Abstract
The authors report on the development of a manual for treating adolescents with anorexia nervosa modeled on a family-based intervention originating at the Maudsley Hospital in London. The manual provides the first detailed account of a clinical approach shown to be consistently efficacious in randomized clinical trials for this disorder. Manualized family therapy appears to be acceptable to therapists, patients, and families. Preliminary outcomes are comparable to what would be expected in clinically supervised sessions. These results suggest that through the use of this manual a valuable treatment approach can now be tested more broadly in controlled and uncontrolled settings.
Keywords: Family Therapy, Eating Disorders, Manualized Treatments
Anorexia Nervosa (AN) is a relatively uncommon disorder with an age-adjusted incidence rate of 14.6 per 100,000 for females 15 through 24 years of age.1 Nonetheless, it is the third most common chronic condition of adolescent females.2 Moreover, chronic AN is associated with a host of acute and chronic medical problems, including bradycardia, orthostatic hypotension, growth retardation, osteoporosis, and infertility.2 In addition to these, depression and anxiety disorders are often associated conditions.3 Mortality rates for AN are exceptionally high for a psychiatric illness, with reports varying from 6% to 10% in adolescent cases.4–7
Unfortunately, our understanding of how best to treat AN has lagged behind our knowledge of the medical and epidemiological features of the illness. To date, there are only nine randomized clinical treatment trials published in the literature.8–16 The total number of patients investigated in all these studies combined is less than 400. The range of treatments studied includes nutritional counseling, cognitive-behavioral therapy, behavioral therapy, family therapy, and individual supportive and analytic therapy. Of these treatments, there is the most evidence supporting a particular type of family-based treatment for adolescents with AN.8–10 This form of treatment was developed at the Maudsley Hospital by Christopher Dare and Ivan Eisler and has been used in a series of controlled treatment studies since 1987. Their approach has consistently demonstrated efficacy in approximately two-thirds of the adolescent AN patients treated. Further, at 5-year follow-up these patients continued to do better than comparison patients.17
The present report summarizes our experiences to date with developing a manual for the type of family-based treatment of AN originating at the Maudsley Hospital in London. The process of developing a manual will be described, and its implementation as a training vehicle for therapists employed in a treatment trial will be reported, along with preliminary information about how patients are faring.
FAMILY TREATMENT OF ANOREXIA NERVOSA
The role of the family in treating AN has been debated since the illness was first described in the late 19th century. The two physicians who first reported the illness were at odds on the issue. William Gull (1874)18 suggested that families were the “worst attendants” for their children. On the other hand, Charles Lasegue (1873)19 held that the family was essential when treating the person with AN and that he considered the “morbid state of the hysterical patient side by side with the preoccupations of her relatives.” Alternatively, Hilde Bruch (1973),20 using an individual psychodynamic approach, suggested that the person with AN suffers from an inadequate self; therefore treatment should be individually based and aimed at developing this deficient self. Such treatments focus on a one-to-one relationship with a caring and supportive therapist. Often, families are viewed as unnecessary or, worse, as obstructing this process. Family therapy for AN was pioneered by Salvador Minuchin21and Mara Selvini Palazzoli in the 1970s.22 These clinicians and their adherents believe that the family's structure or style of management of problems need to be corrected in order for patients to recover from AN.
In line with those who found families essential in the treatment of AN, Christopher Dare and colleagues at the Maudsley Hospital devised a treatment that involves families, but that opposes the tradition of finding families pathological and blaming them for the development of AN.23 Instead, Dare takes an “agnostic” view of the cause of AN consistent with the theoretical work of Jay Haley and Milton Erickson24 and suggests that the family is the most important resource at the therapist's disposal to ensure recovery. The Maudsley approach incorporates elements of a variety of treatment methods developed by other clinicians as well, including the use of family meals; specific techniques for family empowerment; a non-authoritarian therapeutic stance; and externalizing the illness from the patient and family. Family meals were used by Minuchin in his structural family therapy,21 and family empowerment is based in the non-authoritarian stance of strategic systems therapy as well as feminist theory.25,26 The emphasis on separating the patient from the illness is based on narrative therapy techniques.27
Family-based treatment modeled on the Maudsley approach to adolescent AN proceeds through three clearly defined phases. In the first phase, the therapist focuses on the dangers of severe malnutrition associated with AN and emphasizes the need for parents to take immediate action to reverse this. The therapist supports the development of a parental alliance around re-feeding, while also aligning the patient with the sibling subsystem. During this phase, a family meal is conducted that allows the therapist to observe familial interaction patterns around eating. Once the patient accepts the demands of the parents and steady weight gain is evident, phase two begins. Here the treatment focuses on encouraging the parents to help their child to take more control over eating on her own. When the patient is maintaining a stable weight near 95% of her ideal weight on her own, therapy focuses on the impact AN has had on the establishing of a healthy adolescent identity. This entails a review of central issues of adolescence and includes supporting increased personal autonomy for the adolescent and the development of appropriate parental boundaries.
