Abstract
OBJECTIVE
We evaluated whether cardiometabolic risk profiles differ for subjects identified as having prediabetes by A1C, fasting glucose (FPG), or 2-h postchallenge glucose (2-PG) criteria.
RESEARCH DESIGN AND METHODS
Atherosclerosis risk factors, oral glucose tolerance test, and ultrasound measurement of carotid intima–media thickness (IMT) were analyzed in 780 nondiabetic individuals.
RESULTS
Poor agreement existed for A1C and FPG criteria for identification of subjects with prediabetes (κ coefficient = 0.332). No differences in cardiometabolic risk profiles were observed among the three groups of individuals with prediabetes by A1C only, FPG only, and both A1C and FPG. Poor agreement also existed for A1C and 2-PG criteria for identification of individuals with prediabetes (κ coefficient = 0.299). No significant differences in cardiometabolic risk factors were observed between IGT-only and individuals with prediabetes by A1C and 2-PG. Compared with subjects with prediabetes identified by A1C only, IGT-only individuals exhibited a worse cardiometabolic risk profile, with significantly higher systolic blood pressure, pulse pressure, 2-h postchallenge insulin, triglycerides, high-sensitivity C-reactive protein, and carotid IMT, and lower HDL cholesterol levels and insulin sensitivity.
CONCLUSIONS
These results suggest that considerable discordance between A1C, FPG, and 2-PG exists for the identification of individuals with prediabetes and that the cardiometabolic risk profile of these individuals varies by metabolic parameter, with 2-PG showing the stronger association with cardiometabolic risk factors and subclinical atherosclerosis than FPG or A1C.
Hemoglobin A1c (A1C) is an integrated measure of average blood glucose concentrations over the preceding 2–3 months and is widely used for monitoring metabolic control in individuals with diabetes (1). Recently, the American Diabetes Association (ADA) has revised criteria for the diagnosis of type 2 diabetes and the categories at increased risk for diabetes already including impaired fasting glucose (IFG) and impaired glucose tolerance (IGT) on the basis of an ample analysis performed by an international expert committee (2,3) recommending the use of A1C measurements as another diagnostic test option in addition to glucose values. Specifically for the categories of increased risk for type 2 diabetes, the new ADA recommendations state that an A1C from 5.7 to 6.4% identifies individuals at high risk for diabetes to whom the term prediabetes may be applied (2).
A1C measurements offer some practical advantages over assessments of fasting plasma glucose (FPG) or glucose levels during an oral glucose tolerance test (OGTT), including lower day-to-day variability, less perturbations during periods of stress or illness, and requirement of a nonfasting sample (3). However, the A1C measure may identify distinct subjects at increased risk for type 2 diabetes compared with IFG and IGT, and if extensively implemented, may to some extent change the present epidemiologic setting of these dysglycemic conditions. Although it would be desirable for fasting glucose, 2-h postchallenge glucose, and A1C values to be equivalent in identifying at-risk subjects, a poor concordance among the three prediabetes categories has been reported in different ethnic groups (4–10).
Early detection of individuals at high risk for type 2 diabetes is essential not only for prevention of diabetes itself but also of the associated cardiovascular complications. Indeed, the risk of cardiovascular disease is already increased before glucose levels reach the diagnostic threshold of diabetes, and 2-h postchallenge glucose has been reported to be a better predictor of cardiovascular disease than FPG (11,12). However, A1C was shown to be a better predictor of cardiovascular disease than FPG (13). Head-to-head comparisons between 2-h postchallenge glucose and A1C as predictors of cardiovascular disease have been focused on mortality, and results are controversial (14–16).
In consideration of the expected augmented use of A1C as a screening tool to identify individuals with dysglycemic conditions, it would be important to evaluate the effect of the new ADA recommendations for prediabetes definition on the ability to identify individuals who are at increased risk for a number of adverse clinical outcomes. In the current study, we examined the concordance of A1C, FPG, or 2-h postchallenge glucose tests for the identification of prediabetes in a cohort of Italian Caucasians. We also evaluated whether metabolic and cardiovascular risk factors, including carotid preclinical atherosclerosis, differ for subjects identified as having prediabetes by each of these criteria.
