Abstract
Objective
To support collaboration and clinician-targeted decision support, electronic health records (EHRs) must contain accurate information about patients’ care providers. The objective of this study was to evaluate two approaches for care provider identification employed within a commercial EHR at a large academic medical center.
Methods
We performed a retrospective review of EHR data for 121 patients in two cardiology wards during a four-week period. System audit logs of chart accesses were analyzed to identify the clinicians who were likely participating in the patients’ hospital care. The audit log data were compared with two functions in the EHR for documenting care team membership: 1) a vendor-supplied module called “Care Providers”, and 2) a custom “Designate Provider” order that was created primarily to improve accuracy of the attending physician of record documentation.
Results
For patients with a 3–5 day hospital stay, an average of 30.8 clinicians accessed the electronic chart, including 10.2 nurses, 1.4 attending physicians, 2.3 residents, and 5.4 physician assistants. The Care Providers module identified 2.7 clinicians/patient (1.8 attending physicians and 0.9 nurses). The Designate Provider order identified 2.1 clinicians/patient (1.1 attending physicians, 0.2 resident physicians, and 0.8 physician assistants). Information about other members of patients’ care teams (social workers, dietitians, pharmacists, etc.) was absent.
Conclusions
The two methods for specifying care team information failed to identify numerous individuals involved in patients’ care, suggesting that commercial EHRs may not provide adequate tools for care team designation. Improvements to EHR tools could foster greater collaboration among care teams and reduce communication-related risks to patient safety.
Keywords: Provider communication, care team, electronic health records, health information technology, patient care team
1. Introduction
Caring for hospitalized patients is a collaborative process. In academic settings, the process involves multidisciplinary teams that may include attending and consulting physicians, resident physicians, medical students, nurses, nurse practitioners, physician assistants, physical and occupational therapists, social workers, and others. Achieving effective communication and collaboration within teams is a challenging task [1]. A study by McKnight et al. found that identifying the appropriate care providers for hospital patients was perceived as the most pressing communication need for both physicians and nurses [2]. Because effective collaboration is difficult to achieve using electronic health records (EHRs), clinicians resort to time-consuming “work-arounds” such as maintaining duplicate paper records [3, 4].
Through the 2009 American Recovery and Reinvestment Act (ARRA), financial incentives are available to Medicare and Medicaid providers in the United States who achieve “meaningful use” of EHRs [5]. Stage 2 of meaningful use (currently in draft form and intended to go into effect in 2013–2014) requires EHRs to have a list of care team members available for at least 10% of patients [6].While 10% may appear to be a low percentage, previous efforts to specify care team membership using health information technology have been neither comprehensive nor widely adopted [7–10].
Computer applications can support team collaboration by displaying the availability of each member [11, 12] and facilitating communication via instant messaging [13, 14]. Previous research on computer-supported team coordination has examined the formation and maintenance of teams [16, 17] and the notion of activities as long-term, joint endeavors with shared goals [18, 19]. An underlying assumption of computerized collaboration tools is the ability to maintain a comprehensive and accurate list of team members working on shared tasks. Maintaining the list is accomplished through explicit designation by managers or team members. Among other benefits, an accurate electronic listing of team members enables individuals to readily identify collaborator availability and initiate synchronous or asynchronous communication using email, text messaging, or telephony [13]. Specific to hospital settings, an accurate list of patients’ care team members in the EHR would facilitate:
-
1.
improved communication among the care team [9],
-
2.
targeted clinical decision support, such as critical laboratory test results being automatically routed to the appropriate clinician [10], and
-
3.
the sharing of care team information with patients, thus improving patient satisfaction and engagement [20, 21].
While computerized collaboration tools are desirable for patient care teams in the hospital environment, they have not been widely adopted. One reason for the lack of adoption may be the difficulty of identifying care team members in EHRs. The objective of this study was to evaluate the completeness of two approaches for care provider identification employed within a commercial EHR at an urban academic medical center.
