Summary
We describe a rare case of mandibular high-flow arteriovenous malformation (AVM) mimicking an odontogenic cyst in a young man.
The diagnosis of mandibular AVM was made by CT angiography and confirmed by digital subtraction angiography. CT scan showed the extent of mandibular bone alteration and a double enlarged mandibular canal on the same side. An AVM containing a large aneurysm was demonstrated by CT angiography. The mandibular AVM was successfully treated by endovascular therapy with Guglielmi detachable coils.
On panoramic radiogram, mandibular AVMs can appear as cystic lesions without pathognomonic features. Several benign and malignant tumours of this anatomical region must be considered in the differential diagnosis. We emphasize the radiological sign of double enlarged mandibular canal and the diagnostic role of CT, particularly CT angiography, to discriminate a mandibular AVM from neoplastic entities of this region, sparing the risks of a needle biopsy.
Key words: AV fistula, mandible, odontogenic cyst
Introduction
Arteriovenous malformations (AVMs) involving the mandibular bone and the dental arcade are considered rare entities, representing about 5% of all vascular malformations1.
Mandibular AVMs are usually of arterial type with high flow and potentially fatal because of frequent copious bleeding 1.
Traditional treatment includes surgical resection with mandibular reconstruction. Conservative treatments are direct injection therapy and endovascular embolization.
Case Report
A 23-year-old man with a history of blunt trauma (martial arts) was referred to the maxillofacial surgery department of our hospital with a previous diagnosis of odontogenic cyst of the mandible. The patient reported paresthesia of the lower lip for the last six months.
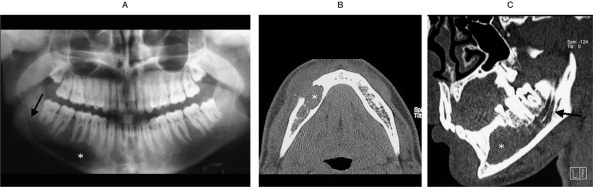
A panoramic radiograph disclosed a lytic lesion with benign radiological features in the right mandibular body, next to 4.4, 4.5 and 4.6 teeth roots. (figure 1A). These teeth had been endodontically treated by a dentist because of trauma to the teeth roots during surgery.
Figure 1.
Panoramic radiograph (A), axial (B) and parasagittal (C) CT scan with bone algorithm. "Benign" lytic lesion in the right mandibular body (asterisk);double mandibular channel on the same side (arrow).
An intraoral incision was made in the 4.4-4.7 region. The vestibular mucosa was unstuck and the intraosseous lesion exposed. The malformation showed a vascular-like consistency. It was throbbing and easily removable from the bone. In the light of the intra-operative finding, the surgical procedure was interrupted.
A 16-row multidetector CT scan confirmed the extent of bone alteration in the right hemimandible and showed a double, enlarged mandibular channel on the same side (figure1 B,C).
CT angiography was performed and processed with maximum intensity projection (MIP) and the volume rendering technique (VRT).
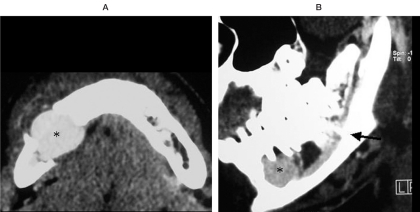
An aneurysmal dilatation of a vessel was demonstrated within the bone lesion (figures 2 and 3). A diagnosis of mandibular AVM was made and the patient underwent digital subtraction angiography.
Figure 2.
CT angiography axial (A) and parasagittal (B) images. Aneurysmal dilatation of a vessel is visible within the mandibular bone lesion (asterisks). An enlarged inferior alveolar artery and vein are also visible within the mandibular channel (arrow).
Figure 3.
CT angiography parasagittal VRT images (A,B) allow a three-dimensional, concomitant evaluation of both vascular and osseous alterations.
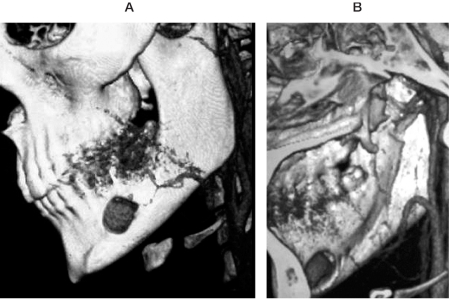
Angiographic evaluation of the right external carotid artery was carried out by transfemoral catheterism. A venous aneurysm with a diameter of 2 cm was demonstrated within the bone lesion (figure 4). The aneurysm was the enlarged venous drainage of an arteriovenous fistula supplied by the inferior alveolar artery, a branch of internal maxillary artery. Moreover, the fistula was supplied by two terminal branches of the submental artery, anastomosed with the mental artery (figure 5).