RESEARCH DESIGN AND METHODS
A total of 780 nondiabetic Caucasian subjects, consecutively recruited in the University of Rome and the University of Catanzaro areas, participated in this cross-sectional study for assessment of cardiometabolic risk factors according to a previously described protocol (17,18). The inclusion criteria were age ≥20 years, absence of diabetes mellitus, defined as A1C ≥6.5%, FPG ≥126 mg/dL, or 2-h postchallenge plasma glucose ≥200 mg/dL, and presence of one or more cardiometabolic risk factors, including elevated blood pressure (BP), dyslipidemia, overweight/obesity, and family history of diabetes. Subjects were excluded if they had gastrointestinal diseases associated with bleeding or malabsorption, chronic pancreatitis, history of any malignant disease, history of drug abuse, positivity for antibodies to hepatitis C virus or hepatitis B surface antigen, and anemia, defined according to the World Health Organization criteria as a hemoglobin concentration <13 g/dL in men and <12 g/dL in women.
After a 12-h fast, all subjects underwent an anthropometric evaluation, including assessment of BMI and waist circumference. Readings of clinic BP were obtained in the left arm of supine patients, after 5 minutes of quiet rest, with a mercury sphygmomanometer. Pulse pressure was calculated as the difference between systolic and diastolic BP. An OGTT was performed with sampling of plasma glucose at 0, 30, 60, 90, and 120 min for insulin determination.
Intima–media thickness (IMT) of the common carotid artery was measured by an ATL HDI 3000 ultrasound system (Advanced Technology Laboratories, Bothell, WA) equipped with a 5-MHz linear array transducer, as previously described (19). Manual measurements were conducted in plaque-free portions of the 10-mm linear segment proximal to the carotid bulb. Two measurements were performed bilaterally for each patient, and the values were averaged, which presented the mean of IMT of the common carotid artery. The ultrasound study was performed by an experienced examiner who was unaware of the subjects’ clinical and laboratory findings.
The individual 10-year risk of coronary heart disease (CHD) was estimated using the Framingham Heart Study prediction score sheet for 659 subjects in aged 30–74 years (20).
The protocol was approved by the institutional ethics committees and informed written consent was obtained from each participant in accordance with principles of the Declaration of Helsinki.
Analytic determinations
A1C was measured with high-performance liquid chromatography using a National Glycohemoglobin Standardization Program (NGSP) certified automated analyzer (Adams HA-8160 HbA1C analyzer, Menarini, Italy; normal reference range, 4.3–5.9%). Plasma insulin concentration was determined by a chemiluminescence-based assay (Immulite, Siemens, Italy). All others metabolites were measured by standard methods.
Statistical analysis
The Matsuda index of insulin sensitivity was calculated as reported (21). Variables with skewed distribution, including triglyceride, high-sensitive C-reactive protein (hs-CRP), and fasting and 2-h insulin, were log transformed for analyses. Continuous data are expressed as means ± SD. Categoric variables were compared by the χ2 test. Phenotypic differences between groups were tested after adjusting for age and sex using a general linear model with post hoc Bonferroni correction for multiple comparisons. The κ statistic was calculated as a measure of agreement between A1C and FPG or 2-h postchallenge diagnoses for individuals at high risk of type 2 diabetes. Partial correlation coefficients adjusted for age and sex were calculated between variables. Relationships between variables were sought by multivariate linear regression analysis to assess their independent contribution to IMT. All analyses were performed using SPSS 16.0 software (SPSS Inc, Chicago, IL).
RESULTS
The mean age of the whole study sample was 45 ± 13 years, 326 (41.8%) were men, and the mean BMI was 29.8 ± 6.8 kg/m2. According to ADA criteria (A1C 5.7–6.4%, IFG, or IGT), 421 of 780 subjects (53.9%) were at high risk for diabetes (prediabetes). The proportion of these subjects identified by A1C 5.7–6.4%, IFG, and IGT, was 31.5% (n = 245), 28.1% (n = 219), and 31.7% (n = 247), respectively.