2. Methods
We examined two approaches for identifying members of patient care teams within a commercial EHR. The EHR (Eclipsys Sunrise, Allscripts Corp., Chicago, IL) had been in use since 2004 at the study site, a large urban academic medical center. Clinicians used the EHR for order entry, results review, and electronic documentation. The study was conducted with data from patients in two cardiology wards who had a hospital stay lasting from 3–5 days during a four-week period in April 2010. Cardiology wards were used because both medical and surgical patients are cared for there, and the complexity of care teams for these patients was thought to be comparable to other areas of the medical center (excluding settings such as intensive care and labor and delivery). The majority of patients on the wards stayed between 3 and 5 days. Institutional Review Board approval was obtained prior to conducting the study.
EHR audit logs have previously been examined to detect patterns of EHR use [22, 23]. In our study, audit logs were used to identify the individuals that accessed each patient’s chart during a hospitalization. While accessing a chart does not necessarily imply care team membership, we used this as a surrogate measure to compare against existing processes for care team designation in the EHR. For this study, we assumed a clinician accessing a patient’s chart for greater than one minute during the hospitalization to be part of the care team.
The audit log data were compared with two methods for identifying team members in the EHR:
-
1.
a “Care Providers” module that was part of the standard EHR software; and
-
2.
a custom “Designate Provider” order that was entered in the computerized provider order entry module of the EHR.
Use of the Care Providers module and the Designate Provider order was assessed by measuring the average number of individuals specified for each type of clinician (e.g., physician, nurse, social worker).
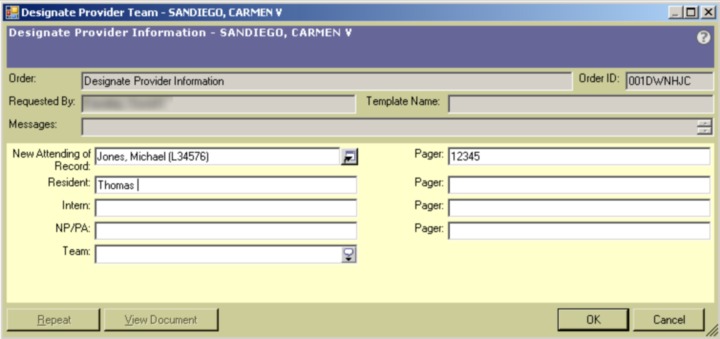
The Care Providers module (►Figure 1) could be accessed by clicking an icon from the main screen in the EHR or by clicking a link in the “Patient Info” section of the electronic chart. The module allowed users to record the name of each individual participating in a patient’s care according to the Care Provider Type and Care Provider Role. The types of care providers that could be specified included: Dietitian, Medical Student, Nurse, Nurse Practitioner, Physician Assistant, Physician, Physical/Occupational Therapist, Respiratory Therapist, and Social Worker. Specific roles could be assigned to some clinician types. For example, Physician roles included Attending, Resident, Fellow, Intern, and Consulting. The Care Providers module was accessible to all clinicians but its use was not mandatory.
Fig. 1.
EHR “Care Providers” interface for specifying clinicians caring for a patient.