MANUAL DEVELOPMENT
Many clinicians have expressed considerable distaste for treatment manuals. They have characterized them as being “recipes” rather than treatment. They report that manuals are overly general and do not provide enough specificity to be of use with real patients. Most important, manuals are perceived as interfering with the therapist–patient relationship and the building of therapeutic rapport, and as extinguishing the intuitive qualities of therapeutic work. On the other hand, manuals provide a focus for the treatment process and help the therapist to set appropriate treatment goals, time interventions, codify effective treatments and experience, and provide an overall structure for the treatment process.
In addition, manuals are necessary to conduct systematic research. For instance, manuals of cognitive-behavioral treatment are used in treatment studies of other eating disorders, specifically bulimia nervosa and binge eating disorder.28–30 One of the limitations of the Maudsley Hospital research studies is that the treatment used did not employ a manual. Manualized versions of psychotherapeutic interventions are standard for controlled treatment studies in the United States. Manuals allow for consistent application of interventions across patients and over time, are less dependent on individual characteristics of the therapist for efficacy, and provide a clear description of the course of treatment. In addition, without a treatment manual it is impossible to replicate treatments at other sites. Hence, there have been no replications of the Maudsley approach to AN in adolescents outside their own center.
The Process for Creating a Manual
The decision to manualize was based on the need to replicate the Maudsley approach in other settings and to conduct additional therapeutic trials of this method. The process for creating a manual involved several stages: 1) reviewing existing descriptions of the treatment, 2) consulting with clinicians trained in the techniques, 3) developing a narrative structure that fit the model of treatment, 4) piloting the treatment manual, and 5) training others in the use of the manual.
Reviewing existing descriptions of the treatment: Various descriptions exist of the main interventions and strategies employed in the family-based approach to AN at the Maudsley Hospital.8,9,23,31–34 Through the process of reviewing these treatment descriptions, the main elements of the therapy were identified. In addition, the theoretical underpinnings of these interventions were described. An outline of the major phases of treatment as well as the key interventions for each of these phases was developed.
Consulting with clinicians trained in the Maudsley approach: Consultation with Dr. Daniel le Grange, a psychologist trained at the Maudsley Hospital in family treatment for AN, began with a review of the findings in the research literature. Further consultation included a review of draft elements of the manual and supervision of piloted cases. Additional consultation with Christopher Dare at the Maudsley Hospital followed the preparation of a complete draft text. Consultative comments and criticisms were incorporated throughout. This consultation helped to ensure that the manual, model, and treatment were consistent with that used in the clinical trials which provided evidence that the treatment was efficacious.
Developing a narrative structure to fit the model: An important and creative aspect of manual development is the consideration of the form of the text. In this case, the goals were to create a useable text as well as provide a meaningful training document and reference for clinicians. This meant that the structure should be at once accessible and detailed. After several attempts, a model that allowed for easy reference while making other information readily available was decided upon. On the largest structural level, it consists of the three phases of treatment already described by Dare and colleagues. However, specific goals for each phase and for sessions within each phase were developed to specify and delineate treatment over time. In addition, within each session, a specific set of therapeutic interventions was outlined and sequenced. Finally, a three-pronged description of each intervention was developed. This consists of a “what, how, why” formulation for each major intervention or therapeutic strategy. The “what” is a short statement of the intervention (e.g., weigh the patient). The “how” provides a narrative description of the manner in which the intervention should be undertaken and includes short examples (e.g., take the patient into a room and ask her to step on the scale). The “why” section provides the therapists with a theoretical orientation to the task and may often be conjectural rather than proven (e.g., in order to track a family's progress, it is important that family members receive regular feedback on their efforts to re-feed their child). Next, in order to provide clinicians with additional assistance, a “common difficulties” section was added for each intervention (e.g., what to do if the patient refuses to be weighed). These sections allow for a discussion of issues therapists will often face in trying to implement a particular intervention. Finally, to enable therapists to get a sense of how the interventions worked together in vivo, transcriptions of key sessions are provided as therapy “in action.”
