Abstract
Social network analysis was used to examine the relationship between HIV/AIDS stigmatization, perceived risk, and centrality in the community network (via participation in community groups). The findings from respondents in Keetmanshoop, Namibia (N = 375) showed an interaction between stigma and risk perceptions: those who perceived higher HIV risk and stronger HIV stigma participated in fewer community groups and participated in groups with members who participated less widely across the network. In contrast, those who perceived higher HIV risk and weaker HIV stigma participated more, and were in community groups that are located on a greater share of the paths between entities in the network. Taboo, secrecy, resistance, knowing a person living with HIV/AIDS, and desire for diagnosis secrecy were also related to centrality. Findings suggest that the interaction of perceived HIV risk and HIV stigma are related to structural-level features of community networks based on participation in community groups.
Keywords: Stigma, Social Network, Centrality, Perceived Risk, Participation
INTRODUCTION
Stigmas are powerful social forces: they may shape interpersonal interactions as people attempt to enforce stigmas or to avoid stigmatization themselves. For example, in order to avoid stigmatization, people may conceal the features or behaviors associated with a stigmatized group [1, 2], if the categorizing marks are concealable, or regulate their social interactions by restricting interpersonal encounters to those who are likely to be supportive and avoiding everyone else [e.g., 1, 3]. Both concealment and withdrawal are likely to shape the community’s social network and people’s centrality within it (i.e., less centrality), yet the structural-level effects of stigmatization on social network centrality have not been examined. For those with complex, chronic health conditions like HIV, less central positions within network can make it difficult to obtain social or instrumental support needed to manage the condition. Indeed, stigmatization may serve as a counterpoint to people’s pragmatic inclination to obtain or maintain more central network positions when facing complex, chronic health conditions. This study, then, contributes to the literature by investigating social mechanisms associated with stigmatization of HIV. This is done in the context of the relationship between Namibian respondents’ centrality in the community network (based on their participation in social groupings) as predicted by their HIV-risk and HIV-stigma perceptions.
Stigmatization
A stigma is “a socialized, simplified, standardized image of the disgrace of a particular social group” [4, p. 455; see also 1, 5, 6]. The disgrace is associated with a community taboo (i.e., prohibited condition or action) [4]. Stigmas and associated taboos must be communicated among community members in order to be taught and enacted [4, 5, 7]. Stigma communication, then, is associated with particular objectives: to recognize those associated with the taboo and to limit their access to community resources and interpersonal encounters [4]. Thus, while stigmas are created, maintained, and diffused through communication, their existence also influences communication, such as interactions between those who are categorized as members of a stigmatized group and those who are not, whom Goffman labeled as “normals” [1, p. 5].
Interactions between stigmatized people and normals can be stressful and challenging [1]. Normals may face conflicting obligations to protect their groups (e.g., identify and exclude stigmatized members) [8], and yet not to appear appalling or sadistic in their actions [9]. Interacting with stigmatized persons is associated with feelings of uncertainty, discomfort and anxiety [10]. Normals attempt to shorten [9] or avoid [11] interactions with stigmatized people. Avoiding contact allows normals to protect their groups and their identities [7], as well as to circumvent distressing encounters [1]. At the same time, stigmatized people risk devaluation, ostracism, and discrimination [12, 13], which are associated with significant psychological pain [14, 15].
Three different strategies are used to avoid stigmatization: secrecy, education, and withdrawal [3]. Secrecy is one communication option; it entails concealing the attributes or actions that could categorize one into the stigmatized group [1, 3, 5, 16, 17]. Education is another option that entails the intentional, explicit disclosure of one’s inclusion in the stigmatized group and information about it, in an effort to change the stigma, produce acceptance, or discourage rejection [3, 18]. Withdrawal, in contrast, entails selective exposure to only those people who accept the person in spite of the stigma or who reject the stigma [1, 19]. All three coping strategies are argued to shrink stigmatized persons’ social networks. Withdrawal is self-evident. Education may lead to acceptance by the person who is hearing the disclosure, but it may also lead to rejection [20] or encouragement not to tell anyone else [21]. If acceptance is successful, then stigmatized persons are likely to stay only within the accepting network of people [12], which becomes withdrawal. Secrecy may also be more difficult to maintain with larger social networks [22]. For many reasons, people who anticipate stigmatization are likely to have restricted networks.
Restricting social networks has costs. People who maintain larger, diverse social networks can more easily gain information [23, 24], such as the name of a specialist. They can also gain instrumental and financial support, which is linked to greater access to medical care [25]. For HIV specifically, larger, more diverse social networks have been associated with slower disease progression to AIDS [26], slower decline in CD4 cells [27], slower symptom onset [26, 28], and longer survival [29]. Conversely, lack of social support has been linked to faster decline in CD4 counts during a 5-year study [27], to development of symptoms among those with lower CD4 counts [28], and to shorter survival among those with AIDS- or HIV-related symptoms [29]. Although social support has been associated with clinical outcomes, a meta-analysis showed that the HIV disclosures may lead to social support or stigmatization [20].
Here lie the fundamental tensions. For those facing a health condition like HIV, there is much to be gained by fostering and maintaining a larger, more diverse social network. If the community supports an HIV stigma, then a person living with HIV or AIDS (PLWHA) may avoid stigmatization, ostracism, and discrimination by maintaining a restricted network. The presence of an HIV stigma has been well-documented [e.g., 30], including in Namibia [e.g., 31-34], the location studied herein.