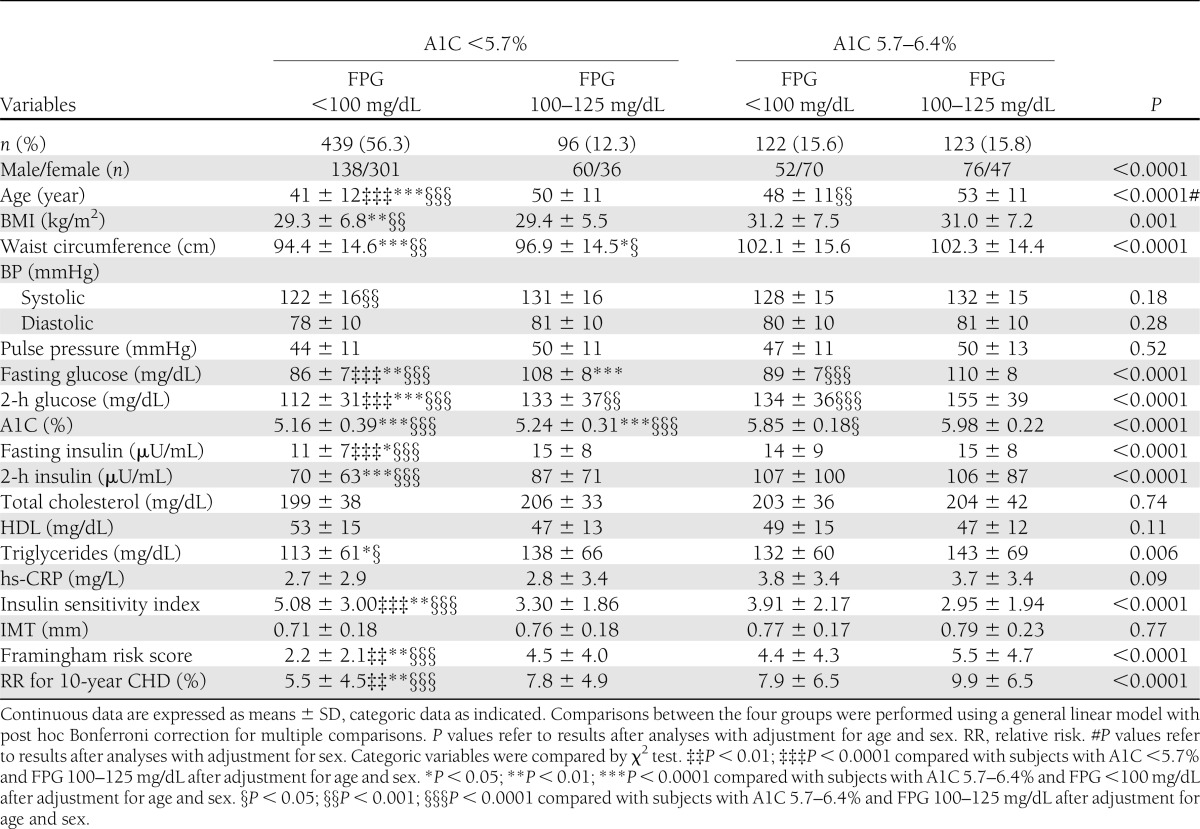
Fasting plasma glucose and A1C
Poor agreement existed for A1C and FPG criteria for identification of subjects with prediabetes (κ coefficient = 0.332), with 56.3% of individuals without prediabetes by both A1C and FPG criteria, and 15.8% classified as prediabetic by both A1C and FPG criteria (Table 1). Discordant classifications occurred for 12.3% of individuals who had an A1C <5.7% and IFG, and for 15.6% who had A1C 5.7–6.4% and FPG <100 mg/dL. Table 1 reports the clinical characteristics and laboratory findings of the four groups identified by FPG only, by A1C only, or by both criteria. The only differences in cardiometabolic risk profile observed among the three groups with prediabetes identified by A1C only, FPG only, and both A1C and FPG were waist circumference, which was higher in individuals with prediabetes identified by both A1C only and by FPG and A1C; FPG, which, by design, was lower in individuals with prediabetes identified by A1C only; A1C, which, by design, was lower in individuals with prediabetes identified by FPG only and both A1C and FPG; and 2-h postchallenge glucose, which was increased in individuals with prediabetes identified by both A1C and FPG.
Table 1.