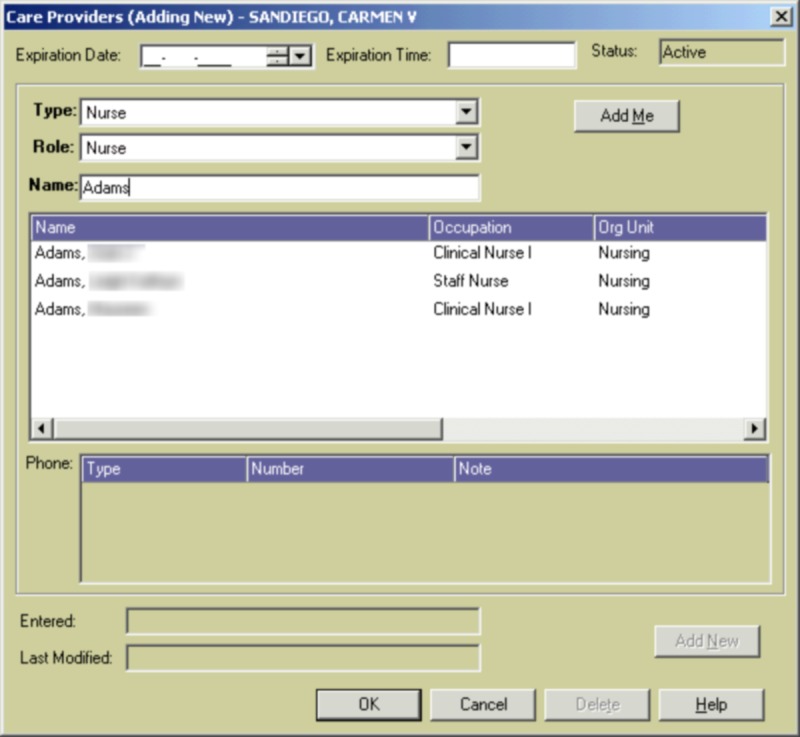
Although the Care Providers module was a standard component of the EHR, anecdotal reports from clinicians indicated that it was seldom used in practice, and in particular, it did not contain accurate information on the attending physician of record. To address the attending of record problem, the institution in 2009 developed a Designate Provider order, which included a mandatory discrete field (i.e., a drop-down list) for the patient’s attending physician. The order also included optional free-text fields to identify the resident physician, intern, nurse practitioner/physician assistant, and the team name (►Figure 2). The benefits of the Designate Provider order were:
Fig. 2.
Custom “Designate Provider” order entry form.
-
1.
as part of the computerized order entry process, it was more familiar to clinicians than the Care Providers module, and
-
2.
when the order was submitted, the updated attending of record information was synchronized with the institution’s registration system as well as the Care Providers module.
The Designate Provider order was included in the hospital’s standard admission order set, and clinicians were instructed to edit the order whenever a change was made to the attending physician of record. The order could also be edited to reflect changes to the other clinician roles, although because these were captured as free-text, they did not propagate to the Care Providers module. Unlike the Care Providers module, the Designate Provider order could only be updated by clinicians with ordering privileges in the EHR.
3. Results
There were 121 patients admitted to the cardiology wards between March 28, 2010 and April 25, 2010 who had a length of stay from 3–5 days. ►Table 1 shows 6 hours of EHR audit log data for one patient. During this interval, 10 individuals accessed the patient’s chart. Each chart access lasted from less than one minute to over 17 minutes. Activities performed included reviewing laboratory test results, reviewing and entering electronic orders, reading and authoring clinical notes, and documenting vital signs, fluid intakes/outputs, and medications administered. The chart access data shown in ►Table 1 were fairly typical of all patients observed in the study. In general, the highest volume of EHR use occurred from mid-morning to early afternoon. As shown in ►Table 2, the total time that resident physicians and nurses spent accessing a single patient’s chart varied considerably with 16.5–145.8 minutes for residents and 2.7–129.7 minutes for nurses.
Table 1.
Example audit log record showing chronological accesses to one patient’s electronic chart during a six-hour interval (11 am –5 pm).
| Time | Provider Type | Identifier | Minutes spent accessing chart |
|---|---|---|---|
| 11:09:40 | Resident | R1 | 17.3 |
| 11:35:31 | Nurse | N1 | 16.4 |
| 11:41:07 | PA | PA1 | 15.4 |
| 11:44:23 | Resident | R2 | 2.7 |
| 11:56:33 | PA | PA1 | 3.6 |
| 12:11:50 | Nurse | N1 | 5.3 |
| 12:26:36 | Dietitian | D1 | 0.7 |
| 12:29:22 | Resident | R2 | 0.7 |
| 12:30:25 | Nurse | N1 | 9.5 |
| 14:19:22 | PA | PA1 | 6.1 |
| 15:38:19 | Social Worker | SW1 | 5.8 |
| 16:06:21 | Nurse | N2 | 0.6 |
| 16:42:55 | Resident | R3 | 14.6 |
| 16:52:11 | Social Worker | SW2 | 0.5 |
Table 2.