One means by which to expand or restrict one’s social network is by choosing whether to participate in community groups (e.g., clubs, teams, associations, and churches). Structurally, people may be connected through their memberships in the same community groups, and these community groups may be tied through shared members (35). Although stigmatization may also be related to people’s personal networks (e.g., friendship and sexual), group participation is central in the discussion of stigmas. Stigmas are tied inherently to group-level protection. Further, stigma reactions focus on group-level choices, such as ostracizing stigmatized persons from ‗normal’ groups (8, 13). Additionally, those facing possible stigmatization may select into small groups of those also facing the stigma (i.e., “the own”) and their supporters (i.e., the “wise”) (1). Perceptions of HIV risk and HIV stigma, together, should be associated with network characteristics, such as centrality.
Centrality in Person-Community Group Networks
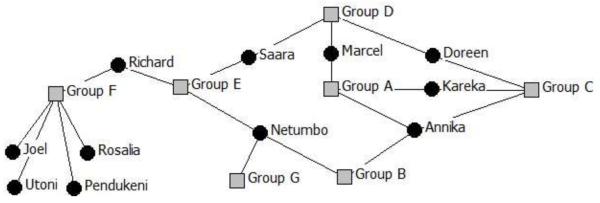
Networks featuring relationships built from people’s membership in groups may be described as two-mode networks (e.g., 36). Mode refers to a set of discrete entities in the network (36). In this two-mode network, the first mode refers to people and the second refers to social groups in the community. Social network analysis (SNA) can quantitatively represent the pattern of relationships between people and groups. Specifically, this paper focuses on the property of centrality. Centrality is a broad concept. Those anticipating stigmatization may restrict their social networks by (a) reducing their general activity in social groups or (b) selecting groups based on the activity of the other members in the social groups. These two processes are captured in three centrality estimates: degree, eigenvector, and betweenness centrality (see Figure 1 for graphical depiction).
Figure 1. A depiction of a network of people and community groups varying in centrality.
For the community groups, Group F has the highest degree centrality; Group E has the highest betweenness centrality; and Groups A and C have the highest eigenvector centrality. For people, Annika and Netumbo have the highest degree centralities; Richard has the highest betweenness centrality; and Annika has the highest eigenvector centrality.
Degree centrality in two-mode networks describes the idea that particular entities are important or visible in a network because of the number of connections they have with other entities in the network (35, 37). For people in this two-mode network, degree centrality represents the number of groups in which they participate; for groups, degree centrality represents the size of their membership. In Figure 1, Group F has the most members, and Netumbo and Annika are participating in the greatest number of groups, and consequently, have the highest degree centrality. Those restricting their participation to fewer groups, then, have smaller degree centralities.
Eigenvector centrality and betweenness centrality in a two-mode network take into account a person’s participation in community groups as well as the level of participation of other group members. Eigenvector centrality is a weighted estimate of degree centrality, such that participation in a community group with members who participate in other community groups in the network is estimated as more central than participation in community groups without shared members. Thus, people’s centrality is related to the centrality of the groups in which they are members [35, 37]. For example, although Netumbo and Annika in Figure 1 each participate in three groups, Annika has higher eigenvector centrality because she participates in groups that have more participatory members.
Betweenness centrality in a two-mode network is the share of paths between entities in the network that pass through a particular person or community group [35, 37]. Because of how people and groups are connected through co-memberships, it may be possible to share information at one community group meeting that is spread through the co-membership ties through the network system. People in community groups positioned between such paths through the social system (e.g., Richard in Figure 1) may be able to access more information and resources than those in less advantageous positions. Both eigenvector and betweenness centrality highlight that a person may not need to be an active member of many community groups to be in important, visible, or embedded positions in the social network.
Anticipating Stigmatization and Centrality
HIV can be associated with greater centrality or less centrality depending on stigma perceptions of HIV. People attempting to manage complex health conditions such as HIV can strengthen, maintain, or use their social networks [22, 38];this provides greater centrality, which affords them the social capital to manage such conditions well, if they are seen as acceptable health conditions. Such social interactions and central positions may have multiple health benefits [39]. Taboo health conditions, however, put one in the position of simultaneously managing the health condition and social taboo. This study tests whether perceiving oneself as likely to have a more taboo health condition is associated with smaller degree, eigenvector, or betweenness centrality, in order to manage stigmatization.
METHOD
Participants and Procedures
Participants were recruited from households (N = 375) immediately adjacent to a hospital located in Keetmanshoop, Namibia. The sampling started with the development of a map, listing all formal and informal households within a 10-kilometer area surrounding the Keetmanshoop State Hospital. Interviewers branched out in a circle around the hospital until they completed 375 interviews. The interviewers were local Namibians who were fluent in English and Afrikaans, as well as local languages to help respondents through the survey. Before interviews began, they attended a two-day workshop on the questionnaire, interviewing procedures, and ethical guidelines. During data collection, all interviewers were debriefed daily by a supervisor, and received additional training as needed. The interviews were conducted from morning until evening. The University of Namibia provided human subjects approval for this project.
Interviewers approached each household and asked to talk to the head of the household, explained the study, obtained an inventory of all eligible members (residents of the household age 15 and older), and then chose at random a person to be interviewed (via roll of a die). The interviewer then asked to talk to the selected person, took him/her to a private place either inside or outside of the household, and read the informed consent information, explaining that participation was voluntary and their answers were confidential. The survey was conducted orally, in order to gain information from those with low reading abilities. At the conclusion of the interview, respondents were given a household food item (e.g., small bag of rice or flour).
Respondents, on average, were 31 years of age (M = 31.35, SD = 11.17, Median = 29) and reported 10 years of education (M = 9.88, SD = 2.80). This sample over-represents adults in a young Namibian population (39% aged below 15 years) [40], and those with more years of education (M = 7.1 years in Karas region) [40]. The sample is 44% male, closely approximating gender proportions in the region (47% male) [40]. The overall prevalence of HIV when the data were collected was 18.5% in Keetmanshoop and 20% in Namibia as a whole (sero-surveys), with heterosexual sex as the predominant mode of transmission [41].