Piloting the treatment: After an initial draft of the manual had been developed, refined, and revised through the work of the principal authors and consultants, the manualized version was ready to be piloted. Adolescent patients were identified through referral processes and offered treatment using the manual. Two families agreed to treatment. Each session was videotaped, transcribed, and then reviewed by both the principal authors and consultants. Patients were treated for approximately 12 months. Both patients recovered from AN, and a trained consultant review of videotaped sessions confirmed that the treatment replicated the Maudsley approach.
Training therapists in use of the manual: In order to test the effectiveness of the manual as an instrument to communicate the family-based approach, five therapists have been trained. Training consisted of reading the manual, reviewing videotapes of key sessions based on the manual, and in some cases observing in vivo treatment sessions. After training, therapists videotaped their sessions with patients and these were reviewed by the principal authors of the manual to ensure compliance with the manual's structure and content. All therapists trained were able to replicate treatment according to the manual.
The manual was recently published as an effort to make the clinical approach more available to clinicians practicing outside research centers.35
CURRENT RESEARCH
The manualized version of family-based therapy described above is currently being used in an NIMH clinical trial (K08 01457) comparing two levels of intensity and duration of this treatment for adolescents with AN. The overall question the study hopes to answer is: How much family-based treatment is needed to help adolescents with AN? The intention is to compare the effectiveness of family treatment at two different levels of intensity and time course to reduce the number of hospital days and overall costs of care during a 12-month experimental period and to explore clinical factors predicting outcome. Data collected from a variety of baseline and follow-up measures should help to predict if there are patient characteristics that may influence outcomes. To date, 43 families have been recruited into the study. Of these, 19 have completed 6 months of treatment and 13 have completed 12 months of treatment. Below we present data from the first 19 cases.
RESULTS
Demographics
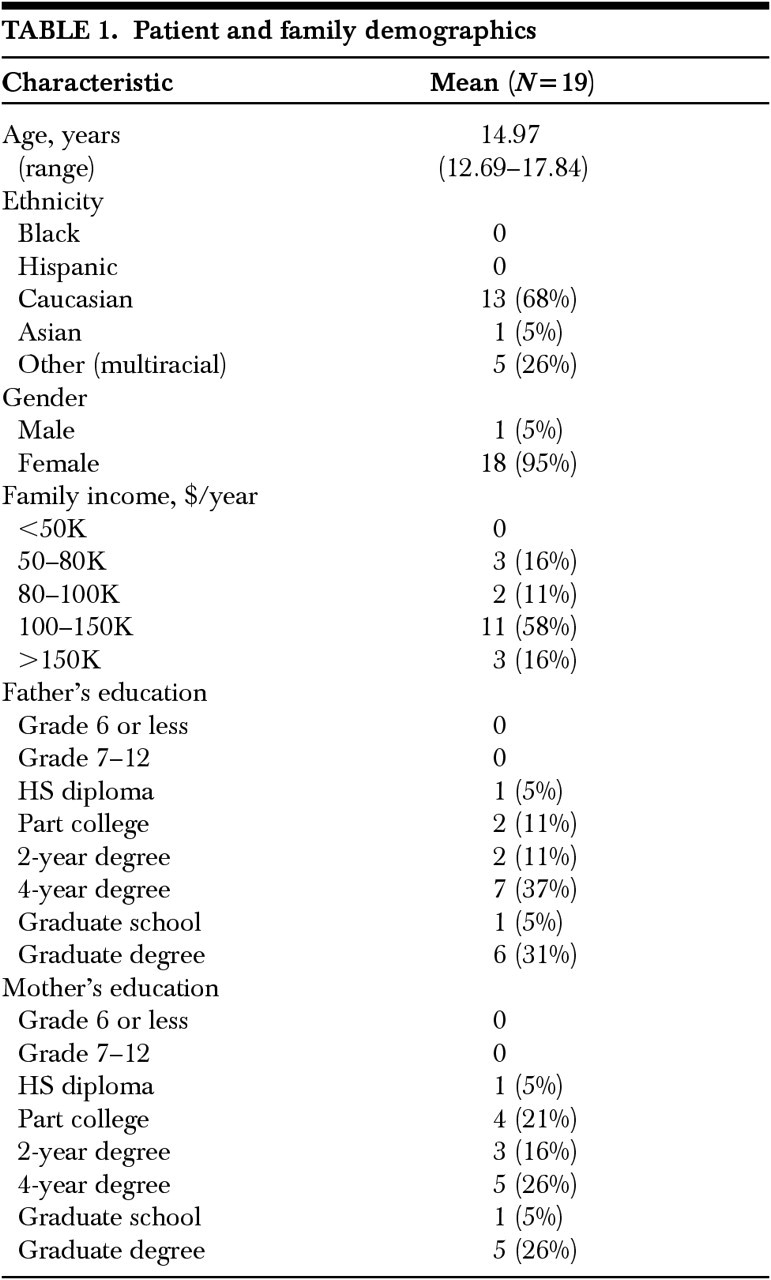
The mean age of patients in the study is 14.97 years (range 12.69–17.84). Ninety-two percent of patients are female. The mean duration of illness is 10.9 months (range 3–36). The majority of patients (68%) are white, 5% are Asian, and 26% identified themselves as “other.” For the most part the families are middle to upper middle class, with incomes greater than $80K per annum in 85% of families. In addition, the families are highly educated, with 95% of fathers having some college and 36% with graduate education. Demographic data are shown in Table 1.
