Abstract
A 72-year-old woman presented with first onset of seizure with no prior history of cognitive dysfunction. EEG revealed focal non-convulsive status epilepticus. MRI brain showed a left temporal non-enhancing lesion. Temporal pole biopsy showed acute neuronal necrosis and astrocyte hyperplasia together with extensive amyloid plaques and neurofibrillary tangles. Perivascular oligodendroglial hyperplasia was present. Postmortem examination revealed extensive plaque and tangle disease. Perivascular oligodendroglial hyperplasia was limited to the left temporal area. The presence of focal perivascular oligodendroglial hyperplasia in the left temporal cortex, combined with extensive plaque and tangle disease may have contributed to the focal status epilepticus in this patient. Although the presence of focal perivascular oligodendroglial hyperplasia has been reported in cases of temporal lobe epilepsy, it has not been reported as a cause of seizure in patients with Alzheimer’s disease previously. Further studies for clinical-pathologic correlation would be required to confirm this hypothesis.
Background
Although the presence of focal perivascular oligodendroglial hyperplasia has been reported in cases of temporal lobe epilepsy, it has not been reported as a cause of seizure in patients with Alzheimer’s disease (AD) previously. This is the first case report bringing to light such a pathologic correlation. Hence we felt it is important to report the same. Also early undiagnosed AD may present as status epilepticus with focal features on EEG and we believe that it is important to bear this in mind when reviewing older patients with no prior confirmed cognitive decline, with new onset of status epilepticus.
Case presentation
A 72-year-old lady presented with two generalised tonic clonic seizures. During the seizure, she made a strange sound, grabbed her left shoulder with her right arm and had a generalised convulsion which lasted for 1 to 2 min. For the previous 12 months, she had recurrent episodes of strange tastes and smells, followed by brief jerking of her right upper limb without loss of consciousness.
There was no prior history of seizures. She had a background history of hypertension, vitamin B12 deficiency and depression and underwent permanent pacemaker insertion in 2008 for symptomatic bradycardia. Medications included bendroflumethiazide, citalopram, lisinopril and lanzoprazole. Before admission, she lived alone and was independent in her activities of daily living.
On initial clinical assessment, the patient was afebrile and drowsy and did not have any rash or nuchal rigidity. Right-sided facial weakness and a right hemiparesis with power of 2/5 was present. Right plantar was upgoing and her eyes were deviated to the left.
Investigations
Full blood count, renal and liver function tests were normal. CT brain did not show any focal lesion. Cerebrospinal fluid (CSF) examination showed four white cells, protein 45 mg/dl, glucose7.8 mmol/l with plasma glucose of 11 mmol/l. EEG showed left hemispheric focal non-convulsive status epilepticus.
Vitamin B12, folate and thyroid function tests were normal. Autoantibody screen, antiglutamic acid decarboxylase antibodies and voltage-gated potassium channel antibodies were negative. CSF viral and bacterial PCR were negative. CT thorax, abdomen and pelvis was normal.
Repeat EEG showed continued focal non-convulsive status epilepticus.
MRI brain demonstrated a left-sided non-enhancing lesion in the temporal lobe.
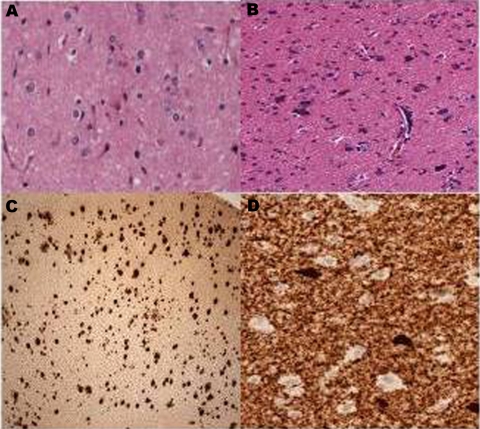
Biopsy of this area showed acute neuronal necrosis and astrocyte hyperplasia together with extensive amyloid plaques and neurofibrillary tangles but no evidence of encephalitis. Perivascular oligodendroglial hyperplasia was also present (figure 1).
Figure 1.