Network Centrality
Respondents were asked to name all the community groups in which they participate. Respondents could name as many groups as they liked. These community groups included sporting clubs, professional organizations, and churches. A two-mode matrix of the respondents and their community groups was created and entered into UCINET 6.232 (42). Degree, eigenvector, and betweenness centrality estimates were generated for all participants and community groups using the two-mode matrix. The centrality measures were intercorrelated; the correlations for degree and eigenvector centrality was .34; for degree and betweenness was .65, and for eigenvector and betweenness was .34. Intercorrelation among such estimates is not unusual [e.g., 43], in fact, they are usually much higher. For the purposes of exploration, the estimates were studied separately.
Independent Measures
Six independent variables were included in the study (see Table 1 for their inter-correlations). 1) Respondents indicated their perceived HIV risk on a single-item scale (0 = not at all likely [44%], 1 = possible [40%], 2 = certain to happen [16%]), M = 0.72, SD = 0.72. 2) Perceived HIV stigma was indexed with three questions about their intended interactions with PLWHAs: would they care for family member living with HIV in their household; would they buy produce from a shopkeeper with HIV; and would they want a teacher living with HIV to continue teaching. The answers were summed into a single score and coded such that higher, positive scores indicate greater stigma intentions (definitely no = 2 [3%], maybe no =1 [12%], maybe yes = −1 [30%], definitely yes = −2 [55%]; M = −1.23, SD = 1.11, α = .75). An interaction term was created from HIV risk and perceived stigma, such that those who felt at risk for HIV and perceived no stigma were coded with higher, positive scores (1 to 4), those who did not feel at risk for HIV regardless of their stigma perceptions were coded with a 0, and those who felt at risk for HIV and perceived a stigma were coded with higher, negative scores (−1 to −4).
Table 1. Inter-Item Correlations.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. HIV Risk | |||||||||
| 2. Taboo topic | −.0 2 | ||||||||
| 3. Secrecy | .04 | .16 a | |||||||
| 4. Know PLWHA | .01 | .07 | −.06 | ||||||
| 5. Stigma | .26 a | .12a | .04 | .01 | |||||
| 6. Stigma * HIV Risk | −.41 a | .14a | .03 | −.07 | .59a | ||||
| 7. Resist Stigma | −.07 | .05 | −.18 a | −.04 | −.03 | .08 | |||
| 8. Gender | .00 | .03 | .03 | −.08 | .14 a | .07 | −.08 | ||
| 9. Age | −.16 a | .02 | −.09 | .14a | −.07 | .02 | .06 | .02 | |
| 10. Education | .02 | −.12 a | .02 | .08 | .04 | .01 | .03 | −.02 | −.05 |
p < .05 one-tailed
Respondents also indicated their agreement with whether 3) HIV/AIDS is a taboo topic in their community (strongly agree = 2 [10%], somewhat agree = 1 [14%], somewhat disagree = −1 [22%], strongly disagree = −2 [54%]; M = −0.64, SD = 1.25) and 4) they would want a family member’s positive HIV diagnosis to remain a secret (definitely no = 2 [18%], maybe no= 1 [36%], maybe yes = −1 [36%], definitely yes = −2 [10%]; M = 0.15, SD = 1.34). Respondents reported whether they 5) had a personal connection to a PLWHA (−1= no [49%], 0 = unsure [4%] 1 = yes [46%]). 6) Resistance to stigma was indexed with three questions about their confidence to help a PLWHA even if their community, spouse, or peers opposed it. The answers were summed into a single score and coded such that higher scores indicate greater efficacy to resist (no confidence = 1 [4%], a little confident = 2 [22%], some confidence = 3 [42%], very confident = 4 [33%]; M = 3.03, SD = 0.83, α = .82).
Analysis Plan
To predict centrality, the three regressions were completed using permutation-based tests for standard errors and significance tests (5000 permutations per test), due to the interdependence in the data. Multiple random starting values (i.e., seeds) were used for each test, with differences appearing in the fourth or greater decimal place. Robust ANOVA tests were also completed (permutations = 5000 for significance tests).
RESULTS
Participation in the Community Network
Participants reported membership in 84 different community groups. Most people (55%) reported membership in only one community group (M = 1.15, SD =0.79, Max = 4, Min = 0.00). Six percent (n = 66) did not participate in any community groups. On average, community groups had 5 sampled respondents participating in them (M = 5.15, SD = 7.99, Max = 44, Min = 1). Five community groups, three churches, a church-related AIDS action group, and a shebeen (i.e., bar), had the highest degree, eigenvector, and betweenness centrality. The three community groups with the highest degree centrality (participation rates from the sample) were churches; 30% of the respondents participated in one of these three churches. A church-related, AIDS action group had the fourth-highest degree centrality. The churches were ranked in the top four groups, but the AIDS action group ranked higher than some of the churches by having the second-highest betweenness centrality and third-highest eigenvector centrality. A close fifth on all three centrality measures was a popular, local shebeen. The other 79 groups included churches, sport clubs, organizational groups (e.g., teacher’s association), action groups (e.g., other AIDS action groups), farmers’ associations, shebeens, youth-related groups, and arts-related groups.
Predicting Centrality
Three multiple linear regressions were completed with degree, eigenvector, and betweenness centrality for participants as the dependent variables. The independent variables included perceived HIV risk, perceived HIV stigma, perception of HIV as a taboo topic, desire for secrecy, personal connection to a PLWHA, perceived efficacy to resist an HIV stigma, interactions between perceived stigma and perceived risk, gender, age, and education. All three regressions completed to predict centrality were statistically significant (R2 = .11, .10, and .08 for degree, eigenvector, and betweenness centrality, respectively); Table 2 shows the regression estimates.