Total duration of interaction with EHR for nurses and resident physicians for one patient.
| Nurse Identifier | Minutes spent accessing chart | Resident Identifier | Minutes spent accessing chart |
|---|---|---|---|
| N1 | 6.7 | R1 | 86.2 |
| N2 | 27.1 | R2 | 28.2 |
| N3 | 2.7 | R3 | 16.5 |
| N4 | 3.5 | R4 | 51.3 |
| N5 | 64.0 | R5 | 21.2 |
| N6 | 129.7 | R6 | 17.4 |
| N7 | 23.7 | R7 | 23.5 |
| N8 | 20.8 | R8 | 145.8 |
| N9 | 15.4 |
►Table 3 summarizes the audit log records for the study patients and compares the number of individuals accessing the patients' charts to the number of individuals specified as part of the care team using the Care Providers module and the Designate Provider order. On average, 30.8 individuals accessed each patient’s chart according to the audit logs, including 1.4 attending physicians, 10.2 nurses, 2.3 residents and 5.4 physician assistants.
Table 3.
Care providers identified for 121 cardiology patients with hospital stay from 3–5 days.
| Audit Log | EHR “Care Providers” Module | Custom “Designate Provider” Order | ||||
|---|---|---|---|---|---|---|
| Patients with ≥1 | Mean # per patient (range) | Patients with ≥1 | Mean # per patient (range) | Patients with ≥1 | Mean # per patient (range) | |
| Attending Physician | 99 | 1.4 (0–5) | 121 | 1.8 (1–5) | 121 | 1.1 (1–2) |
| Resident | 71 | 2.3 (0–14) | 78** | 0.8 (0–2) | ||
| PA | 112 | 5.4 (0–12) | 25 | 0.2 (0–3) | ||
| NP | 21 | 0.5 (0–5) | *** | *** | ||
| Nurse | 121 | 10.2 (4–22) | 100* | 0.9 (0–2) | Not included in Designate Provider Order | |
| Social Worker | 117 | 2.1 (0–4) | ||||
| Dietitian | 103 | 2.1 (0–7) | ||||
| Pharmacist | 66 | 0.8 (0–5) | ||||
| PT/OT | 17 | 0.2 (0–4) | ||||
| Respiratory Therapist | 10 | 0.1 (0–5) | ||||
| Medical Student | 10 | 0.1 (0–1) | ||||
| Other**** | 121 | 5.7 (1–14) | ||||
| TOTAL | 30.8 | 2.7 | 2.1 | |||
* 98/100 nurses specified using the “Care Providers” function were labeled as “Primary Nurse”.
** The “Designate Provider” order had two fields for resident physicians: intern and resident.
*** Physician Assistant/Nurse Practitioner were combined for the “Designate Provider” order.
**** The category “Other” includes unit clerks, technicians, and other support staff.
Overall, the Care Providers module and the Designate Provider order identified fewer individuals per patient than the audit log record (2.7 and 2.2 versus 30.8, respectively). Attending physician and nurse were the only clinician roles recorded for the study patients using the Care Providers module although other clinical roles identified in the audit logs, such as social worker, dietitian, pharmacist, physical/occupational therapist, and medical student, were available for selection. The Designate Provider order was used to specify at least one resident for 64% (78/121) of patients, and at least one physician assistant or nurse practitioner for 20% (25/121) of patients; the number of roles available for designation was limited compared to audit logs and the Care Providers module.
The Care Providers module contained only 0.9 nurses per patient compared with 10.2 from the audit logs. Of note, the nurses that were specified using the “Care Providers” function were virtually all designated as the Primary Nurse for the patient. Primary nursing is a method of nursing practice where one nurse is primarily responsible for coordinating all aspects of nursing care for a patient throughout his/her stay [24]. At our institution, the first nurse caring for a patient was assigned to be the Primary Nurse. When that nurse worked subsequent shifts, he or she would typically be assigned once again to that patient.
4. Discussion
Our findings suggest that accurate and comprehensive lists of care team members may not be available in EHRs. The lack of care team information is one limitation preventing the EHR from becoming the “hub of clinical collaboration” as described in the recent report of the U.S. National Research Council [25]. The report states that current EHRs provide little support for collaboration and describes field observations where “collaborative interactions took place via verbal discussion, not directly supported in any way by the computer systems.”
