Abstract
Background: Genome-wide association studies (GWAS) have identified consistent associations with obesity. However, the mechanisms remain unclear.
Objective: The objective was to determine the association between obesity susceptibility loci and dietary intake.
Design: The association of GWAS-identified obesity risk alleles (FTO, MC4R, SH2B1, BDNF, INSIG2, TNNI3K, NISCH-STAB1, MTIF3, MAP2K5, QPCTL/GIPR, and PPARG) with dietary intake, measured through food-frequency questionnaires, was investigated in 2075 participants from the Look AHEAD (Action for Health in Diabetes) clinical trial. We adjusted for age, sex, population stratification, and study site.
Results: Obesity risk alleles at FTO rs1421085 significantly predicted more eating episodes per day (P = 0.001)—an effect that persisted after adjustment for body weight (P = 0.004). Risk variants within BDNF were significantly associated with more servings from the dairy product and the meat, eggs, nuts, and beans food groups (P ≤ 0.004). The risk allele at SH2B1 rs4788099 was significantly associated with more servings of dairy products (P = 0.001), whereas the risk allele at TNNI3K rs1514176 was significantly associated with a lower percentage of energy from protein (P = 0.002).
Conclusion: These findings suggest that obesity risk loci may affect the pattern and content of food consumption among overweight or obese individuals with type 2 diabetes. The Look AHEAD Genetic Ancillary Study was registered at clinicaltrials.gov as NCT01270763 and the Look AHEAD study as NCT00017953.
INTRODUCTION
Obesity is a major public health problem associated with an increased risk of cardiovascular disease (1). Obesity susceptibility loci identified through genome-wide association studies (GWAS)4 and replicated in multiple independent cohorts have provided new insights into the genetic factors that contribute to the development of obesity. The fat mass and obesity-associated gene FTO was one of the first genes to be identified by this approach and has been associated with obesity and body mass in numerous cohorts (2–7). Additional genes associated with obesity include MC4R (3), SH2B1, BDNF (7, 8), and, although less consistently replicated, INSIG2 (9). More recent GWAS studies also implicate TNNI3K, NISCH-STAB1, MTIF3, MAP2K5, and QPCTL/GIPR (6). INSIG2 and the Pro12Ala polymorphism in PPARG have also been associated with the degree of weight loss in response to behavioral interventions (10–12).
Many of these genes are expressed in the brain, particularly in the feeding centers of the hypothalamus, emphasizing the role of the central nervous system and potentially dietary intake in obesity predisposition (8). Studies in children indicated that the obesity risk allele at rs9939609 in the FTO gene is associated with preference for energy-dense food (13), greater consumption of fat and calories (14), consumption of palatable food after having eaten a meal (15), and reduced satiety (16), although a lack of association between FTO rs9939609 and caloric intake or the percentage of energy from fat has also been reported (17). In adult populations, MC4R obesity risk alleles were shown to be associated with a greater caloric intake and a greater percentage of energy from fat in one study of women from the Nurses’ Health Study (18) but not in a second sample of men and women of Scottish descent (19). Obesity risk alleles at SH2B1 were associated with greater total fat intake, SFA intake, and MUFA intake in Dutch women (20), but no associations of dietary intake with FTO or MC4R were observed.
The goal of the current study was to determine the association of obesity risk single nucleotide polymorphisms (SNPs) identified through GWAS (within or in the regions of FTO, SH2B1, BDNF, INSIG2, TNNI3K, NISCH-STAB1, MTIF3, MAP2K5, QPCTL/GIPR, MC4R, INSIG2, and PPARG) and available on the ITMAT-Broad-CARe array chip (IBC) (21) or through additional genotyping with measures of dietary intake in the Look AHEAD (Action for Health in Diabetes) cohort—a sample of ethnically diverse overweight and obese participants with type 2 diabetes.