Table 2. Standardized Coefficients for Centrality Estimates.
| Degree | Eigenvector | Betweenness | |
|---|---|---|---|
|
Standardized coefficient |
Standardized coefficient |
Standardized coefficient |
|
| Perceived Risk | -0.05 | 0.10 | 0.03 |
| Taboo Topic | 0.11a | 0.18a | 0.08 |
| Secrecy | -0.13a | -0.06 | -0.15a |
| Know PLWHA | -0.09a | 0.02 | -0.08 |
| Stigma | 0.24a | 0.08 | 0.15a |
| Stigma * Risk | -0.15a | 0.01 | -0.10a |
| Resist Stigma | 0.20a | 0.05 | 0.14a |
| Gender | -0.01 | -0.07 | -0.05 |
| Age | 0.03 | 0.18a | 0.00 |
| Education | 0.01 | -0.02 | 0.00 |
| R2 | .11a | .10a | .08a |
p < .05
Note. The centrality estimates were generated from a two-mode matrix. Significance probabilities were generated from 5000 permutation-based tests (5000 permutations per test). Multiple random number seeds were used; differences were minimal (fourth decimal place). The models are all statistically significant: degree centrality, F (11, N = 375) = 4.29, p (one-tailed) = .001; eigenvector centrality, F (11, N = 375) = 3.76, p (one-tailed) =.003; betweenness centrality, F (11, N = 375) = 3.02, p (one-tailed) =.01.
The findings show that perceived HIV risk, gender, and education were not related to centrality in the community network. Respondents were likely to participate in more community groups (degree centrality) if they felt that HIV was a more taboo topic, had less desire for secrecy, knew fewer PLWHAs, perceived greater HIV stigma, and felt capable of more stigma resistance. The interaction term for perceived HIV risk and HIV stigma was also related to participation, such that those perceiving themselves more at risk for contracting stigmatized HIV were participating in fewer community groups. Older participants who perceived more of an HIV taboo were more likely to be in community groups with members with higher levels of participation in multiple community groups (eigenvector centrality). Participants were more likely to be in community groups placed between entities who are not directly connected to each other (betweenness centrality), if they had less desire for secrecy, perceived greater HIV stigma, and felt more efficacy to resist this stigma. The interaction term for perceived HIV risk and HIV stigma was also related to participation, such that those perceiving themselves more at risk for contracting stigmatized HIV had lower betweenness centrality.
The main effects for HIV stigma and its interaction with perceived risk predict centrality differently. Greater perceived HIV stigma was positively related to higher degree and betweenness centrality, but the interaction - greater perceived HIV stigma and personal risk for HIV - was negatively correlated. It is not the stigma itself, then, that predicts lower centrality, but the combined perception of its existence and personal relevance.
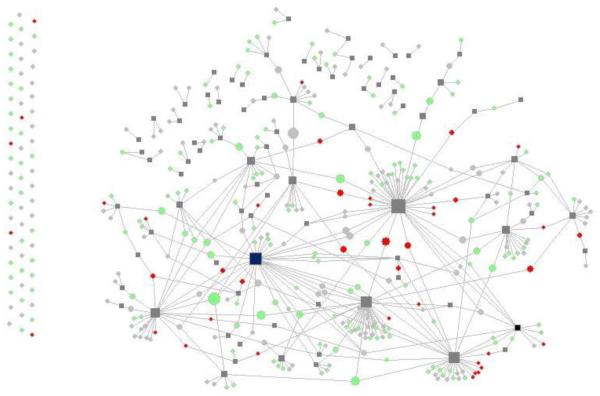
Figure 2 shows the community network, highlighting respondents’ (shown as circles) and their community groups’ (shown as squares) betweenness centrality and the risk by stigma interaction. Larger graphics (circles and squares) have higher betweenness centrality. Respondents appearing as white circles are those who feel at risk for HIV, but do not feel that there is an HIV stigma; often the white circles are the biggest ones in the network. Black circles represent respondents feeling at risk for HIV and that there is an HIV stigma; they appear smaller because they are less central in the network.
Figure 2. A depiction of the community network of Keetmanshoop.
Community groups are shown as gray squares. The lines represent self-reported participation in the group (those who are not active in social groups are depicted without lines, on the left hand side of the image). Respondents are shown as circles. The size of the community group and person varies by betweenness centrality (bigger squares and circles are more central). The color for respondents varies by their HIV risk and stigma perception (solid red feel at risk and that HIV is stigmatized; green feel at risk but HIV is not stigmatized; and light gray do not feel at risk for contracting HIV).
Participation in HIV-related Organizations
Of the 375 participants, 41 reported participating in one of two HIV/AIDS-related organizations in the area. Most participated in the church-related organization (n = 29), fewer in the secular organization (n = 11), and one person participated in both groups. In a post-hoc analysis, multiple robust ANOVA tests were completed with membership in an HIV/AIDS-related group as the independent variable and the variables in Table 1 as dependent variables in each test. No statistical differences appeared for perceived risk, desire for secrecy, connection to a PLWHA, perceived HIV stigma, or the stigma by risk interaction. There were differences in perceived HIV taboo (F[1, 373] = 7.49, p < .05, R2 = .02) and stigma resistance (F[1, 373] = 14.04, p < .05, R2 = .04). Those participating in an HIV/AIDS-related group perceived a stronger HIV taboo (M = −0.15, SD = 1.35) compared to those who did not participate in such community groups (M = −0.71, SD = 1.22). Those participating in an HIV/AIDS-related group also reported greater ability to resist an HIV-stigma(M = 3.49, SD = 0.60) compared to those who did not participate in such community groups (M = 2.98, SD = 0.84). The ANOVAs were calculated with church membership as the independent variable and no statistically significant differences were found in these variables.