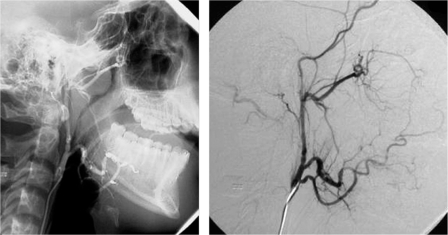
Figure 4.
Digital subtraction angiography. A) Selective catheterization of the external carotid artery common trunk shows the arteriovenous malformation supplied by a split inferior alveolar artery. A 2 cm venous aneurysm is visible (asterisk). B) Superselective angiography of the inferior alveolar artery better shows the venous aneurysm (asterisk).
Figure 5.
Angiographic evaluation of the arterial supply through the inferior alveolar artery after releasing platinum GDC coils (arrow).
Super-selective catheterization and embolization of feeding arteries was successfully performed with Guglielmi detachable coils (GDC) (figures 6 and 7).
Figure 6.
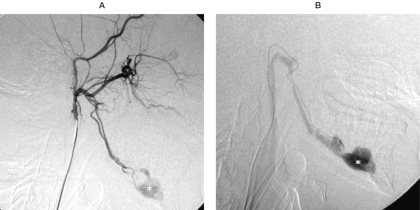
Angiographic evaluation of the facial artery. Another arterial supply to the arteriovenous malformation is visible by retrograde flow from two terminal branches of the submental artery, anastomosed with the mental artery (arrow).
Figure 7.
Post-embolization angiographic evaluation of alveolar and submental arteries by external carotid common trunk catheterization. The AV malformation is completely occluded.
CT angiography performed six months after endovascular treatment showed a complete disappareance of the arteriovenous fistula.
Discussion
Mandibular AVMs are rare conditions that could be fatal if left untreated as the result of massive blood loss after tooth extraction or attempts to remove or biopsy the lesion1-4. Mandibular AVMs can be acquired or congenital. The acquired forms are usually caused by a deep penetrating trauma involving any area of the jaw and affecting different ages 1-3.
The congenital forms occur as a result of error in vascular morphogenesis. This type of mandibular AVMs can be present at birth and enlarge with physical growth. This overgrowth is connected to hormonal factors, vasomotor disturbances or trauma. Most commonly, they occur in the second decade of life and involve the molar region 2-4. Some authors have noted a predominance in women (2:1), while others have reported no sex prevalence 5.
Mandibular AVMs may be asymptomatic or show various signs and symptoms including bruit, dental loosening, erythematous and bleeding gingiva, swelling of the soft tissues of the face and dysesthesia of the lower lip or chin due to sensorial fifth nerve irritation3.
Radiological diagnosis of mandibular bone pathologies is traditionally committed to panoramic radiography. Mandibular AVMs can appear as cystic lesions without pathognomonic features. However, evidence of an expanded (greater than 6 mm in diameter) or double mandibular channel on the same side as the lesion suggests a mandibular AVM. Bone expansion is probably due to intraosseous dilatation of the inferior alveolar artery and vein2-4.
This essential radiological sign can be observed on panoramic radiography and, better, a CT scan. A double mandibular canal in the absence of a lacunar osteolysis is not clearly indicative of pathology, but an expression of an normal anatomical variation5.
The role of CT in the diagnosis of a mandibular AVM has been greatly improved by the introduction of CT angiography. CT is the gold standard for detection of lytic changes in mandibular bone and the alteration of mandibular channel. Moreover, CT angiography will safely disclose vessels within the bone, discriminating a mandibular AVM from neoplastic entities of this region, sparing the risks of a needle biopsy.
Digital Subtraction Angiography is irreplaceable for a precise definition of a mandibular AVM. This technique accurately defines the vascular architecture of the lesion, particularly the number of feeding vessels from the ipsi- and contralateral facial, lingual and maxillary arteries. This vascular map is essential for planning surgical or endovascular procedures.
Mandibular AVMs have traditionally been treated by surgery. Surgical treatment requires extensive bone resection with complex reconstruction to maintain the mandibular functions and prevent disfigurement6,7,13.
Endovascular treatment of mandibular AVMs can be carried out by transfemoral catheterization or by direct puncture8,9,10,11,12,14,15.
Either technique can be performed as a preliminary adjunct to excision and reconstructive surgery or as the sole definitive approach. In our case, endovascular treatment was preferred because the lesion was an arteriovenous fistula without an arteriovenular nidus: complete and durable treatment is difficult when a nidus is present8,9,10,11,12,14,15.
