Ile-Ife, Nigeria. Trop Doct. 1990;20:188–9. doi: 10.1177/004947559002000425. [DOI] [PubMed] [Google Scholar]
- 2.Ezechi OO, Mabayoje P, Obissie LO. Rupture uterus in Southern Western Nigeria: A reappraisal. Singapore Med J. 2004;45:113–6. [PubMed] [Google Scholar]
- 3.Aboyegi AP. Rupture uterus in Illorin, Nigeria: A 5-years Review. Niger Med Pract. 1997;33:5–8. [Google Scholar]
- 4.Kafkes S, Tanner CE. Rupture uterus. Int J Gynaecol Obstet. 1990;34:41–4. doi: 10.1016/0020-7292(91)90536-e. [DOI] [PubMed] [Google Scholar]
- 5.Konje JC, Odukoya OA, Ladipo OA. Ruptured uterus in Ibadan-a twelve year review. Int J Gynaecol Obstet. 1990;32:207–13. doi: 10.1016/0020-7292(90)90347-n. [DOI] [PubMed] [Google Scholar]
- 6.Okanlawon LO, Peter A, Olubi O, Peter O, Olufemi AO, Tuminu AF, et al. Uterine rupture a major contributor to obstetrics morbidity in Sagamu. Trop J Obstet Gynecol. 2003;20:137–40. [Google Scholar]
- 7.Oronsaye OA, Asuquo EE. Rupture uterus in Nigeria Hospital. Singapore J Obstet Gynaecol. 1990;11:34–8. [Google Scholar]
- 8.Ola ER, Olamijulo JA. Rupture at the Lagos University Teaching Hospital, Lagos, Nigeria. West Afr J Med. 1998;17:188–93. [PubMed] [Google Scholar]
- 9.Iloki LH, Okongo D, Ekoundzola JR. [Uterine rupture in an African environment.59 cases at the University Hospital Center in Brazzaville] J Gynaecol Obstet Biol Reprod (Paris) 1994;23:922–5. [PubMed] [Google Scholar]
- 10.Edward HP, Benjamin PS. High Risk Pregnancy Management options. Philadelphia: W.B. Saunders; 2000. Post–partum haemorrhage and other problems of the third stage; pp. 1231–46. [Google Scholar]
- 11.Padyne SM. Rupture of the pregnant uterus-a 20 year review. Kathamandu Univ Med J (KUMJ) 2005;3:234–8. [PubMed] [Google Scholar]
- 12.Gessssew A, Mengiste MM. Rupture uterus.A eight year retrospective analysis of causes and management outcome in Adrigrat Hospital, Tigray Region, Ethiopia. Ethiop J Health Dev. 2002;16:241–5. [Google Scholar]
- 13.Onwudiegwu U, Okonofua FE, Omole-Ohonsi A. Rupture of the gravid uterus following a road traffic accident. Int J Gynecol Obstet. 1990;33:273–4. doi: 10.1016/0020-7292(90)90014-c. [DOI] [PubMed] [Google Scholar]
- 14.Chen LH, Tain KH, Yeo GS. A ten-year review of uterine rupture in modern obstetric practice. Ann Acad Med Singapore. 1995;24:830–5. [PubMed] [Google Scholar]
- 15.Ezechi OC, Fasubaa OB, Dare FO. Socioeconomic barriers to safe motherhood among booked patients in rural Nigerian communities. J Obstet Gynaecol. 2000;20:32–4. doi: 10.1080/01443610063426. [DOI] [PubMed] [Google Scholar]
- 16.Onwudiegwu U. The effect of a depressed economy in the utilization of maternal health services.The Nigerian experience II. J Obstet Gynaecol. 1997;17:143–8. doi: 10.1080/01443619750113672. [DOI] [PubMed] [Google Scholar]
- 17.Ogunowo T, Olayemi O, Aimakhu CO. Uterine rupture: UCH, Ibadan experience. West Afr J Med. 2003;22:236–9. doi: 10.4314/wajm.v22i3.27957. [DOI] [PubMed] [Google Scholar]
- 18.Nkata M. Rupture of the uterus: A review of 32 cases in a general hospital in Zambia. BMJ. 1996;312:1204–5. doi: 10.1136/bmj.312.7040.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ekele BA, Audu LR, Muyibi S. Uterine rupture in Sokoto, Northern Nigeria-are we winning? Afr J Med Med Sci. 2000;29:191–3. [PubMed] [Google Scholar]
- 20.Aboyeji AP, Iyaiya MD, Yahaya RU. Rupture uterine: A study of 100 consecutive cases IIlorin Nigeria. J Obstet Gynecol Res. 2001;27:341–8. doi: 10.1111/j.1447-0756.2001.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 21.Okogbenin SA, Gharoro EP, Otoide VO, Okonta PI. Obstetric hysterectomy: Fifteen years’ experience in a Nigerian tertiary centre. J Obstet Gynaecol. 2003;23:356–9. doi: 10.1080/0144361031000119475. [DOI] [PubMed] [Google Scholar]
- 22.Olatunji AO, Sule-Odu AO, Adefuye PO. Rupture uterus in Sagamu, Nigeria. Niger Postgrad Med J. 2002;9:235–9. [PubMed] [Google Scholar]
- 23.Harrison KA. Maternal mortality-a sharper focus on a major issue of our time. Trop Obstet Gynaecol. 1988;1:9–13. [PubMed] [Google Scholar]
- 24.Campbell S, lee C, editors. Obstetrics by ten Teachers. 11th ed. London UK: Arnold Publishers; 2000. Operative intervention in Obstetrics; pp. 299–300. [Google Scholar]
- 25.Johnson R. Obstetrics procedures. In: Edmond DK, editor. Dewhurst's Textbook of Obstetrics and Gynaecology for Postgraduates. 6th ed. Oxford UK: Blackwell Scientific Publishers; 1999. pp. 308–29. [Google Scholar]
- 26.Ezegwui HU, Nwogu-Ikoju EE. Trends in uterine rupture in Enugu, Nigeria. J Obstet Gynaecol. 2005;25:260–2. doi: 10.1080/01443610500060768. [DOI] [PubMed] [Google Scholar]
- 27.Oladapo OT, Sotunsa JO, Sule-Odu AO. The rise in caesarean birth rate in Sagamu, Nigeria: Reflection of changes in obstetric practice. J Obstet Gynaecol. 2004;24:377–81. doi: 10.1080/01443610410001685484. [DOI] [PubMed] [Google Scholar]
- 28.Ado DG, Bala MA, Bello MK. Rising trends and indication of caesarean section at the University of Maiduguri teaching hospital, Nigeria. Niger Med J. 2009;50:64–7. [Google Scholar]
- 29.Ikeako IC, Nwajiaku I, Ezegwui HU. Caesarean section in a secondary health hospital in Akwa.Nigeria. Niger Med J. 2009;50:64–7. [Google Scholar]
- 30.Abubakar RD, Lyaiya MA, Aboyeji AP. Uterine rupture. Postgrad Doct Caribb. 2003;20:89–91. [Google Scholar]
- 31.Elkady AA, Bayomy HM, Bekhiet MT, Najib HS, Waliba AK. A review of 126 cases of ruptured gravid uterus. Int Surg. 1993;78:231–5. [PubMed] [Google Scholar]
- 32.Lema VC, Ojwang SB, Wanjala SH. Rupture of the gravid uterus: A Review. East Afr Med J. 1991;68:430–41. [PubMed] [Google Scholar]