DISCUSSION
This study investigated people’s combined perceptions of risk for contracting HIV and of an HIV stigma, as they relate to their centrality in a community network in Namibia built through participation in community groups. The findings showed that people who perceived both greater HIV risk and greater HIV stigma participated in fewer community groups and participated in community groups with members who participated less widely across the network. In contrast, those who perceived greater HIV risk but less HIV stigma participated more, and were in community groups that were located on a greater share of the paths between entities in the network. The combination of perceptions—risk and stigma—is related to structural-level features of the community network, built from participation in community groups.
Push and Pull
As suggested by others, anticipating or having a health condition may encourage people to seek support, which may come through community groups. Perceived HIV risk alone was not predictive of centrality, suggesting that risk alone may motivate action, but the action may be moderated by the social risk carried by the condition. The findings here support the notion [1, 12, 44] that those facing a stigmatized condition may forego the benefits of a large, diverse network for a smaller one restricted to similar connections, which manifests as lower degree and betweenness centrality.
In addition, those who knew a PLWHA and desired greater secrecy about a family member’s HIV-positive diagnosis showed lower degree and betweenness centrality. Those who know a PLWHA may find themselves facing what Goffman [1] calls a courtesy stigma, or stigma by association [16, 45], which is when the community extends stigmatization to those associated with or sympathetic to the stigmatized. In reaction to the extended stigma, associated persons may also be found in smaller, more selected parts of the community network. The desire for family secrecy, then, may be a means by which to address the stigma-by-association. On the other hand, the causality may be reversed: those participating in fewer community groups may be aware of and not want to risk their weak, potentially vulnerable social positions by providing possible reasons for ostracism. Chronically ostracized persons may be especially alert to the prospect of rejection, because chancing risky interactions could lead to the painful consequence of total social exclusion [46]. The pain that results from ostracism [46] has been shown to be resistant to moderating factors such as trait self-esteem [47] and social anxiety [48]; therefore, regardless of a person’s individual characteristics, ostracism is associated with immediate and painful consequences [46] that may motivate vulnerable persons to protect their position in fewer social groups as a strategy to avoid complete social exclusion.
The main effects for perceived HIV stigma and centrality, which were positive, support the argument that people may be able to attain and retain their centrality in the network through participation in community groups if they have greater knowledge of the stigma and fewer connections to those associated with it.
Tensions at the Center
Taboo, stigma, and resistance were related to centrality. Those who felt that HIV was more taboo had higher degree and eigenvector centrality; as participants perceived a stronger HIV taboo, they were active in more community groups and participated in more central, well-connected community groups. Also, stronger perception of HIV/AIDS stigma was associated with higher degree and betweenness centrality. To date, scholars have argued that, as a socialized phenomenon, everyone is aware of a stigma [2, 49]; no one has suggested that a particular community group may have stronger stigma beliefs or attitudes. Brewer and Caporael [50] point out that there are advantages for community group members who reject those who are deviant, which may be why rejecters may be more central. Those who share stigma communication more frequently may benefit from the in-group bonding that comes from sharing stigma messages [4, 5]. Reasons for a stronger stigma at the center remain unclear; pragmatically, though, this finding suggests that leader-based initiatives using social members as the basis of leadership may have difficulty finding champions [51] to distribute HIV-related messages without the stigma. On the other hand, those who reported greater efficacy to resist the HIV stigma also had higher degree and betweenness centrality, so the situation may not be so bleak. As pointed out by an anonymous reviewer, one AIDS-related group had high betweenness centrality, providing it a strategic placement in the community, even though it did not have many members. These members also reported confidence in their ability to resist an HIV stigma. This organization’s members could be influential in spreading stigma resistance through the community. The tensions between socialized stigma and efficacy to resist it are likely to play out in the social dynamics of community group participation, and should be pursued in future research.
One may also note that the community groups with the highest centrality were churches, a church-affiliated AIDS action group, and shebeens (i.e., bars). Although central, these organizations may interface differently with HIV/AIDS interventions. Second, of those reporting participation in a community group, respondents with the highest perceptions of both HIV risk and stigma participated in a church, an HIV-prevention club, or a shebeen. It may be useful to better understand the role that such organizations play in the social life of a community and those living with HIV.
Participation in HIV/AIDS-related community groups
Over 15% (n = 60) of the respondents believed that they were certain to contract HIV, but only four of them reported participation in one of two HIV/AIDS-related organizations. In total, 11% (n = 41) of the respondents reported participation in these two community groups. The findings showed that those participating in the HIV/AIDS-related organization reported stronger beliefs in HIV/AIDS as a taboo topic and greater efficacy to resist the HIV/AIDS stigma. That said, on average, those who participated in the HIV/AIDS-related community groups were not different from those who did not participate in terms of HIV risk, the risk by stigma interaction, secrecy desires, or knowing PLWHAs. It is possible that both those who need such organizations (e.g., PLWHA) and those sympathetic to HIV/AIDS (i.e., the “wise”) may participate in HIV/AIDS-related organizations. Participating in such a community group may also associate someone with HIV/AIDS, which may limit participation if that association is stigmatized. It is interesting that with only two such organizations reported, only one person reported participation in both community groups. Inter-organizational collaboration and cooperation may be an important consideration for future activities.
Uncovering mechanisms that may increase stigma resistance, such as participation in the HIV/AIDS-related groups, is important. Table 1 shows that the ability to resist the HIV/AIDS stigma and desire to keep family member diagnoses secret were negatively related. If individuals believe they can resist stigma, secrecy may not be seen as necessary. Because secrecy has damaging effects on individuals’ social networks [3, 21] and, therefore, life chances [1, 29], future research should focus on the possible relationship between efficacy to resist stigma and desire for secrecy.