Compared to other settings (e.g., software development offices) where teams rely on information technology to communicate and collaborate, the hospital environment introduces a number of challenges for electronically capturing and representing team activity. Because of service rotations and the shift-based nature of hospital work, there may be little continuity in teams over time [8]. Moreover, the makeup of clinical teams changes frequently in response to the needs of each patient [7] and transfers of location. Our results suggest that patients who experience a 3–5 day hospital stay have upwards of 30 clinicians accessing their records and participating in their care. Given the complexity of the clinical environment, it is difficult to identify who is on a patient’s care team at any given moment.
In the United States, considerable resources are being expended to deploy and achieve “meaningful use” of EHRs. The draft requirements for Stage 2 of meaningful use require EHRs to have a list of care team members available for at least 10% of patients [6]. Details are not yet available regarding what constitutes a “list of care team members” and how frequently the list must be updated. Based upon our results, we believe that maintaining a comprehensive list that is accurate down to the current hospital nursing shift would require major changes in workflow for many organizations, and would likely require major changes to EHR software modules as well. Nevertheless, we argue that without a comprehensive and accurate list of the care team, important benefits of EHRs may not be realized.
4.1. Benefits of Specifying the Care Team in the EHR
Inadequate communication among members of the care team contributes to many hospital errors [26–28]. Good continuity and coordination of care are associated with reduced costs, increased patient satisfaction, and improved patient outcomes [29–33]. If the EHR contains an accurate list of the clinicians who are responsible for a patient's care, it could facilitate verbal communication among members of the team (e.g., a patient’s nurse could quickly identify the covering physician and how to contact him or her). In addition the EHR may be used to support various forms of electronic communication, such as using alphanumeric paging or video-conferencing. For example, we developed a custom alphanumeric paging module within our EHR. Because patients’ care team members are not effectively documented (as demonstrated by the results of our study), users of the paging module must manually locate the name and beeper number of the clinician they wish to contact.
Another benefit of maintaining an accurate list of a patient’s care providers is the ability to provide timely clinical decision support (e.g., critical laboratory test results) to the correct individuals [34]. While some groups have achieved success in determining the correct notification recipient for EHR alerts using custom-developed applications and algorithms [35–37], such functionality is absent in most commercial EHRs. An accurate, up-to-date list of care providers in the EHR will facilitate the delivery of targeted clinical alerts and reminders to the responsible parties, thus improving the signal to noise ratio and increasing the likelihood that the clinician will attend to the message.
In addition to improving communication among care teams and facilitating targeted clinical decision support, an accurate list of a patient’s hospital care providers could be of great benefit to patients themselves. Hospital patients are often unclear about the identities and roles of the individuals taking care of them. O’Leary et al. found that only 32% of hospitalized patients could correctly name even one of their hospital physicians [38]. Evidence suggests that the patient-practitioner relationship has a considerable impact on trust, adherence to treatment regimens, and patient satisfaction [39–44]. The lack of access to information makes patients and their families feel alienated, uncertain, and anxious [45–47]. If EHRs contain accurate care team information, names and photographs of doctors, nurses, and other individuals can be digitally shared with patients, thus improving patient satisfaction and engagement [21–22].
4.2. Limitations
This study was performed at a single academic medical center with data from patients in two cardiology wards. The medical center had used a commercial EHR system since 2004, so the EHR was familiar to most clinicians at the time the study was performed. Thus, the results of this study may not generalize to other locations, care settings, or EHRs.
From our analysis, many more clinicians appeared to be involved in patients’ care than were explicitly recorded using the Care Providers function or the Designate Provider order in our EHR. However, while the EHR audit logs provided helpful clues to determine the makeup of patient care teams, the information gleaned cannot be construed as a gold standard. Some clinicians caring for a patient may not have needed to access the EHR and would therefore not be identified in the audit logs. Conversely, the mere accessing of patient information by a clinician does not imply that he or she is part of the care team. In some cases, clinicians who appeared in the audit logs may have been only peripherally involved in a patient’s care (e.g., a resident physician logged in to the EHR during group rounds). Enhanced logging capabilities and better methods of analyzing audit log data could help to overcome these limitations.