Pathological findings of left temporal biopsy. (A) Astrocytic hyperplasia; (B) Perivascular oligodendrocyte hyperplasia; (C) Plaques-CERAD stage C; (D) Tau positive tangles and neuropil threads (from left to right).
Treatment
Intravenous phenytoin and acyclovir were commenced on the day of admission. Since her EEG and clinical condition showed no change with phenytoin, levetiracetam was added. That also showed no beneficial effect.
Outcome and follow-up
The patient continued to be drowsy and confused.
A percutaneous gastrostomy tube was inserted due to the high risk of aspiration. Three days postinsertion, the tube dislodged and acute peritonitis developed. An emergency laparotomy with peritoneal lavage was carried out but she died shortly thereafter.
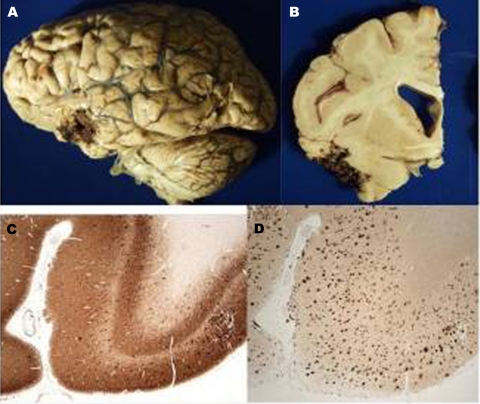
Postmortem examination showed extensive plaque (Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) C) and tangle disease (Braak VI) in all areas of the brain. Perivascular oligodendroglial hyperplasia was limited to the left temporal area (figure 2). The biopsy site showed normal reparative change.
Figure 2.
Postmortem pathological findings. (A) Gross pathology showing temporal biopsy site; (B) Left temporal biopsy site; (C) Left hippocampal section-CA1 region preserved; (D) βA4 stain-CERAD stage C plaques (from left to right).
There was no selective damage to the CA1 region of the hippocampus in this patient.
Discussion
Accumulation of β amyloid plaques causing selective destruction of the CA1 region of the hippocampus thereby damaging GABAergic circuits and altering the balance between excitatory and inhibitory pathways in the hippocampus, as seen in familial AD, thus could not be applied to our patient,1 as her brain showed no selective damage to CA1 region of hippocampus.
Two previously reported patients had complex partial seizures that preceded any cognitive decline in AD but the accumulation of plaques and tangles was focal and corresponded to the focality of their seizures.2 Our patient had generalised plaques of CERAD C category with Braak VI tangles in all areas including the neocortex bilaterally.
The presence of focal perivascular oligodendroglial hyperplasia in the left temporal cortex, combined with extensive plaque and tangle disease may have contributed to the focal status epilepticus in our patient. Although the presence of focal perivascular oligodendroglial hyperplasia has been reported in cases of temporal lobe epilepsy,3 it has not been reported as a cause of seizure in patients with AD previously.
To our knowledge this is the first case of perivascular oligodendroglial hyperplasia occurring in conjunction with Alzheimer pathology. Since this is a first case report proposing a new hypothesis, larger clinic pathologic correlation studies would be required to confirm this hypothesis.
Learning points.
-
▶
Early undiagnosed AD may present as status epilepticus with focal features on EEG.
-
▶
It is important to bear this in mind when reviewing older patients with new onset of status epilepticus.
-
▶
Focal cortical perivascular oligodendroglial hyperplasia in combination with plaques and tangles may be causative in the seizure pathophysiology in these cases.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Mendez MF, Catanzaro P, Doss RC, et al. Seizures in Alzheimer’s disease: clinicopathologic study. J Geriatr Psychiatry Neurol 1994;7:230–3 [DOI] [PubMed] [Google Scholar]
- 2.Armon C, Peterson GW, Liwnicz BH. Alzheimer’s disease underlies some cases of complex partial status epilepticus. J Clin Neurophysiol 2000;17:511–8 [DOI] [PubMed] [Google Scholar]
- 3.Kasper BS, Paulus W. Perivascular clustering in temporal lobe epilepsy: oligodendroglial cells of unknown function. Acta Neuropathol 2004;108:471–5 [DOI] [PubMed] [Google Scholar]