Cardiometabolic characteristics of subjects with prediabetes defined by FPG only, by A1C only, and by both FPG and A1C
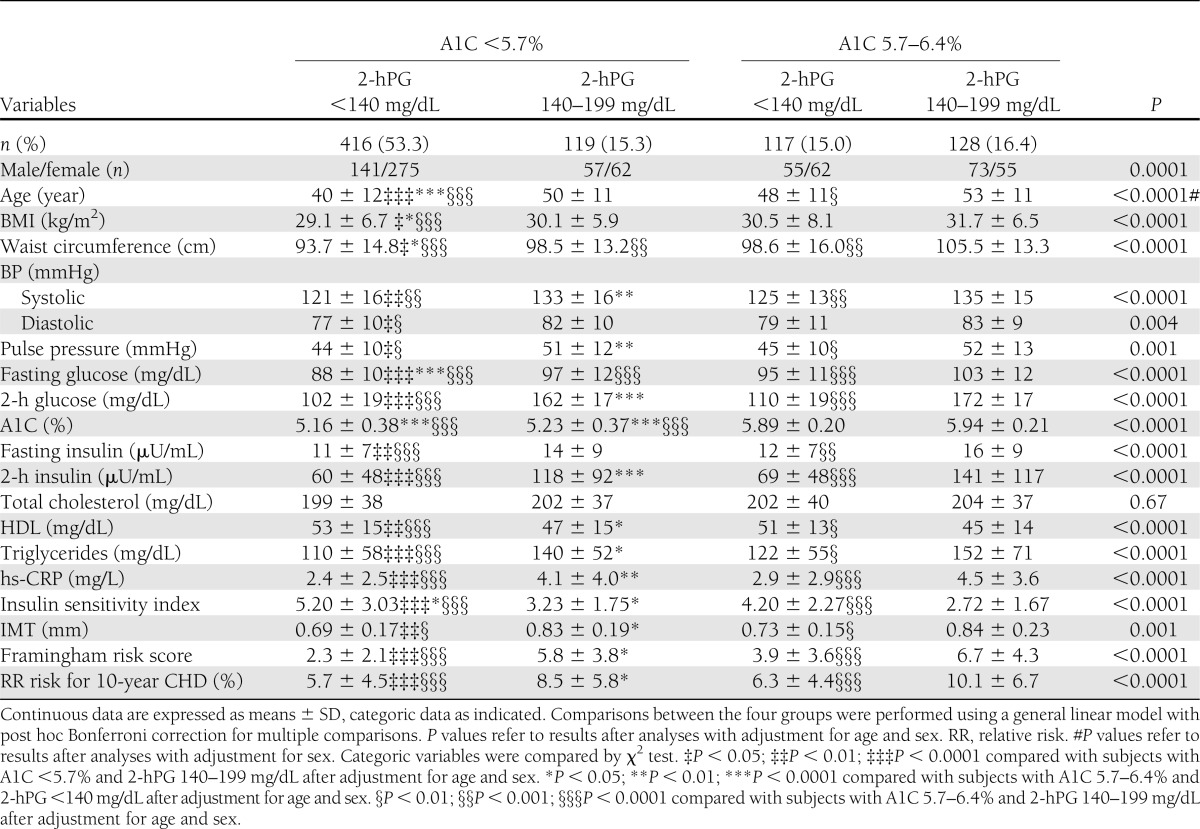
Agreement for 2-h postchallenge glucose and A1C
Poor agreement existed for A1C and 2-h postchallenge glucose criteria for identification of individuals with prediabetes (κ coefficient = 0.299), with 53.3% of individuals not having prediabetes by both A1C and 2-h postchallenge glucose criteria and 16.4% classified as having prediabetes by both A1C and 2-h postchallenge glucose criteria (Table 2). Discordant classifications occurred for 15.3% of individuals who had an A1C <5.7% and IGT and for 15.0% who had an A1C 5.7–6.4% and 2-h postchallenge glucose <140 mg/dL (Table 2).
Table 2.
Cardiometabolic characteristics of subjects with prediabetes defined by 2-h postchallenge glucose (2-hPG) only, by A1C only, and by both 2-hPG and A1C
The worst cardiometabolic risk profile was observed in the two groups identified by 2-h postchallenge glucose criterion (Table 2). No significant differences in cardiometabolic risk factors were observed between IGT-only subjects and individuals with prediabetes by both A1C and 2-h postchallenge glucose, with the exception of waist circumference, and FPG, which were increased in the latter individuals.
Compared with subjects with prediabetes identified by A1C only, IGT-only individuals exhibited significantly higher systolic BP, pulse pressure, 2-h postchallenge insulin, triglycerides, hs-CRP, and carotid IMT, and lower HDL cholesterol levels and insulin sensitivity. These differences remained significant after adjusting for age and sex using a general linear model with post hoc Bonferroni correction for multiple comparisons. IGT-only individuals also exhibited a significantly higher Framingham risk score compared with subjects with prediabetes identified by A1C only.
No significant differences in cardiometabolic risk factors were observed between normal individuals and subjects with prediabetes identified by A1C only, with the exception of age, BMI, waist circumference, and FPG, which were significantly increased in the latter individuals.
In univariate analyses adjusted for sex and age, carotid IMT was significantly correlated with waist circumference, systolic and diastolic BP, and 2-h postchallenge glucose (Supplementary Table 1). Of the three glycemic parameters, 2-h postchallenge glucose only was significantly correlated with carotid IMT.