SUBJECTS AND METHODS
Participants
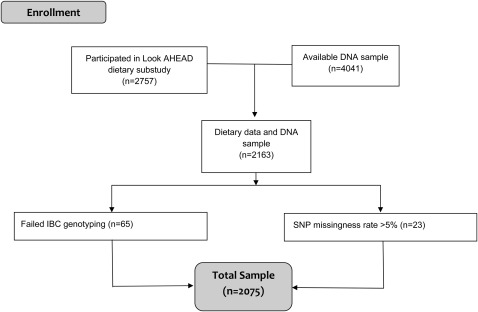
The design and methods of the Look AHEAD trial have been reported elsewhere (22), as have the baseline characteristics of the randomized cohort (23). Of the 5145 ethnically diverse overweight and obese Look AHEAD subjects with type 2 diabetes, aged 45–76 y at baseline, the first 2757 completed the dietary substudy (24); 2163 of the participants in the dietary substudy provided genetic consent and were in clinical centers participating in this ancillary study. Of the 2163, 65 were missing genetic data as a result of failed genotyping, and 23 were missing genetic data as a result of a high degree of missing genotype calls (>5%), yielding an effective sample size of 2075 (Figure 1). Participants who completed the Look AHEAD dietary substudy were somewhat younger than those who did not (57.2 ± 7.2 y compared with 60.5 ± 5.9 y; P < 0.0001) because of a change in the age inclusion criteria during year 2 of the recruitment period. No significant differences in sex, race, or educational attainment were found between the 2 groups. All participants included in this study provided written informed consent for participation in the Look AHEAD trial and genetic analyses in accordance with the requirements of the Institutional Review Board at their local institution. The current data analysis was approved by the Miriam Hospital Institutional Review Board, and the procedures that were followed were in accordance with The Miriam Hospital Guidelines.
FIGURE 1.
Consort flow diagram. IBC, ITMAT-Broad-CARe array chip; Look AHEAD, Look AHEAD (Action for Health in Diabetes) clinical trial; SNP, single nucleotide polymorphism.
Anthropometric measures
Weight and height were measured in duplicate by using a digital scale and a standard wall-mounted stadiometer. BMI was calculated as weight (in kg) divided by height (in m) squared.
Dietary assessment
The Look AHEAD semiquantitative, previously validated food-frequency questionnaire (FFQ) was selected to measure food and nutrient intakes (24–26). The FFQ is a modified version of the Diabetes Prevention Program Food-Frequency questionnaire and was designed to collect information about usual intake of food items during the preceding 6 mo. The Diabetes Prevention Program food list, developed for regional and ethnic sensitivity, was formed the basis of the Look AHEAD FFQ food list. The FFQ contained 134 line items, 20 items that can be used to adjust the 134 main items (ie, type of oil used when cooking, fat added to vegetables), and 3 quality-control questions. Meal-replacement beverages and bars were added as line items to the FFQ.
For each line item, the respondents reported their frequency of consumption and portion size consumed. The 9 frequency categories for food items ranged from “never or less than once per month” to “2 or more times per day.” The 9 frequency categories for beverages ranged from “never or less than once per month” to “6 or more times per day.” Portion sizes were listed as small, medium, or large. The maximum category of frequency of consumption for foods does not apply to meal replacements that could be considered foods (bars) or beverages (liquid meal replacements or reconstituted powders). The maximum category for frequency of consumption of meal replacements (either liquid, bar, or powder) was >4 times/d.
Estimates of The Food Guide Pyramid (27) food group and nutrient intake were conducted by using the Health Habits and History Questionnaire/DietSys software and Look AHEAD–specific programming written to incorporate the Look AHEAD modifications to the questionnaire. The nutrient database was modified from the Diabetes Prevention Program database to incorporate foods added for the Look AHEAD FFQ. These nutrient values were obtained primarily from the Nutrition Data System for Research (version 4.01_30, 1999; Nutrition Coordinating Center). The number of daily eating episodes was defined as the total number of meals and snacks consumed per day as reported on the FFQ.