5. Conclusions
Our study suggests that commercial EHRs may not provide adequate tools for specifying and updating the members of patients’ care teams. Lack of information regarding patients’ care providers may hinder collaboration among clinicians and reduce the ability for EHRs to provide targeted clinical decision support. In addition to improving opportunities for clinical communication and collaboration, specifying care team membership in the EHR will be required for healthcare providers in the United States to receive ARRA financial incentives governed by stages 2 and 3 of Meaningful Use. Hospitals and EHR vendors should leverage the opportunities afforded by Meaningful Use to develop and implement tools that support collaborative work performed by clinical teams.
Clinical Relevance Statement
There is an acute need for electronic health records to support collaborative work performed by clinical teams. Our study suggests that commercial EHRs may not provide adequate tools for specifying and updating the members of patients’ care teams. This obstacle limits the ability for EHRs to improve team communication and provide targeted clinical decision support.
Statement on conflicts of interest
There are no conflicts reported by any of the authors.
Human Subjects Protections
The study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects, and was reviewed by Columbia University Institutional Review Board.
Acknowledgements
This work was partially supported by HRSA grant 1 D11 HP07346 (SB), 5K22LM8805 (PDS), and AACN-Philips Medical Systems Outcomes Grant: CONCERN (SC).
References
- 1.Pronovost PJ, Wu AW, Sexton JB. Acute decompensation after removing a central line: practical approaches to increasing safety in the intensive care unit. Ann Intern Med 2004; 140: 1025–1033 [DOI] [PubMed] [Google Scholar]
- 2.McKnight L, Stetson PD, Bakken S, Curran C, Cimino JJ. Perceived information needs and communication difficulties of inpatient physicians and nurses. Proc AMIA Symp 2001: 453–457 [PMC free article] [PubMed] [Google Scholar]
- 3.O'Malley AS, Grossman JM, Cohen GR, Kemper NM, Pham HH. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med 2009; 25(3): 177–185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bardram JE, Bossen C. A web of coordinative artifacts: collaborative work at a hospital ward. In Proceedings of the International ACM SIGGROUP Conference on Supporting Group Work, GROUP '05: 2005; 168–176 [Google Scholar]
- 5.Blumenthal D. Launching HITECH. N Engl J Med 2010; 362(5): 382–385 [DOI] [PubMed] [Google Scholar]
- 6.Health Information Technology Policy Committee Meaningful use workgroup request for comments regarding meaningful use stage 2. Available at: http://healthit.hhs.gov/media/faca/MU_RFC%20_2011–01–12_final.pdf Accessed 19 May2011
- 7.Patel VL, Cytryn KN, Shortliffe EH, Safran C. The collaborative health care team: the role of individual and group expertise. Teach Learn Med 2000; 12(3): 117–132 [DOI] [PubMed] [Google Scholar]
- 8.Tang C, Carpendale S. Supporting nurses’ information flow by integrating paper and digital charting. In: Proceedings of the European Conference on Computer Supported Cooperative Work (ECSCW) 2009, Vienna, Austria, Sept 7–11, 43–62 [Google Scholar]
- 9.Kannry J, Moore C. MediSign: using a web-based signout system to improve provider identification. Proc AMIA Symp 1999: 550–554 [PMC free article] [PubMed] [Google Scholar]
- 10.Wong HJ, Caesar M, Bandali S, Agnew J, Abrams H. Electronic inpatient whiteboards: improving multidisciplinary communication and coordination of care. Int J Med Inform 2009; 78(4): 239–247 [DOI] [PubMed] [Google Scholar]
