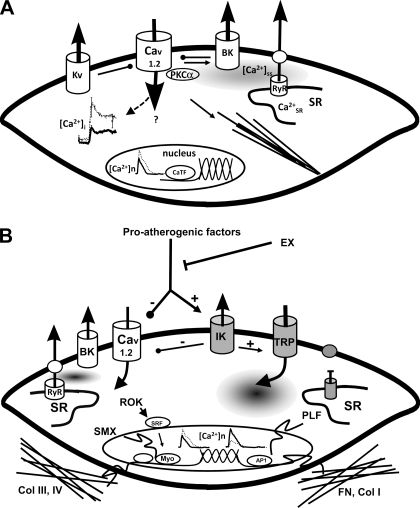
Fig. 4.
A: model of EX-induced adaptations of coronary smooth muscle (CSM) in normal subjects (boldface indicates those elements altered by EX). The left center illustrates decreased intracellular calcium concentration ([Ca2+]i) response to selective agonists (e.g., endothelin), which produces a reduced Ca2+-dependent activation of contraction. This decreased [Ca2+]i occurs despite an increased Ca2+-influx through L-type Ca2+ channels (Cav1.2), which is buffered by a non-sarcoplasmic reticulum (SR), non-Na+/Ca2+ exchanger mechanisms. Nuclear Ca2+ responses ([Ca2+]n) are similarly reduced by EX, which may affect Ca2+-dependent transcription factors (CaTF, e.g., cAMP response element-binding protein and nuclear factor of activated T cell) and target gene expression. On the top right note that EX increases spontaneous, slow-Ca2+ release from the SR into the subsarcolemmal space ([Ca2+]ss), which may contribute to the increased activation of large-conductance Ca2+-activated (BK) K+ channels by EX. In addition, Kv channels are also activated by EX. In arteriolar CSM, Ca2+-dependent PKC (e.g., PKCα) signaling enhances Cav1.2, leading to activation of contractile filaments and enhanced myogenic tone. Together, these changes result in an increase in the gain of the vasomotor contractile system and a more stable mature CSM phenotype. B: proposed model illustrating the manner in which EX may interact with proatherogenic factors, thereby decreasing lesion progression and/or stimulating lesion regression of atherosclerosis through regulation of CSM phenotype in coronary artery disease (CAD; gray, atherogenic effects). Proatherogenic factors (such as PDGF-BB, TNF-α, leptin) upregulate intermediate conductance Ca2+-activated K+ channels (KCa3.1, IK) and voltage-independent Ca2+ channels (e.g., TRP) while suppressing Cav1.2 and BK (KCa1.1) channels. CAD also disrupts SR Ca2+ release and extrusion and increases [Ca2+]n. As shown on the right, this ion channel profile switch enhances CSM synthesis of fibronectin (FN) and collagen I (Col I), leading to a more proinflammatory matrix composition and synthesis of proliferative genes (PLF). EX adaptations described in A produce a stable, noninflammatory phenotype and increased expression of collagens III and IV (Col III, IV), producing a noninflammatory matrix. Note that there are a number of similarities and differences in the effects of EX on CSM in normal and diseased states. RyR, ryanodine receptor; ROK, Rho-associated protein kinase; SMX, smooth muscle-specific gene expression; Myo, myocardin; AP1, activator protein-1.