Genotyping
The genomic DNA extraction is based on the use of the FlexiGene DNA Kit (Qiagen Inc) as described by the manufacturer, and DNA quantitation was performed by using the PicoGreen dsDNA Quantitation Reagent (Invitrogen Inc). Genotyping was carried out at the Children's Hospital of Philadelphia by using the IBC chip, a gene-centric 50,000-SNP array designed to assess potentially relevant loci across a range of cardiovascular, metabolic, and inflammatory syndromes (21). The data set with 14 SNP genotypes at or near 9 reported genes was filtered for individuals with <5% missing genotypes and SNPs with <5% missing data. The mean genotyping success rate for the candidate SNPs was 99.6%. Two additional SNPs in the regions of 2 additional genes were genotyped with Taqman Applied Biosystems Assays-On-Demand by using an Applied Biosystems 7900HT: the MC4R polymorphism rs17782313 (Applied Biosystems catalog number C__32667060_10) and the INSIG2 rs7566605 polymorphism (Applied Biosystems catalog number C__29404113_20).
Gene and SNP selection
We searched the published literature and selected SNPs that had been associated with obesity by GWAS (2–9, 28, 29) or weight loss (10, 12) and appeared on the IBC (21) or, in the case of MC4R and INSIG2, were genotyped by Taqman. The SNP array also included Ancestry Informative SNP Markers and haplotype-tagging SNPs. GWAS obesity SNPs not on the IBC were replaced by proxies when possible by using the SNP Annotation and Proxy Search tool (30) based on haplotype maps of US residents of European ancestry (CEU) and Yoruba people of Ibadan (YRI) as follows: FTO rs9930506 was replaced by rs9922708 [distance 681 base pair (bp) r2 = 1.00, D′ = 1.00 in both CEU and YRI], BDNF rs925946 was replaced by rs1401635 (distance 26,789 bp r2 = 0.96, D′ = 1.00 in CEU; no proxy was available in YRI), SH2B1 rs7498665 was replaced by rs4788099 (distance 27,514 bp r2 = 1.00, D′ = 1.00 in CEU and D′ = 1.00 and r2 = 0.94 in YRI), TNNI3K rs1514175 was replaced by rs1514176 (distance 48 bp r2 = 1.00, D′ = 1.00 in CEU and r2 = 1.00, D′ = 1.00 in YRI), NISCH-STAB1 rs6784615 was replaced by rs4687617 (distance 2851 bp r2 = 1.00, D′ = 1.00 in CEU; no proxy was available in YRI), MTIF3 rs4771122 was replaced by rs7988412 (distance 19898, r2 = 0.83, D′ = 1.00 in CEU; no proxy was available in YRI), MAP2K5 rs2241423 was replaced by rs2241420 (distance 4022 bp, r2 = 0.91, D′ = 1.00 in CEU, r2 = 0.97, D′ = 1.00 in YRI), and QPCTL/GIPR rs2287019 was replaced by rs11672660 (distance 21988 bp, r2 = 0.83, D′ = 1.00 in CEU, r2 = 0.892, D′ = 1.00 in YRI).
Statistical analysis
Observed genotype frequencies were compared with those expected under Hardy-Weinberg equilibrium by using a chi-square test in the 2 most populous racial-ethnic groups (non-Hispanic whites and African Americans). Pearson correlations were used to examine the association between dietary variables, BMI, and weight. Multivariable linear regression analyses were carried out to examine genetic associations with the dietary variables. Additive coding for the number of copies of rare alleles was used, unless the marker minor allele frequency (MAF) fell below 20%, in which case the rare genotype was combined with the intermediate genotype. Therefore, linear regression coefficients capture the effect either of a single copy of the rare allele (MAF ≥0.20) or of being a rare allele carrier (MAF <0.20). In cases in which the risk allele differs from the rare allele, negating the regression coefficients gives the effect of each additional copy of the risk allele (MAF ≥0.20) or of being a risk allele homozygote (MAF <0.20).