TABLE 1. Patient and family demographics.
Weight Change
In order to enter treatment, patients had to meet weight loss criteria for AN. Mean qualifying weight for patients was 81% of ideal body weight (IBW). At the beginning of treatment patients had a mean weight of 88% IBW. This initial weight gain was due for the most part to a large subset of patients who required medical hospitalization for complications of severe malnutrition prior to beginning outpatient treatment. At 6 months, the mean weight for 19 subjects was 92% IBW. Body mass index (BMI) at baseline was 17.18 (SD=1.37). It rose to 18.8 at 6 months after treatment began (P=0.0001, effect size=–1.22). By 6 months, 89% of patients no longer met BMI criteria for AN.
Binge/Purge Characteristics
At baseline 26% (5) of the patients exhibited binge eating or purging characteristics in conjunction with AN. At 6-month follow-up, 60% (3) of these patients were abstinent, and symptoms were dramatically reduced from baseline in the remaining 2 patients (53% and 88%, respectively). One patient without prior purging began using laxatives during this period (3 episodes of laxative use).
Psychological Change
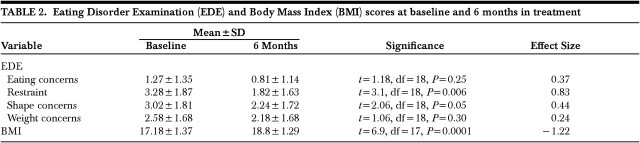
The standard measure of psychological change for eating disorders is the Eating Disorder Examination.36 The EDE has been used in several large treatment studies for eating disorders.37,38 For patients in our study, the baseline mean scores on the four EDE subscales were consistent with those expected for patients with a diagnosis of AN: Eating Concerns=1.27 (SD=1.35), Restraint=3.28 (SD=1.87), Shape Concerns=3.02 (SD=1.81), and Weight Concerns=2.58 (SD=1.68). All measures declined during the 6-month treatment period; however, only Restraint and Shape Concerns showed statistically significant changes. The largest change was in the Restraint subscale of the EDE (effect size=0.83). Data are shown in Table 2.
TABLE 2. Eating Disorder Examination (EDE) and Body Mass Index (BMI) scores at baseline and 6 months in treatment.
DISCUSSION
In this preliminary report, we found that a manualized version of family therapy for AN can be devised that provides consistent, focused, and directed interventions. Further, therapists can be trained to use the manual and find its clinical use acceptable. In addition, many families and patients appear to have few difficulties with using this approach.