Of note, the correlations (Table 1) showed that there was not an association between knowing PLWHAs and desires for secrecy, taboo perceptions, risk perceptions, stigma beliefs, or resistance efficacy. Contact with PLWHA, in and of itself, does not seem to influence perceived HIV risk, HIV stigma, or stigma resistance, which conflicts with interventions aiming to use contact to reduce stigma [e.g., 52, 53].
Social and Individual Factors in HIV/AIDS Stigma
Social networks play a role in generating and sustaining stigmas [4, 5]. This study showed the association between stigma and positions in a community network, and thus the potential for stigma to shape social networks. Because stigma is socially constructed [1, 4, 5], understanding the social structures that influence its communication may be important for stigma-reduction efforts. Much research has emphasized stigma’s impact on those enacting or experiencing stigmatization [54]. Although this research has provided important insights regarding stigma, an exclusively person-centered focus may overlook vital societal mechanisms [54]. Social network analysis provides an opportunity to consider relationships at many social scales and evaluate their role in effective stigma-reduction campaigns.
Limitations
The findings are limited. First, causality should not be inferred from these cross-sectional data. Social patterns may be explained by the fact that people tend to cluster together due to physical proximity [55]: those who live further away [55] or in areas of social stratification [56] may have fewer chances to interact with others and participate in community groups. Second, measurement error increases with small networks [57]; this limits these data and also provides a serious challenge to studies of stigmatization and related processes, such as ostracism and isolation. Third, stigma is a multifaceted concept [6]. The measures in this study focused more on social distance and taboo, and less on character judgments or responsibility. Moreover, research has shown that differences in the form of and perception of ostracism, social exclusion, and rejection lead to a variety of social behaviors including attempts to rejoin community groups, to leave situations, and to garner attention through anti-social means [46]. As pointed out by an anonymous reviewer, membership in some groups may preclude participation in another (e.g., membership in a fundamental religious organization may limit involvement in other groups). Further attention to details in the forms and meaning of stigma-related community group exclusion and inclusion, and their influence on structural-level dynamics, is an important avenue for future research [46].
The status of HIV treatment and services available at the time of the study may also shape these findings. Better distribution of anti-retrovirals and expanded services for PLWHAs (including preventing mother-to-child transmission) were both challenges for Namibia, especially to people outside of the capital [41]. Collaborations among hospitals and community-based organizations, such as church-based AIDS action committees, may have developed to meet these challenges; their existence was applauded and encouraged [41]. In addition, participants’ HIV status (e.g., test results) was not known, but it is unlikely that their perceptions and status were perfectly correlated [58]. Although perception was considered focal in this study because of its relationship to stigma [1], it is important to consider the role of actual test results in future studies.
CONCLUSIONS
By using social network analysis involving both individuals and community groups, this study showed that perceptions of HIV risk and HIV stigma may be related structurally to people’s participation in community groups. The benefits of larger, more diverse social networks and health outcomes are well-established [39], but these networks may also provide opportunities for exploitation, isolation, loneliness, and conflict [59]. What is not well understood is whether and how one can optimize the size and character of a social network so that it provides the breadth and depth of support that is beneficial without harm [57]. For example, health discussion networks comprised of strong, accessible ties [60] influence a number of health outcomes [22]. Understanding how to best facilitate access to such health discussion networks via interpersonal or social means is critical for developing effective interventions to improve health behaviors and quality of life through social networks.
ACKNOWLEDGMENTS
Our thanks to Erna Keulder, Research Facilitation Services (Windhoek, Namibia), and JHUCCP/Namibia, and colleagues at the Methodology Center. This project was supported by Award Number P50-DA010075-15 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health. The data was collected with primary support from the United States Agency for International Development under the Health Communication Partnership project (GPH-A-02-00008-00) based at Johns Hopkins/Bloomberg School of Public Health/Center for Communication Programs. Most importantly, we are grateful to the leaders and citizens of Keetmanshoop for sharing their thoughts with us.