To estimate the independent contribution of A1C, FPG, or 2-h postchallenge plasma glucose to carotid IMT, we conducted a multivariate regression analysis in a model also including age, sex, and components of the metabolic syndrome (i.e., waist circumference, systolic and diastolic blood pressure, triglycerides, and HDL cholesterol). The two variables that remained significantly associated with carotid IMT were age (β = 0.223; P < 0.0001), and 2-h postchallenge plasma glucose (β = 0.199; P < 0.0001), accounting for 18.1% of its variation.
CONCLUSIONS
Increasing evidence suggests a low agreement between a prediabetes diagnosis made by A1C and one obtained using FPG and 2-h postchallenge criteria (4–10). As pointed out by the ADA, the characterization of subjects discordantly categorized by the three tests is now pending (2). In the current study, we show that different subjects are identified as having prediabetes using the three glucose tests, demonstrating for the first time that individuals with prediabetes identified by the 2-h postchallenge glucose criterion have a worse cardiovascular risk profile that is not explained by the other features of the metabolic syndrome concurrently observed in these subjects.
In our cohort of adult Italian Caucasians, there was low agreement between the diagnosis of high risk for type 2 diabetes (prediabetes) made by A1C and FPG or 2-h postchallenge ADA criteria. We observed that 55.1% of the individuals with A1C 5.7–6.4% were not classified as being at high risk by FPG criterion and that 46.4% of the individuals at high risk by FPG criterion would be classified as not being at high risk by A1C criterion. Using 2-h postchallenge glucose as the criterion, 49.7% of the individuals with A1C 5.7–6.4% were not classified as being at high risk by 2-h postchallenge glucose, and 52.3% of the individuals at high risk by 2-h postchallenge glucose would be classified as not being at high risk by the A1C criterion.
The present results are in agreement with those recently reported in studies of adults from the U.S. National Health and Nutrition Examination Survey (NHANES) (4,6,7), from the Screening for Impaired glucose tolerance (SIGT) study (6), from the Insulin Resistance Atherosclerosis Study (IRAS) (8), from a cohort of Asian Indians (5), and from a cohort of Arab ancestry (10). Higher A1C levels at any given level of FPG have been reported in Hispanics, American Indians, Blacks, and Asian Americans compared with their Caucasian counterparts, even after adjustment for confounding factors affecting glycemia (22). These disparities are likely due to differences in hemoglobin glycation or erythrocyte turnover among ethnic groups. Because previous studies have included cohorts of different ethnicities, the current results, which are based only on a cohort of Caucasian individuals, provides important information to help clinicians and patients of European ancestry understand the advantages and shortcomings of each test used alone or in combination. Notably, multiple nonglucose factors, such as hemoglobinopathies and anemia, can influence the accuracy of A1C measurement. Although individuals with undiagnosed anemia might possibly have been included in previous studies comparing the concordance of A1C, FPG, or 2-h postchallenge glucose tests for the identification of prediabetes, in the current study, we excluded individuals with conditions that affect red cell turnover, such as anemia and major blood loss, thus increasing the accuracy in the A1C measurement of the present results.
The discordance in the identification of individuals at high risk for type 2 diabetes using different metabolic parameters is not entirely unexpected given that measurements of FPG, 2-h postchallenge glucose, and A1C are likely to reflect different aspects of glucose metabolism, and a diagnosis of prediabetes based on IFG, IGT, and A1C highlights the different pathophysiologic mechanisms underlying abnormal glucose homeostasis (23). In fact, IFG is characterized by a combination of hepatic insulin resistance and defective early-phase insulin secretion resulting in excessive fasting hepatic glucose production that accounts for fasting hyperglycemia. By contrast, IGT is characterized by nearly normal hepatic insulin sensitivity and marked muscle insulin resistance combined with defective late insulin secretion thus resulting in prolonged hyperglycemia after a glucose load (23). In contrast to the daily glucose picture offered by IFG and IGT, A1C is an indicator of the average blood glucose concentrations over the preceding 2–3 months, accounting for chronic exposure to both basal and postprandial hyperglycemia and, therefore, may reflect a combination of pathophysiologic defects underlying both IFG and IGT. Taken together, the different pathophysiologic mechanisms underlying each glycemic marker help explain the discordant diagnoses of prediabetes based on FPG, 2-h postchallenge glucose, and A1C. However, it is likely that as overt diabetes develops, each underlying mechanism is active, which may help explain the fair concordance between FPG, 2-h postchallenge, and A1C tests to diagnose diabetes (24–27).