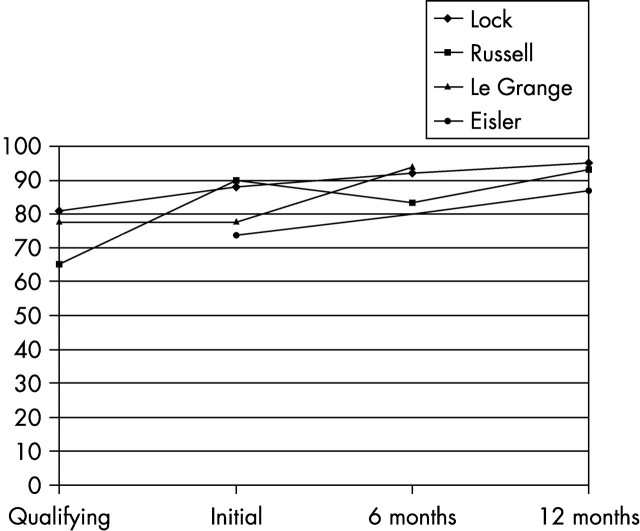
On the basis of this case series, we find that the manualized version of family therapy appears to be effective in reversing self-starvation and in improving some key psychological measures related to the disordered thinking associated with AN in a relatively short time period. Compared with earlier treatment studies using a non-manualized version, our results are comparable in terms of weight restoration. For example, in the original study by Russell et al.,8 patients were weight-restored to 90% of IBW in the hospital prior to starting treatment, but at 6 months the patients' mean weights had dropped to 83% IBW compared with 92% IBW in our group. At 12 months, Russell et al. and our group reached similar percentages of IBW, approaching 95% in both. Our 6-month outcomes were similar to those found by Le Grange et al.9 in their pilot treatment study. In the recent study by Eisler et al.,10 only 12-month outcomes are published. In that sample, where patients did not receive any baseline hospitalization, outcomes at 12 months were lower (87% IBW) than in the Russell study or in our group to date (Figure 1).
FIGURE 1.
Outcomes of family-based treatment studies of adolescents with anorexia nervosa: Lock & Le Grange (present study), Russell et al,8 Le Grange et al.,9 Eisler et al.10 IBW=ideal body weight.
In respect to some of the possible predictors and moderators of response, our data are too limited to draw conclusions, but our clinical observations about some key variables may be pertinent, including age, duration of illness, binge eating and purging characteristics, and treatment adherence.
The literature on the impact of age on outcome of AN remains controversial. Early onset and very early onset have been associated with better,39–41 no different,42,43 and worse outcomes.44,45 Age was specifically assessed as a predictor of treatment response in the original Maudsley trial8 comparing individual to family therapy. The authors concluded that age was an important determinant of treatment response to their therapy. They found that for patients whose illness began before age 19, family therapy was superior, whereas for patients over age 19, individual therapy was superior. Although the current case series has insufficient numbers to allow us to assess the effect of age, clinicians have not detected a pattern of older patients refusing family-based help or younger patients being unable to use it. However, it should be noted that age might at times affect how therapy is conducted. For example, with younger patients, the therapist might have greater difficulty entering into a treatment alliance because younger patients appear to deny their illness more and feel treatment is not necessary.46
A variety of studies suggest that chronic illness makes it less likely that a patient will respond to a specific treatment In Russell et al.,8 duration of illness was reported as having a negative effect. Specifically, patients with illness of greater than 3 years' duration did less well than those with illness lasting less than this. More recently, Eisler et al.10 found that those with poor or intermediate outcomes were ill for a significantly longer period than those with good outcomes (short illness: <5.7 months). In our present study, the mean duration of illness at this point in time is a little less than 11 months. Overall, this would suggest a positive prognosis. However, it is interesting that no dropouts were from the longer duration of illness group, and only 1 of the 6 patients with longer duration of illness appeared not to respond well to treatment up to this point. At the same time, clinically it must be noted that therapy with families that have been dealing with AN for a longer period of time presented different challenges. These included initially greater resistance by the patient to parental re-feeding and greater difficulty for the therapist in activating the parents to take action against the illness (presumably because the parents had adopted a sustained passive stance). On the other hand, among the few cases that fell into this category, there was a palpable relief when parents recognized there might be a way out of the illness. For the patient, there was often greater understanding of the cost of AN to her life as she had experienced repeated hospitalization and treatment failures, allowing the therapist more easily to put a wedge between her pre- and post-anorexia self.
Previous treatment for AN has been suggested to be a poor prognosticator for response to a new treatment. This seems reasonable on general grounds, in the sense that the illness is likely to be more entrenched and that feelings of hopelessness and pessimism are now based on the grim reality of previous failure. Eisler et al.10 suggest patients who had no previous therapy did better, with only 3 of 16 having a poor outcome. To date in our study in progress, 36% (7) had previous treatment, and most did well in terms of weight gain. On the other hand, it is noteworthy that one of the few treatment dropouts was from this small subset, perhaps suggesting that patients with previous treatment are less likely to respond to this form of treatment as well.