- 11.Carroll JM, Neale DC, Isenhour PL, Rosson MB, McCrickard DS. Notification and awareness: synchronizing task-oriented collaborative activity. International Journal of Human-Computer Studies 2003; 58: 605–632 [Google Scholar]
- 12.Carroll JM, Rosson MB, Convertino G, Ganoe C.Awareness and teamwork in computer supported collaborations. Interacting with Computers 2006; 18: 21–46 [Google Scholar]
- 13.Viégas FB, Donath JS. Chat circles. In: Proceedings of the ACM SIGCHI Conference on Human Factors in Computing Systems, CHI '99. 1999; 9–16 [Google Scholar]
- 14.Tang J, Yankelovich N, Begole J, Van Kleek M, Li F, Bhalodia J. ConNexus to awarenex: extending awareness to mobile users. In: Proceedings of the ACM 28th International Conference on Human Factors in Computing Systems, CHI '10: 2001; 221–228 [Google Scholar]
- 15.Buxton WAS, Sellen AJ, Sheasby MC. Interfaces for multiparty video conferences. Finn KE, Sellen AJ, Wilbur SB.(Eds.). Video-mediated communication Mahwah, NJ: Lawrence Erlbaum Associates; 1997; 385–400 [Google Scholar]
- 16.McGrath JE. Groups: interaction and performance. Inglewood, NJ: Prentice Hall, Inc; 1984 [Google Scholar]
- 17.Arrow H, McGrath JE, Berdahl JL. Small groups as complex systems: formation, coordination, development, and adaptation. Beverly Hills, CA: Sage Publications; 2000 [Google Scholar]
- 18.Bodker S. Applying activity theory to video analysis: how to make sense of video data in human-computer interaction. Nardi BA.(Ed.), Context and consciousness: activity theory and human-computer interaction. Cambridge, MA: MIT Press, 1996; 147–174 [Google Scholar]
- 19.Bardram J. Designing for the dynamics of cooperative work activities. In:Proceedings of the ACM Conference on Computer Supported Cooperative Work, CSCW ’98: 1998; 89–98 [Google Scholar]
- 20.Hripcsak G, Vawdrey DK, Fred MR, Bostwick SB. Use of electronic clinical documentation: time spent and team interactions. J Am Med Inform Assoc 2011; 18(2): 112–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilcox L, Morris D, Tan D, Gatewood J. Designing patient-centric information displays for hospitals. In CHI ’10: Proceedings of the ACM 28th International Conference on Human Factors in Computing Systems 2010; 2123–2132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vawdrey DK, Wilcox L, Collins SA, Bakken S, Feiner S, Restaino SW. Patient use of a tablet computer to participate in hospital care. Proc AMIA Annu Fall Symp, 2011(to appear) [PMC free article] [PubMed] [Google Scholar]
- 23.Chen ES, Cimino JJ. Patterns of usage for a Web-based clinical information system. Stud Health Technol Inform 2004; 107(Pt1): 18–22 [PubMed] [Google Scholar]
- 24.Bowers L. The significance of primary nursing. J Adv Nurs 1989; 14(1): 13–19 [DOI] [PubMed] [Google Scholar]
- 25.Stead W, Lin H.(eds.) Computational technology for effective health care: immediate steps and strategic directions. Washington, DC: National Academies Press, 2009 [PubMed] [Google Scholar]
- 26.Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med 1991; 324(6): 377–384 [DOI] [PubMed] [Google Scholar]
- 27.Jain M, Miller L, Belt D, King D, Berwick DM. Decline in ICU adverse events, nosocomial infections and cost through a quality improvement initiative focusing on teamwork and culture change. Qual Saf Health Care 2006; 15(4): 235–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coiera E, Tombs V. Communication behaviours in a hospital setting: an observational study. BMJ 1998; 316(7132): 673–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Petersen LA, Brennan TA, O'Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med 1994; 121(11): 866–872 [DOI] [PubMed] [Google Scholar]
- 30.Petersen LA, Orav EJ, Teich JM, O'Neil AC, Brennan TA. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv 1998; 24(2): 77–87 [DOI] [PubMed] [Google Scholar]