A central question is whether individuals with prediabetes diagnosed by FPG, 2-h postchallenge glucose, and A1C are at equivalent risk of cardiovascular disease. Elevation in plasma glucose at the prediabetic levels has been shown to be associated with increased risk of subsequent cardiovascular disease (28,29). Longitudinal data on cardiovascular risk comparing FPG, 2-h postchallenge glucose, and A1C in the prediabetic range are sparse, have been focused on mortality, and have reached controversial results (11–15). In this study, we observed no differences in cardiometabolic risk profile among the three groups with prediabetes diagnosed by FPG only, A1C only, and both A1C and FPG. By contrast, compared with individuals with prediabetes by A1C only, prediabetic individuals identified by 2-h postchallenge glucose (IGT only and combined IGT/A1C) had a worse cardiovascular risk profile, resulting in a higher Framingham score for 10-year CHD risk and subclinical atherosclerosis as determined by IMT. The latter differences remained significant after adjusting for age and sex using a general linear model with the conservative post hoc Bonferroni correction for multiple comparisons.
To the best of our knowledge, this is the first study comparing the effect of the recently proposed ADA criteria of elevated A1C (5.7–6.4%) with both FPG and 2-h postchallenge glucose on subclinical atherosclerosis, a well-validated proxy of cardiovascular disease. Notably, we observed that the 2-h postchallenge glucose value showed a stronger correlation with IMT than FPG or A1C, and was the only glycemic parameter independently associated with IMT in a multivariate regression analysis in a model including components of metabolic syndrome. The present data are in agreement with those of a prospective population-based study showing that the 2-h postchallenge glucose, at variance with FPG and A1C, was the only glycemic marker in the prediabetic range significantly associated with incident cardiovascular disease in women (30). It is important to note that only subjects who converted from IFG to diabetes (31) or from A1C of 5.7–6.4% to A1C ≥6.5% have an increased risk for cardiovascular disease. By contrast, IGT individuals are at increased risk for cardiovascular disease independently of the conversion to diabetes (31).
Taken together with the present findings showing that IGT-only individuals have signs of early atherosclerosis independently from elevated A1C, we can suggest that additional information on cardiovascular disease risk, that may be clinically useful for the identification of subjects at increased risk, is embedded in the 2-h postchallenge glucose level. These findings showing a link between postchallenge hyperglycemia and cardiovascular risk may have clinical implications. Because lifestyle changes and pharmacologic interventions in individuals at high-risk for type 2 diabetes have been consistently demonstrated to be successful in reducing the incidence of the disease and its associated cardiovascular complications (32,33), it would be important to identify individuals at increased risk for both clinical outcomes, such as those with IGT, who could benefit from lifestyle change interventions, and, possibly, pharmacotherapy.
The mechanism by which elevated 2-h postchallenge glucose levels are associated with an increased risk of atherosclerosis is not settled. A greater degree of insulin resistance in IGT individuals is one possibility accounting for development of atherosclerosis. Accordingly, we observed that prediabetic individuals identified by 2-h postchallenge glucose (IGT only and combined IGT/A1C) had lower insulin sensitivity than normal individuals and prediabetic individuals identified by A1C only. In addition, chronic subclinical inflammation could be a unifying mechanistic factor because it predicts the development of both type 2 diabetes (34) and cardiovascular disease (35). Among markers of subclinical inflammation, the most reliable for clinical use is hs-CRP. We found that IGT-only and combined IGT/A1C subjects had increased hs-CRP levels compared with normal individuals and prediabetic individuals identified by A1C only. Increased levels of hs-CRP may reflect systemic inflammation but may be also directly involved in the pathogenesis of both type 2 diabetes (36) and vascular atherosclerosis (37). Overall, these findings suggest a greater contribution of postprandial glucose to both insulin resistance and subclinical inflammation compared with A1C levels, thus reinforcing the idea that performing OGTT may be useful to identify individuals at high-risk for type 2 diabetes and cardiovascular complications.
The current study has several strengths, including the broad range of demographic, clinical, and biochemical data collected by trained staff following a standardized protocol, the centralization of laboratory analyses, the inclusion of well-validated risk factors for cardiovascular disease (lipids, blood pressure, insulin sensitivity, and hs-CRP), and the use of OGTT data instead of fasting glucose alone, as reported in other studies. Nevertheless, the current study needs to be interpreted in the context of certain potential limitations. A first limitation of our study is that each test (FPG, A1C, and OGTT) was only performed once. Although such an approach reflects clinical practice and is a common limitation to most large epidemiologic studies, the day-to-day variability of FPG and 2-h postchallenge glucose results cannot be taken into account in the current study.