The relationship of binge eating and purging to recovery from AN is unclear. Some authors have suggested that the presence of these characteristics appears to improve short-term recovery rates,47 presumably because these patients are more likely to become weight-recovered. Others have suggested that the presence of these symptoms complicates treatment and makes a good response less likely. For example, in the initial Maudsley study, the presence of bulimic symptoms appeared to worsen outcomes and reduce the effectiveness of family therapy.8 This trend continued to be present at 5 years post treatment.17 In the present study cohort, 26% (5) had binge/purge characteristics. As noted, 60% (3) of these patients had ceased bulimic behaviors by 6 months, and others had significantly decreased these behaviors. Only 1 patient had initiated purging, and this was at a low level. Clinically, the presence of these symptoms made the work of the parents harder because they had to monitor both food intake and purging behavior. However, it also suggests that parental monitoring of binge eating or purging may be an important strategy in working with adolescents who binge eat and/ or purge, as suggested by the earlier work of Dodge et al.48 We are currently undertaking another NIMH-sponsored investigation of family-based treatment for adolescents with bulimia nervosa to better understand the efficacy of this treatment with this population.
Treatment adherence is a well-known problem with AN treatment.8,15,49 It is noteworthy that in the original Maudsley study, the recommended course of treatment was 12 months without a specified number of treatment sessions.8 More recently, Eisler et al.10 reported that 10% of patients dropped out treatment and most patients completed about 95% of planned sessions, although about one-third completed only about half the sessions. In our present cohort, 15% (3) dropped out of treatment, but all kept scheduled appointments up to that point. In addition, in all cases except one, families completed at least 50% of their allotted sessions. This suggests that treatment adherence has been remarkably high so far. In part, we believe this is true because the protocol is well understood from the start of treatment and future sessions are scheduled out in approximately 2-month blocks.
There are significant limitations to our data that should be considered when interpreting our findings. The present data are from an uncontrolled case series rather than a comparison of controlled treatment. In addition, the data are based on only 19 subjects treated for only 6 months. Patients had been ill for a relatively short period of time; as a whole they had moderately well-off and well-educated parents; and many had been treated in a hospital prior to the onset of treatment. Each of these factors may have an impact on the generalizability our findings. However, the primary purpose of this preliminary report is to introduce the treatment approach used at the Maudsley Hospital through a manual and to report on its effectiveness in this format. The full treatment trial under way will help to address many of the above limitations.
CONCLUSIONS
The most important conclusion from this preliminary report is that a treatment manual that systematically describes the interventions used at the Maudsley hospital in its treatment studies of family-based treatment for AN adolescents can be developed. Further, manualized family therapy appears to be acceptable to therapists and to patients and families. In addition, preliminary findings are comparable to those that would have been expected in the supervised sessions conducted at the Maudsley Hospital. These results are important because they suggest that a valuable treatment approach can now be tested more broadly in controlled and uncontrolled settings. Therapists now have a tool at their disposal to add to their strategies to combat AN. In addition, researchers who have received training in the use of the manual in research can systematically examine the treatment more closely to better explore its effectiveness, as well as the predictors and moderators of response to treatment.
ACKNOWLEDGEMENTS