REFERENCES
- 1).Goffman E. Stigma: Notes on the management of spoiled identity. Prentice Hall; Englewood Cliffs, NJ: 1963. [Google Scholar]
- 2).Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: an empirical assessment. Am Sociol Rev. 1989;54:400–423. [Google Scholar]
- 3).Link BG, Mirotznik J, Cullen FT. The effectiveness of stigma coping orientations: can negative consequences of mental illness labeling be avoided? J Health Soc Behav. 1991;32:302–320. [PubMed] [Google Scholar]
- 4).Smith RA. Stigma communication and health. In: Thompson TL, Parrott R, Nussbaum J, editors. Handbook of health communication. 2nd ed Taylor Francis; London, UK: 2011. pp. 455–468. [Google Scholar]
- 5).Smith RA. Language of the lost: an explication of stigma communication. Commun Theor. 2007;17:462–485. [Google Scholar]
- 6).Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–385. [Google Scholar]
- 7).Neuberg SL, Smith DM, Asher T. Why people stigmatize: aoward a biocultural framework. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. Guilford Press; New York: 2000. pp. 31–60. 2000. [Google Scholar]
- 8).Cottrell CA, Neuberg SL. Different emotional reactions to different groups: a sociofunctional threat-based approach to ‘prejudice. J Pers Soc Psychol. 2005;88:770–789. doi: 10.1037/0022-3514.88.5.770. [DOI] [PubMed] [Google Scholar]
- 9).Thompson TL, Seibold DR. Stigma management in “normal”-stigmatized interactions: test of the disclosure hypothesis and a model of stigma acceptance. Hum Commun Res. 1978;4:231–242. [Google Scholar]
- 10).Kelly HH, Hastorf AH, Jones EE, Thibaut JW, Usdane WM. Some implications of social psychological theory for research on the handicapped. In: Lofquist LH, editor. Psychological research and rehabilitation. American Psychological Association; Washington, DC: 1960. pp. 172–204. [Google Scholar]
- 11).Thompson TL. Gaze toward and avoidance of the handicapped: A field experiment. J Nonverbal Behav. 1982;6:188–196. [Google Scholar]
- 12).Link BG, Cullen FT, Frank J, Wozniak JF. The social rejection of former mental patients: understanding why labels matter. Am J Sociol. 1987;92:1461–1500. [Google Scholar]
- 13).Williams KD. Social ostracism. In: Kowalski RM, editor. Aversive interpersonal behaviors. Plenum Press; New York: 1997. pp. 133–170. [Google Scholar]
- 14).Goodwin SA, Williams KD, Carter-Sowell AR. The psychological sting of stigma: the costs of attributing ostracism to racism. J Exp Soc Psychol. 2010;46:612–618. [Google Scholar]
- 15).Williams KD, Shore WJ, Grahe JE. The silent treatment: perceptions of its behaviors and associated feelings. Group Process Interg. 1998;1:117–141. [Google Scholar]
- 16).Herek GM. Why tell if you’re not asked? Self-disclosure, intergroup contact, and heterosexuals’ attitudes toward lesbians and gay men. In: Herek J, Jobe GM, Carney R, editors. Out in force: sexual orientation and the military. University of Chicago Press; Chicago: 1996. pp. 197–225. [Google Scholar]
- 17).Jones EE, Farina A, Hastorf AH, Markus H, Miller DT, Scott RA. Social stigma: the psychology of marked relationships. W. H. Freeman and Company; New York: 1984. [Google Scholar]
- 18).Peters KF, Apse KA, Blackford A, McHugh B, Michalic D, Biesecker BB. Social and behavioral research in clinical genetics. Living with Marfan syndrome: coping with stigma. Clin Genet. 2005;68:6–14. doi: 10.1111/j.1399-0004.2005.00446.x. [DOI] [PubMed] [Google Scholar]
- 19).Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. On describing and seeking to change the experience of stigma. Psychiatric Rehabilitation Skills. 2002;6:201–231. [Google Scholar]
- 20).Smith RA, Rossetto K, Peterson BL. A meta-analysis of perceived stigma, disclosure of one’s HIV + status, and perceived social support. AIDS Care. 2008;20:1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- 21).Smith RA, Hipper T. Label management: investigating how confidants encourage the use of communication strategies to avoid stigmatization. Health Commun. 2010;25:410–422. doi: 10.1080/10410236.2010.483335. [DOI] [PubMed] [Google Scholar]
- 22).Perry BL, Pescosolido BA. Functional specificity in discussion networks: the influence of general and problem-specific networks on health outcomes. Soc Networks. 2010;32:345–357. [Google Scholar]
- 23).Granovetter MS. The strength of weak ties. Am J Sociol. 1973;78:1360–1380. [Google Scholar]
- 24).Schaeffer C, Coyne J, Lazarus R. The health related functions of social support. J Behav Med. 1981;4:381–406. doi: 10.1007/BF00846149. [DOI] [PubMed] [Google Scholar]
- 25).Knowlton AR, Hua W, Latkin C. Social support networks and medical service use among HIV positive injection drug use: Implications for intervention. AIDS Care. 2005;17:479–492. doi: 10.1080/0954012051233131314349. [DOI] [PubMed] [Google Scholar]
- 26).Leserman J, Petitto JM, Gu H, et al. Progression to AIDS, a clinical AIDS condition and mortality: psychosocial and physiological predictors. Psychol Med. 2002;32:1059–1073. doi: 10.1017/s0033291702005949. [DOI] [PubMed] [Google Scholar]
- 27).Theorell T, Blomkvist V, Jonsson H, Schulman S, Berntorp E, Stigendal L. Social support and the development of immune function in human immunodeficiency virus infection. Psychosom Med. 1995;57:32–36. doi: 10.1097/00006842-199501000-00005. [DOI] [PubMed] [Google Scholar]
- 28).Solano L, Costa M, Salvati S, Coda R, Aiuti F, Mezzaroma I, Bertini M. Psychosocial factors and clinical evolution in HIV-1 infection:A longitudinal study. J Psychosom Res. 1993;37:39–51. doi: 10.1016/0022-3999(93)90122-v. [DOI] [PubMed] [Google Scholar]
- 29).Patterson TL, Shaw WS, Semple SJ, Cherner M. Relationship to psychosocial factors to HIV disease progression. Ann Behav Med. 1996;18:30–39. doi: 10.1007/BF02903937. [DOI] [PubMed] [Google Scholar]