A second limitation of the current study is the cross-sectional design, making causal interpretations of associations between diagnostic criteria and risk of cardiovascular disease difficult. Indeed, the current results reflect only an association with early atherosclerosis and not incident cardiovascular disease. Although carotid IMT is a well-established index of early atherosclerosis and is widely used as surrogate marker of cardiovascular disease, further prospective studies with incident cases of cardiovascular events are needed to draw such conclusions.
In conclusion, the results of the current study suggest that considerable discordance between A1C, FPG, 2-h postchallenge glucose exists to identify individuals with prediabetes and that the cardiometabolic risk profile of these individuals varies by metabolic parameter, with 2-h postchallenge glucose showing stronger associations with cardiometabolic risk factors and subclinical atherosclerosis than FPG or A1C.
Acknowledgments
This work was partly supported by the Italian Ministry of Health (Grant RF-FSR-2007-631176) to G.S.
No potential conflicts of interest relevant to this article were reported.
M.A.M., E.S., E.C., S.C., F.A., and A.S. acquired, analyzed, and interpreted data. R.L. and F.P. contributed to discussion and reviewed the manuscript. M.L.H. reviewed and edited the manuscript. G.S. designed the study, analyzed and interpreted the data, and wrote the manuscript. G.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-2032/-/DC1.
References
- 1.Nathan DM, Singer DE, Hurxthal K, Goodson JD. The clinical information value of the glycosylated hemoglobin assay. N Engl J Med 1984;310:341–346 [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association Standards of medical care in diabetes—2011. Diabetes Care 2011;34(Suppl. 1):S11–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Expert Committee International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327–1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mann DM, Carson AP, Shimbo D, Fonseca V, Fox CS, Muntner P. Impact of A1C screening criterion on the diagnosis of pre-diabetes among U.S. adults. Diabetes Care 2010;33:2190–2195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohan V, Vijayachandrika V, Gokulakrishnan K, et al. A1C cut points to define various glucose intolerance groups in Asian Indians. Diabetes Care 2010;33:515–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olson DE, Rhee MK, Herrick K, Ziemer DC, Twombly JG, Phillips LS. Screening for diabetes and pre-diabetes with proposed A1C-based diagnostic criteria. Diabetes Care 2010;33:2184–2189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.James C, Bullard KM, Rolka DB, et al. Implications of alternative definitions of prediabetes for prevalence in U.S. adults. Diabetes Care 2011;34:387–391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lorenzo C, Wagenknecht LE, Hanley AJ, Rewers MJ, Karter AJ, Haffner SM. A1C between 5.7 and 6.4% as a marker for identifying pre-diabetes, insulin sensitivity and secretion, and cardiovascular risk factors: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Care 2010;33:2104–2109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Succurro E, Marini MA, Arturi F, et al. Usefulness of hemoglobin A1c as a criterion to define the metabolic syndrome in a cohort of italian nondiabetic white subjects. Am J Cardiol 2011;107:1650–1655 [DOI] [PubMed] [Google Scholar]
- 10.Pinelli NR, Jantz AS, Martin ET, Jaber LA. Sensitivity and specificity of glycated hemoglobin as a diagnostic test for diabetes and prediabetes in Arabs. J Clin Endocrinol Metab 2011;96:E1680–E1683 [DOI] [PubMed] [Google Scholar]
- 11.The DECODE study group on behalf of the European Diabetes Epidemiology Group Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. Lancet 1999;354:617–621 [PubMed] [Google Scholar]
- 12.Nakagami T, DECODA Study Group Hyperglycaemia and mortality from all causes and from cardiovascular disease in five populations of Asian origin. Diabetologia 2004;47:385–394 [DOI] [PubMed] [Google Scholar]
- 13.Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010;362:800–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qiao Q, Dekker JM, de Vegt F, et al. Two prospective studies found that elevated 2-hr glucose predicted male mortality independent of fasting glucose and HbA1c. J Clin Epidemiol 2004;57:590–596 [DOI] [PubMed] [Google Scholar]
- 15.Park S, Barrett-Connor E, Wingard DL, Shan J, Edelstein S. GHb is a better predictor of cardiovascular disease than fasting or postchallenge plasma glucose in women without diabetes. The Rancho Bernardo Study. Diabetes Care 1996;19:450–456 [DOI] [PubMed] [Google Scholar]