Dr. Lock's work on this article was supported by a Career Development Award from the National Institute of Mental Health (K08-01457).
References
- 1.Lucas AR, Beard CM, O'Fallon WM: 50-year trends in the incidence of anorexia nervosa in Rochester, Minn.: a population-based study. Am J Psychiatry 1991; 148:917-929 [DOI] [PubMed] [Google Scholar]
- 2.Fisher M, Golden N, Katzman DK, et al: Eating disorders in adolescents: a background paper. J Adolesc Health 1995; 16: 420-437 [DOI] [PubMed]
- 3.Herzog DB, Keller MB, Sacks NR, et al: Psychiatric comorbidity in treatment-seeking anorexics and bulimics. J Am Acad Child Adolesc Psychiatry 1992; 31:810-818 [DOI] [PubMed] [Google Scholar]
- 4.Herzog DB, Keller MB, Lavori PW, et al: The course and outcome of bulimia nervosa. J Clin Psychiatry 1991; 52(suppl):4-8 [PubMed]
- 5.Herzog DB, Greenwood DN, Dover DJ, et al: Mortality in eating disorders: a descriptive study. International Journal of Eating Disorders 2000; 28:20-26 [DOI] [PubMed] [Google Scholar]
- 6.Steinhausen H, Rauss-Mason C, Seidel R: Follow-up studies of anorexia nervosa: a review of four decades of outcome research. Psychol Med 1991; 21:447-454 [DOI] [PubMed] [Google Scholar]
- 7.Steinhausen H, Rauss-Mason C, Seidel R: Short-term and intermediate term outcome in adolescent eating disorders. Acta Psychiatr Scand 1993; 88:169-173 [DOI] [PubMed] [Google Scholar]
- 8.Russell GFM, Szmukler GI, Dare C, et al: Family therapy versus individual therapy for adolescent females with anorexia nervosa and bulimia nervosa. Arch Gen Psychiatry 1987; 44:1047-1056 [DOI] [PubMed] [Google Scholar]
- 9.Le Grange D, Eisler I, Dare C, et al: Evaluation of family treatments in adolescent anorexia nervosa: a pilot study. International Journal of Eating Disorders 1992; 12:347-357 [Google Scholar]
- 10.Eisler I, Dare C, Hodes M, et al: Family therapy for adolescent anorexia nervosa: the results of a controlled comparison of two family interventions. J Child Psychol Psychiatry 2000; 41:727-736 [PubMed] [Google Scholar]
- 11.Crisp AH, Norton K, Gowers S, et al: A controlled study of the effect of therapies aimed at adolescent and family psychopathology in anorexia nervosa. Br J Psychiatry 1991; 159:325-333 [DOI] [PubMed] [Google Scholar]
- 12.Hall A, Crisp AH: Brief psychotherapy in the treatment of anorexia nervosa: outcome at one year. Br J Psychiatry 1987; 151:185-191 [DOI] [PubMed] [Google Scholar]
- 13.Robin A, Siegal PT, Moye AW, et al: A controlled comparison of family versus individual therapy for adolescents with anorexia nervosa. J Am Acad Child Adolesc Psychiatry 1999; 38:1482-1489 [DOI] [PubMed] [Google Scholar]
- 14.Channon S, de Silva P, Hemsley D, et al: A controlled trial of cognitive-behavioural and behavioural treatment of anorexia nervosa. Behav Res Ther 1989; 27:529-535 [DOI] [PubMed] [Google Scholar]
- 15.Treasure JL, Todd G, Brolly M, et al: A pilot study of a randomized trial of cognitive-behavioral analytical therapy vs educational behavioral therapy for adult anorexia nervosa. Behav Res Ther 1995; 33:363-367 [DOI] [PubMed] [Google Scholar]
- 16.Dare C, Eisler I, Russell GF, et al: Psychological therapies for adults with anorexia nervosa: randomized controlled trial of outpatient treatments. Br J Psychiatry 2001; 178:216-221 [DOI] [PubMed] [Google Scholar]
- 17.Eisler I, Dare C, Russell GF, et al: Family and individual therapy in anorexia nervosa: a five-year follow-up. Arch Gen Psychiatry 1997; 54:1025-1030 [DOI] [PubMed] [Google Scholar]
- 18.Gull W: Anorexia nervosa (apepsia hysterica, anorexia hysterica). Transactions of the Clinical Society of London 1874; 7:222-228 [Google Scholar]
- 19.Lasègue EC: On hysterical anorexia (1873), in Evolution of Psychosomatic Concepts—Anorexia Nervosa: A Paradigm, edited by Kaufman MR, Heiman M. New York, International Universities Press, 1964, pp 298-319
- 20.Bruch H: Eating Disorders: Obesity, Anorexia Nervosa, and the Person Within. New York, Basic Books, 1973
- 21.Minuchin S, Rosman B, Baker I: Psychosomatic Families: Anorexia Nervosa in Context. Cambridge, MA, Harvard University Press, 1978
- 22.Palazzoli M: Self-Starvation: From the Intrapsychic to the Transpersonal Approach to Anorexia Nervosa. London, Chaucer Publishing, 1974