- 31.Wasson JH, Sauvigne AE, Mogielnicki RP, Frey WG, Sox CH, Gaudette C, Rockwell A. Continuity of outpatient medical care in elderly men. A randomized trial. JAMA 1984; 252(17): 2413–2417 [PubMed] [Google Scholar]
- 32.Ways M, Umali J, Buchwald D.Frequency and impact of housestaff contact with primary care physicians. J Gen Intern Med 1995; 10(12): 688–690 [DOI] [PubMed] [Google Scholar]
- 33.Neher JO, Kelsberg G, Oliveira D. Improving continuity by increasing clinic frequency in a residency setting. Fam Med 2001; 33(10): 751–755 [PubMed] [Google Scholar]
- 34.Maviglia SM, Yoon CS, Bates DW, Kuperman G. KnowledgeLink: impact of context-sensitive information retrieval on clinicians' information needs. J Am Med Inform Assoc 2006; 13(1): 67–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rind DM, Safran C, Phillips RS, Wang Q, Calkins DR, Delbanco TL, et al. Effect of computer-based alerts on the treatment and outcomes of hospitalized patients. Arch Intern Med 1994; 154(13): 1511–1517 [PubMed] [Google Scholar]
- 36.Hiltz FL, Teich JM. Coverage List: a provider-patient database supporting advanced hospital information services. Proc Annu Symp Comput Appl Med Care 1994: 809–813 [PMC free article] [PubMed] [Google Scholar]
- 37.Kuperman GJ, Teich JM, Bates DW, Hiltz FL, Hurley JM, Lee RY, et al. Detecting alerts, notifying the physician, and offering action items: a comprehensive alerting system. Proc AMIA Annu Fall Symp 1996: 704–708 [PMC free article] [PubMed] [Google Scholar]
- 38.O'Leary KJ, Kulkarni N, Landler MP, Jeon J, Hahn KJ, Englert KM, Williams MV. Hospitalized patients' understanding of their plan of care. Mayo Clin Proc 2010; 85(1): 47–52 Erratum in: Mayo Clin Proc2010; 85(2): 205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clever SL, Jin L, Levinson W, Meltzer DO. Does doctor-patient communication affect patient satisfaction with hospital care? Results of an analysis with a novel instrumental variable. Health Serv Res 2008; 43(5p1): 1505–1519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract 2000; 50(460): 892–899 [PMC free article] [PubMed] [Google Scholar]
- 41.Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol 1999; 17(1): 371–379 [DOI] [PubMed] [Google Scholar]
- 42.Fuertes JN, Mislowack A, Bennett J, Paul L, Gilbert TC, Fontan G, Boylan LS. The physician-patient working alliance. Patient Educ Couns 2007; 66(1): 29–36 [DOI] [PubMed] [Google Scholar]
- 43.Bakken S, Holzemer WL, Brown MA, Powell-Cope GM, Turner JG, Inouye J, Nokes KM, Corless IB. Relationships between perception of engagement with health care provider and demographic characteristics, health status, and adherence to therapeutic regimen in persons with HIV/AIDS. AIDS Patient Care STDS 2000; 14(4): 189–197 [DOI] [PubMed] [Google Scholar]
- 44.Thom DH, Hall MA, Pawlson LG. Measuring patients' trust in physicians when assessing quality of care. Health Aff (Millwood) 2004; 23(4): 124–132 [DOI] [PubMed] [Google Scholar]
- 45.O'Farrell P, Murray J, Hotz SB. Psychologic distress among spouses of patients undergoing cardiac rehabilitation. Heart Lung 2000; 29(2): 97–104 [PubMed] [Google Scholar]
- 46.Burker EJ, Evon D, Loiselle MM, Finkel J, Mill M. Planning helps, behavioral disengagement does not: coping and depression in the spouses of heart transplant candidates. Clin Transplant 2005; 19(5): 653–658 [DOI] [PubMed] [Google Scholar]
- 47.Hannemann-Weber H, Kessel M, Budych K, Schultz C. Shared communication processes within health care teams for rare diseases and their influence on health care professionals' innovative behavior and patient satisfaction. Implement Sci 2011; 6(1): 40. [DOI] [PMC free article] [PubMed] [Google Scholar]