All analyses were adjusted for age, sex, study site, and population stratification. For total caloric intake, we further considered whether any observed associations were attributable to weight in secondary models. For eating occasions and the Food Guide Pyramid food groups, we considered whether any observed associations were attributable to total caloric intake by including total caloric intake as a covariate in secondary models. A Huber-White sandwich estimator was used to produce SE robust to deviations from normality (31, 32). Principal component analysis of the genotypic correlation matrix of the 16 markers of interest suggested that the effective number of linearly independent markers in the data set was only 13 (33). Therefore, one can maintain the family-wise error rate at 0.05 via Sidak's adjustment for multiplicity by declaring as statistically significant only those markers with a nominal significance level of 0.05/13 = 0.004 (34). However, because the markers were selected a priori due to their association with obesity, we also consider associations reaching a nominal threshold for statistical significance of 0.05. Analyses were performed by using Splus 8.2 for Solaris/Linux (35). The analyses were performed at Brown University.
To control for admixed study population, all IBC SNPs were examined by principal component analysis using the EIGENSTRAT algorithm (36) as implemented in Golden Helix version 7.1 (Bozeman). Results indicated that most of the variance among the Look AHEAD cohort was accounted for by the first 2 principal components, which agreed with self-reported ethnicity. Accordingly, the first 2 principal components were included as covariates in our analyses to adjust for population stratification in the multi-ethnic Look AHEAD cohort.
RESULTS
Participant characteristics of the subcohort of Look AHEAD used in these analyses are shown in Table 1. Participants came from an ethnically diverse background, and 56% were women. They had an average age of 57.6 y and a BMI in the obese range. Participants reported consuming ∼2000 kcal/d over an average of 4.7 eating episodes. Forty percent of calories were derived from fat, 44% from carbohydrate, and 17% from protein.
TABLE 1.
Baseline characteristics
| Characteristic | Value (n = 2075) |
| Women [n (%)] | 1163 (56.0) |
| Race [n (%)] | |
| African American | 324 (15.6) |
| American Indian/Alaskan Native1 | 12 (0.6) |
| Asian/Pacific Islander | 23 (1.1) |
| White | 1595 (76.9) |
| Other (multiple) | 121 (5.8) |
| Ethnicity [n (%)] | |
| Hispanic/Latino | 161 (8.2) |
| Age (y) | 57.6 ± 7.22 |
| BMI (kg/m2) | 36.3 ± 6.1 |
| Dietary intake | |
| Total energy intake (kcal) | 1992.1 ± 875.7 |
| Eating occasions (no./d) | 4.7 ± 1.2 |
| Carbohydrate (% of energy) | 43.6 ± 7.7 |
| Fat (% of energy) | 40.0 ± 7.0 |
| Protein (% of energy) | 17.2 ± 2.9 |
| Bread, cereal, rice, pasta (servings/d) | 3.2 ± 1.7 |
| Vegetables (servings/d) | 2.9 ± 1.5 |
| Fruit (servings/d) | 1.9 ± 1.4 |
| Milk, yogurt, cheese (servings/d) | 2.2 ± 1.6 |
| Meat, poultry, fish, dry beans, eggs, nuts (servings/d) | 2.7 ± 1.5 |
| Fats, oils, sweets (servings/d) | 2.2 ± 1.8 |
The number of American Indian participants included in this study is less than that in the parent Look AHEAD trial.
Mean ± SD (all such values).
SNP characteristics, including the obesity-risk allele identified in the prior literature, are presented in Table 2. All SNPs under study conformed to Hardy-Weinberg equilibrium, except for rs2241420 in non-Hispanic whites (P < 0.001) and rs1401635 in African Americans (P = 0.02). Given that this sample was selected for being overweight/obese and having type 2 diabetes and that the genetic markers were selected for association with obesity, we retained these markers in analyses.
TABLE 2.