- 30).Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States:Prevalence and trends, 1991-1999. Am J Public Health. 2002;92:371–377. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31).Fay, Baral H, Trapence SD, Motimedi G, Umar F, Iipinge E, Beyrer S, Stigma C. health care access, and HIV knowledge among men who have sex with men in Malawi, Namibia, and Botswana. AIDS Behav. 2011;15:1088–1097. doi: 10.1007/s10461-010-9861-2. [DOI] [PubMed] [Google Scholar]
- 32).Ruiz-Casares M. Kin and youths in the social networks of youth-headed households in Namibia. J Marriage Fam. 2010;72:1408–1425. [Google Scholar]
- 33).Smith RA, Ferrara M, Witte K. Social sides of health risks:stigma and collective efficacy. Health Commun. 2007;21:55–64. doi: 10.1080/10410230701283389. [DOI] [PubMed] [Google Scholar]
- 34).Thomas F. Stigma, fatigue, and social breakdown:Exploring the impacts of HIV/AIDS on patient and caregiver well-being in the Caprivi region, Namibia. Soc Sci Med. 2006;63:3174–3187. doi: 10.1016/j.socscimed.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 35).Faust K. Centrality in affiliation networks. Soc Networks. 1997;;19:157–191. [Google Scholar]
- 36).Wasserman S, Faust K. Social Network Analysis. Cambridge University; Cambridge, UK: 1994. [Google Scholar]
- 37).Borgatti SP, Everett MG. Network analysis of 2-mode data. Soc Networks. 1997;19:243–269. [Google Scholar]
- 38).Goldsmith DJ, Albrecht TL. Social support, social networks, and health: A guiding framework. In: Thompson TL, Parrott R, Nussbaum J, editors. Handbook of health communication. Taylor Francis; London (UK): 2011. pp. 335–348. [Google Scholar]
- 39).Luke DA, Harris JK. Network analysis in public health: history, methods, and applications. Annu Rev Public Health. 2007;28:69–93. doi: 10.1146/annurev.publhealth.28.021406.144132. [DOI] [PubMed] [Google Scholar]
- 40).Ministry of Health and Social Services (MoHSS) [Namibia] and Macro International Inc. (Macro) Windhoek, Namibia and Calverton. MoHSS and Macro; Maryland, USA: 2008. Namibia Demographic and Health Survey 2006-07. [Google Scholar]
- 41).Family Health International . Namibia final report September 2000-2007 for USAID’s implementing AIDS prevention and care (IMPACT) project. Family Health International; Arlington,VA: 2007. http://www.fhi.org/NR/rdonlyres/ex6yvg457j57s72yee6ve35u664rzz7ke7t4vr53v7zy24fwerymkhtjxrnqpufo747kotjefvvufk/IMPACTNamibiaFinalReportHV.pdf. [Google Scholar]
- 42).Borgatti SP, Everett MG, Freeman LC. UCINET 6 for Windows:Software for social network analysis. Analytic Technologies; Harvard, MA: 2002. [Google Scholar]
- 43).Valente TW, Coronges K, Lakon C, Costenbader E. How correlated are network centrality measures? Connect (Tor) 2008;28:16–26. [PMC free article] [PubMed] [Google Scholar]
- 44).Shelley GA, Bernard HR, Killworth P, Johnsen E, McCarty C. Who knows your HIV status? What HIV+ patients and their network members know about each other. Soc Networks. 1995;17:189–217. [Google Scholar]
- 45).Ogunmefun C, Gilbert L, Schatz E. Older female caregivers and HIV/AIDS-related secondary stigma in rural South Africa. J Cross Cult Gerontol. 2011;26:85–102. doi: 10.1007/s10823-010-9129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46).Williams KD. Ostracism. Annu Rev Psychol. 2007;58:425–452. doi: 10.1146/annurev.psych.58.110405.085641. [DOI] [PubMed] [Google Scholar]
- 47).Leary MR, Haupt AL, Strausser KS, Chokel JT. Calibrating the sociometer: the relationship between interpersonal appraisals and state self-esteem. J Pers Soc Psychol. 1998;74:1290–99. doi: 10.1037//0022-3514.74.5.1290. [DOI] [PubMed] [Google Scholar]
- 48).Zadro L, Boland C, Richardson R. How long does it last? The persistence of the effects of ostracism in the socially anxious. J Exp Soc Psychol. 2006;42:692–697. 2006. [Google Scholar]
- 49).Link B. Understanding labeling effects in the area of mental disorders: an assessment of the effects of expectations of rejection. Am Sociol Rev. 1987;52:96–112. [Google Scholar]
- 50).Brewer MB, Caporael LR. Selfish genes vs. selfish people: sociobiology as origin myth. Motiv Emotion. 1990;14:237–243. [Google Scholar]
- 51).Rogers EM. Diffusion of innovations. 5th edition Free Press; New York: 2005. [Google Scholar]
- 52).Link BG, Cullen FT. Contact with the mentally ill and perceptions of how dangerous they are. J Health Soc Behav. 1986;27:289–302. [PubMed] [Google Scholar]
- 53).Phelan JC, Link BG. Fear of people with mental illnesses: the role of personal and impersonal contact and exposure to threat or harm. J Health Soc Behav. 2004;45:68–80. doi: 10.1177/002214650404500105. [DOI] [PubMed] [Google Scholar]
- 54).Yang HL, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med. 2006;64:1524–1535. doi: 10.1016/j.socscimed.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 55).Sias PM. Social ostracism, cliques, and outcasts. In: Lutgen-Sandvik P, Davenport-Sypher B, editors. Destructive organizational communication: processes, consequences, and constructive ways of organizing. Routledge; New York: 2009. pp. 145–163. [Google Scholar]
- 56).Sampson RJ, Raudenbush SW. Seeing disorder: neighborhood stigma and the social construction of “broken windows. Soc Psychol Quart. 2004;67:319–342. [Google Scholar]
- 57).Carter WC, Feld SL. Principles relating social regard to size and density of personal networks, with applications to stigma. Soc Networks. 2004;26:323–329. [Google Scholar]
- 58).Aulagnier M, Janssens W, De Beer I, et al. 2011 Incidence of HIV in Windhoek, Namibia: demographic and socio-economic associations. PLoS ONE. 6(10):e25860. doi: 10.1371/journal.pone.0025860. doi:10.1371/journal.pone.0025860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59).Cohen S. Social relationships and health. Am Psychol. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 60).Wellman B. Partners in illness: Who helps when you are sick? In: Kelner M, Wellman B, Pescosolido BA, Saks M, editors. Complementary and alternative medicine: challenge and change. Harwood Academic Publishers; Amsterdam, Netherlands: 2000. pp. 143–162. [Google Scholar]