- 16.de Vegt F, Dekker JM, Ruhé HG, et al. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study. Diabetologia 1999;42:926–931 [DOI] [PubMed] [Google Scholar]
- 17.Marini MA, Succurro E, Frontoni S, et al. Metabolically healthy but obese women have an intermediate cardiovascular risk profile between healthy nonobese women and obese insulin-resistant women. Diabetes Care 2007;30:2145–2147 [DOI] [PubMed] [Google Scholar]
- 18.Succurro E, Andreozzi F, Marini MA, et al. Low plasma insulin-like growth factor-1 levels are associated with reduced insulin sensitivity and increased insulin secretion in nondiabetic subjects. Nutr Metab Cardiovasc Dis 2009;19:713–719 [DOI] [PubMed] [Google Scholar]
- 19.Cardellini M, Marini MA, Frontoni S, et al. Carotid artery intima-media thickness is associated with insulin-mediated glucose disposal in nondiabetic normotensive offspring of type 2 diabetic patients. Am J Physiol Endocrinol Metab 2007;292:E347–E352 [DOI] [PubMed] [Google Scholar]
- 20.Wilson PWF, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation 1998;97:1837–1847 [DOI] [PubMed] [Google Scholar]
- 21.Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 1999;22:1462–1470 [DOI] [PubMed] [Google Scholar]
- 22.Herman WH, Ma Y, Uwaifo G, et al. Diabetes Prevention Program Research Group Differences in A1C by race and ethnicity among patients with impaired glucose tolerance in the Diabetes Prevention Program. Diabetes Care 2007;30:2453–2457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nathan DM, Davidson MB, DeFronzo RA, et al. American Diabetes Association Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 2007;30:753–759 [DOI] [PubMed] [Google Scholar]
- 24.Carson AP, Reynolds K, Fonseca VA, Muntner P. Comparison of A1C and fasting glucose criteria to diagnose diabetes among U.S. adults. Diabetes Care 2010;33:95–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care 2010;33:562–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kramer CK, Araneta MR, Barrett-Connor E. A1C and diabetes diagnosis: The Rancho Bernardo Study. Diabetes Care 2010;33:101–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marini MA, Succurro E, Arturi F, et al. Comparison of A1C, fasting and 2-h post-load plasma glucose criteria to diagnose diabetes in Italian Caucasians. Nutr Metab Cardiovasc Dis 23 September 2011 [Epub ahead of print: http://dx.doi.org/10.1016/j.numecd.2011.04.009] [DOI] [PubMed] [Google Scholar]
- 28.Meigs JB, Nathan DM, D’Agostino RB, Sr, Wilson PW, Framingham Offspring Study Fasting and postchallenge glycemia and cardiovascular disease risk: the Framingham Offspring Study. Diabetes Care 2002;25:1845–1850 [DOI] [PubMed] [Google Scholar]
- 29.Smith NL, Barzilay JI, Shaffer D, et al. Fasting and 2-hour postchallenge serum glucose measures and risk of incident cardiovascular events in the elderly: the Cardiovascular Health Study. Arch Intern Med 2002;162:209–216 [DOI] [PubMed] [Google Scholar]
- 30.Saukkonen T, Cederberg H, Jokelainen J, et al. Limited overlap between intermediate hyperglycemia as defined by A1C 5.7-6.4%, impaired fasting glucose, and impaired glucose tolerance. Diabetes Care 2011;34:2314–2316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rijkelijkhuizen JM, Nijpels G, Heine RJ, Bouter LM, Stehouwer CD, Dekker JM. High risk of cardiovascular mortality in individuals with impaired fasting glucose is explained by conversion to diabetes: the Hoorn study. Diabetes Care 2007;30:332–336 [DOI] [PubMed] [Google Scholar]
- 32.Ratner R, Goldberg R, Haffner S, et al. Diabetes Prevention Program Research Group Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program. Diabetes Care 2005;28:888–894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M, STOP-NIDDM Trial Research Group Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA 2003;290:486–494 [DOI] [PubMed] [Google Scholar]
- 34.Perticone F, Maio R, Sciacqua A, et al. Endothelial dysfunction and C-reactive protein are risk factors for diabetes in essential hypertension. Diabetes 2008;57:167–171 [DOI] [PubMed] [Google Scholar]
- 35.Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 2000;342:836–843 [DOI] [PubMed] [Google Scholar]
- 36.D’Alessandris C, Lauro R, Presta I, Sesti G. C-reactive protein induces phosphorylation of insulin receptor substrate-1 on Ser307 and Ser 612 in L6 myocytes, thereby impairing the insulin signalling pathway that promotes glucose transport. Diabetologia 2007;50:840–849 [DOI] [PubMed] [Google Scholar]
- 37.Verma S, Wang CH, Li SH, et al. A self-fulfilling prophecy: C-reactive protein attenuates nitric oxide production and inhibits angiogenesis. Circulation 2002;106:913–919 [DOI] [PubMed] [Google Scholar]