SNP characteristics1
| Chromosome | Closest gene | SNP | Major allele | Minor allele | MAF | Obesity risk allele |
| 1 | TNNI3K | rs1514176 | A | G | 0.48 | G |
| 2 | INSIG2 | rs7566605 | G | C | 0.31 | C |
| 3 | PPARG | rs1801282 | C | G | 0.09 | C2 |
| 3 | NISCH-STAB1 | rs4687617 | A | G | 0.05 | A |
| 11 | BDNF | rs10767664 | A | T | 0.18 | A |
| 11 | BDNF | rs6265 | G | A | 0.16 | G |
| 11 | BDNF | rs1401635 | G | C | 0.29 | C |
| 13 | MTIF3 | rs7988412 | G | A | 0.18 | A |
| 15 | MAP2K5 | rs2241420 | G | A | 0.30 | G |
| 16 | SH2B1 | rs4788099 | A | G | 0.37 | G |
| 16 | FTO | rs1421085 | T | C | 0.40 | C |
| 16 | FTO | rs3751812 | C | A | 0.39 | A |
| 16 | FTO | rs9922708 | G | A | 0.43 | A |
| 16 | FTO | rs9939609 | T | A | 0.45 | A |
| 18 | MC4R | rs17782313 | T | C | 0.25 | C |
| 19 | QPCTL/GIPR | rs11672660 | G | A | 0.19 | G |
MAF, minor allele frequency; SNP, single nucleotide polymorphism.
The C allele at PPARG rs1801282 has been associated with diabetes and resistance to weight loss.
The 4 FTO SNPs were in strong linkage disequilibrium in our white subsample (r2 = 0.80–0.99), but differed in the degree of disequilibrium in our African American subsample (rs3751812 and rs1421085: r2 = 0.96; rs3751812 and rs9922708: r2 = 0.51; rs1421085 and rs9922708: r2 = 0.48; rs9939609 with other SNPs: r2 < 0.13). Two BDNF SNPs, rs6265 and rs10767664, were in strong linkage disequilibrium in both our white (r2 = 0.79) and African American (r2 = 0.69) subsamples. The third BDNF SNP, rs1401635, appeared unrelated to the first two (r2 < 0.11 in both whites and African Americans).
Total caloric intake was positively associated with weight (r = 0.22, P < 0.001), BMI (r = 0.14, P < 0.001), and number of eating episodes (r = 0.17, P < 0.001). Number of eating episodes showed no association with BMI (r = 0.00, P = 0.926) or weight (r = −0.04, P = 0.108).
Total calories
Obesity risk markers within BDNF and FTO were nominally associated with greater total caloric intake (Table 3). Risk alleles at FTO rs1421085, rs3751812, and rs9922708 were associated with 57–60 more calories per day per copy (P = 0.031–0.035). Carriers of the AA genotype at BDNF rs10767664 or the GG genotype at BDNF rs6265 consumed on average >100 kcal/d more than did carriers of the less common genotypes (P = 0.006–0.007). The effect of the 3 FTO SNPs on dietary intake was diminished by statistical adjustment for weight (P = 0.066–0.068). However, BDNF rs10767664 and rs6265 remained nominally associated with total caloric intake after statistical adjustment for weight (rs6265, P = 0.007; rs10767664, P = 0.007).
TABLE 3.