In conclusion, we suggest the use of CT angiography in case of a well-circumscribed lytic lesion of the mandible combined with a double enlarged mandibular canal. Mistaking an arteriovenous malformation for a simple odontogenic cyst is very dangerous for the patient.
References
- 1.Lasjaunias P, Berenstein A. Surgical Neuro-angiography. vol 2. Berlin Heidelberg: Springer-Verlag; 1987. Chapter 10 - Craniofacial hemangioma, vascular malformations and angiomatosis: specific aspects; pp. 341–397. [Google Scholar]
- 2.Scholl RJ, Kellett HM, et al. Cysts and cystic lesions of the mandible: clinical and radiologic-histopathologic review. Radiographics. 1999;19:1107–1124. doi: 10.1148/radiographics.19.5.g99se021107. [DOI] [PubMed] [Google Scholar]
- 3.Fan X, Qiu W, et al. Comparative study of clinical manifestations, plain-film radiography, and computed tomographic scan in arteriovenous malformations of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:503–509. doi: 10.1067/moe.2002.126910. [DOI] [PubMed] [Google Scholar]
- 4.Mohammadi H, Said-Al-Naief N, Heffez LB. Arteriovenous malformation of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:286–289. doi: 10.1016/s1079-2104(97)90344-9. [DOI] [PubMed] [Google Scholar]
- 5.Rouas P, Nancy J, Bar D. Identification of double mandibular canals: literature review and three case reports with CT-scans and cone beam CT. Dentomaxillofacial Radiology. 2007;36:34–38. doi: 10.1259/dmfr/27374727. [DOI] [PubMed] [Google Scholar]
- 6.Noreau G, Landry PP, Morais D. Arteriovenous malformation of the mandible: review of literature and case history. J Can Dent Assoc. 2001;67(11):646–651. [PubMed] [Google Scholar]
- 7.Motamedi MH, Behnia H, Motamedi MR. Surgical technique for the treatment of high-flow arteriovenous malformations of the mandible. Journal of Craniomaxillofacial Surgery. 2000;28:238–242. doi: 10.1054/jcms.2000.0139. [DOI] [PubMed] [Google Scholar]
- 8.Benndorf G, Campi A, et al. Endovascular management of a bleeding mandibular arteriovenous malformation by transfemoral venous embolization with NBCA. American Journal of Neuroradiology. 2001;22:359–362. [PMC free article] [PubMed] [Google Scholar]
- 9.Siu WW, Weill A, et al. Arteriovenous malformation of the mandible: embolization and direct injection therapy. Journal of Vascular and Interventional Radiology. 2001;12:1095–1098. doi: 10.1016/s1051-0443(07)61597-8. [DOI] [PubMed] [Google Scholar]
- 10.Fathi M, Manafi A, et al. Large arteriovenous high-flow mandibular malformation with exsanguinating dental socket haemorrhage: a case report. Journal of Cranio-Maxillofacial Surgery. 1997;25:228–231. doi: 10.1016/s1010-5182(97)80080-7. [DOI] [PubMed] [Google Scholar]
- 11.Fan X, Zhang Z, et al. Direct-puncture embolization of intraosseous arteriovenous malformation of jaws. J Oral Maxillofac Surg. 2002;60:890–896. doi: 10.1053/joms.2002.33858. [DOI] [PubMed] [Google Scholar]
- 12.Brusati R, Galioto S, et al. Conservative treatment of arteriovenous malformations of the mandible. Int J Oral Maxillofac Surg. 2001;30:397–401. doi: 10.1054/ijom.2001.0120. [DOI] [PubMed] [Google Scholar]
- 13.Schneider C, Wagner A, Hollmann K. Treatment of intraosseous high flow arteriovenous malformation of the mandible by temporary segmental ostectomy for extracorporal tumour resection: a case report. Journal of Cranio-Maxillofacial Surgery. 1996;24:271–275. doi: 10.1016/s1010-5182(96)80057-6. [DOI] [PubMed] [Google Scholar]
- 14.Rodesch G, Soupre V, et al. Arteriovenous malformations of the dental arcades. The place of endovascular therapy: results in 12 cases are presented. Journal of Cranio-Maxillofacial Surgery. 1998;26:306–313. doi: 10.1016/s1010-5182(98)80059-0. [DOI] [PubMed] [Google Scholar]
- 15.Guibert-Tranier F, Piton J, et al. Vascular malformations of the mandible (intraosseous haemangiomas). The importance of preoperative embolization. A study of 9 cases. Europ J Radiol. 1982;2:257–272. [PubMed] [Google Scholar]