- 23.Dare C, Eisler I: Family therapy for anorexia nervosa, in Handbook of Treatment for Eating Disorders, edited by Garner DM, Garfinkel P. New York, Guilford, 1997, pp 307-324
- 24.Haley J: Uncommon Therapy: The Psychiatric Techniques of Milton H. New York, WW Norton, 1973
- 25.Mandanes C: Strategic Family Therapy. San Francisco, Jossey-Bass, 1981
- 26.Schwartz R, Barrett M, Saba G: Women and eating disorders. Journal of Psychotherapy and the Family 1988; 3:131-144 [Google Scholar]
- 27.White M: Anorexia nervosa: a cybernetic perspective. Family Therapy Collections 1987; 20:117-129 [Google Scholar]
- 28.Fairburn CG: Overcoming Binge Eating. New York, Guilford, 1995
- 29.Apple RF, Agras WS: Overcoming Eating Disorders: A Cognitive-behavioral Treatment for Bulimia Nervosa and Binge Eating Disorder: Client Workbook. San Antonio, TX, The Psychological Corporation, 1997
- 30.Agras WS, Apple RF: Overcoming Eating Disorders: A Cognitive-behavioral Treatment for Bulimia Nervosa and Binge Eating Disorder: Therapist Guide. San Antonio, TX, The Psychological Corporation, 1997
- 31.Dare C, Eisler I: Family therapy for anorexia nervosa, in The Nature and Management of Feeding Problems in Young People, edited by Cooper I, Stein A. New York, Harwood Academics, 1992
- 32.Dare C, Eisler I, Colohan M, et al: The listening heart and the chi square: clinical and empirical perceptions in the family therapy of anorexia nervosa. Journal of Family Therapy 1995; 17:31-58 [Google Scholar]
- 33.Dare C, Eisler F, Russell GF, et al: Family therapy for anorexia nervosa: implications from the results of a controlled trial of family and individual therapy. J Marital Fam Ther 1990; 16:39-57 [Google Scholar]
- 34.Eisler I: Combining individual and family therapy in adolescent anorexia nervosa, in Treating Eating Disorders, edited by Werne J. San Francisco, Jossey-Bass, 1995
- 35.Lock J, Le Grange D, Agras WS, et al: Treatment Manual for Anorexia Nervosa: A Family Based Approach. New York, Guilford, 2001
- 36.Cooper Z, Fairburn CG: The Eating Disorder Examination: a semi-structured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders 1987; 6:1-8 [Google Scholar]
- 37.Agras WS, Walsh BT, Fairburn CG, et al: A multicenter comparison of cognitive-behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Arch Gen Psychiatry 2000; 57:459-466 [DOI] [PubMed] [Google Scholar]
- 38.Fairburn CG, Jones R, Peveler RC, et al: Three psychological treatments for bulimia nervosa: a comparative trial. Arch Gen Psychiatry 1991; 48:463-469 [DOI] [PubMed] [Google Scholar]
- 39.Blitzer J, Rollins N, Blackwell A: Children who starve themselves: anorexia nervosa. Psychosom Med 1961; 23:369-383 [DOI] [PubMed] [Google Scholar]
- 40.Halmi K, Brodland G, Loney J: Progress in anorexia nervosa. Ann Intern Med 1973; 78:907-909 [DOI] [PubMed] [Google Scholar]
- 41.Lesser L, Asheriden BJ, Delvuskey M, et al: Anorexia nervosa in children. Am J Orthopsychiatry 1960; 30:572-580 [DOI] [PubMed] [Google Scholar]
- 42.Swift W: The long-term outcome of early onset anorexia nervosa: a critical review. J Am Acad Child Adolesc Psychiatry 1982; 21:38-46 [DOI] [PubMed] [Google Scholar]
- 43.Hawley R, The outcome of anorexia nervosa in younger subjects. Br J Psychiatry 1985; 146:657-660 [DOI] [PubMed] [Google Scholar]
- 44.Bryant-Waugh R, Knibbs J, Fasson A, et al: Long-term follow-up of patients with early onset anorexia nervosa. Archives of Diseases of Childhood 1988. 63:5-9 [DOI] [PMC free article] [PubMed]
- 45.Walford G, McCune N; Long-term outcome in early onset anorexia nervosa. Br J Psychiatry 1991; 159:383-389 [DOI] [PubMed] [Google Scholar]
- 46.Fisher M, Schneider M, Burns J, et al: Differences between adolescents and young adults at presentation to an eating disorder program. J Adolesc Health 2001; 28:222-227 [DOI] [PubMed] [Google Scholar]
- 47.Herzog DB, Nussbaum KM, Marmor AK: Comorbidity and outcome in eating disorders. Psychiatr Clin North Am 1996; 19:843-59 [DOI] [PubMed] [Google Scholar]
- 48.Dodge E, Hodes M, Eisler I, et al: Family therapy for bulimia nervosa in adolescents: an exploratory study. Journal of Family Therapy 1995; 17:59-77 [Google Scholar]
- 49.Steiner H, Mazer C, Litt I: Compliance and outcome in anorexia nervosa. West J Med 1990; 153:133-139 [PMC free article] [PubMed] [Google Scholar]