Baseline association of the minor allele at each single nucleotide polymorphism with total caloric intake1
| Adjusted for age, sex, study site, and population stratification |
Adjusted for age, sex, study site, population stratification, and weight |
|||||
| Gene | Single nucleotide polymorphism | Minor allele | β ± SE | P value | β ± SE | P value |
| Total energy intake (kcal) | ||||||
| TNNI3K | rs1514176 | G | 45.193 ± 26.169 | 0.085 | 42.724 ± 25.711 | 0.097 |
| INSIG2 | rs7566605 | C | −20.850 ± 27.815 | 0.453 | −17.082 ± 27.434 | 0.534 |
| PPARG | rs1801282 | G2 | 97.386 ± 52.528 | 0.064 | 94.497 ± 52.129 | 0.070 |
| NISCH-STAB1 | rs4687617 | G | 85.890 ± 61.122 | 0.160 | 78.626 ± 60.108 | 0.191 |
| BDNF | rs10767664 | T2 | −104.005 ± 38.290 | 0.0073 | −103.103 ± 37.993 | 0.0073 |
| BDNF | rs6265 | A2 | −107.090 ± 38.659 | 0.0063 | −103.370 ± 38.332 | 0.0073 |
| BDNF | rs1401635 | C | −25.061 ± 26.324 | 0.341 | −23.982 ± 26.115 | 0.359 |
| MTIF3 | rs7988412 | A | 3.427 ± 40.260 | 0.932 | 0.223 ± 39.938 | 0.995 |
| MAP2K5 | rs2241420 | A | 8.400 ± 28.813 | 0.771 | 14.043 ± 28.402 | 0.621 |
| SH2B1 | rs4788099 | G2 | 33.762 ± 27.025 | 0.211 | 22.708 ± 26.838 | 0.398 |
| FTO | rs1421085 | C | 60.139 ± 27.833 | 0.0313 | 50.581 ± 27.638 | 0.067 |
| FTO | rs3751812 | A | 58.685 ± 27.836 | 0.0353 | 50.746 ± 27.618 | 0.066 |
| FTO | rs9922708 | A | 56.935 ± 26.736 | 0.0333 | 48.480 ± 26.540 | 0.068 |
| FTO | rs9939609 | A | 45.604 ± 27.764 | 0.101 | 38.738 ± 27.434 | 0.158 |
| MC4R | rs17782313 | C | 17.953 ± 30.710 | 0.559 | 12.429 ± 30.497 | 0.684 |
| QPCTL/GIPR | rs11672660 | A2 | 27.161 ± 40.326 | 0.501 | 34.735 ± 39.823 | 0.383 |
All analyses were conducted with multivariable linear regression with the statistical covariates listed in the table (n = 2075). Statistical significance was determined after correction for multiple comparisons, or P ≤ 0.004.
As the marker minor allele frequency fell below 20%, the rare genotype was combined with the intermediate genotype.
P values of nominal significance.
Number of eating episodes
Genetic associations with number of eating episodes are presented in Table 4. Obesity risk alleles at rs1421085 within FTO were significantly associated with eating a greater number of meals and snacks per day (P = 0.001), an effect that persisted after further adjustment for total caloric intake (P = 0.004). Obesity risk alleles at FTO rs3751812, rs9922708, and rs9939609 showed similar effects in the same direction but significance was nominal (P = 0.014–0.039). For QPCTL/GIPR rs11672660, MC4R rs17782313, and PPARG rs1801282, risk alleles associated with obesity or diabetes and resistance to weight loss in the prior literature were nominally associated with fewer eating occasions per day. Statistical adjustment for total caloric intake did not substantially alter these associations.
TABLE 4.
Baseline association of the minor allele at each single nucleotide polymorphism with the number of eating occasions1
| Adjusted for age, sex, study site, and population stratification |
Adjusted for age, sex, study site, population stratification, and total energy intake |
|||||
| Gene | Single nucleotide polymorphism | Minor allele | β ± SE | P value | β ± SE | P value |
| Eating occasions (no./d) | ||||||
| TNNI3K | rs1514176 | G | −0.030 ± 0.037 | 0.414 | −0.041 ± 0.036 | 0.255 |
| INSIG2 | rs7566605 | C | −0.042 ± 0.038 | 0.263 | −0.037 ± 0.037 | 0.317 |
| PPARG | rs1801282 | G2 | 0.153 ± 0.074 | 0.0383 | 0.128 ± 0.073 | 0.080 |
| NISCH-STAB1 | rs4687617 | G | 0.027 ± 0.082 | 0.742 | 0.006 ± 0.081 | 0.945 |
| BDNF | rs10767664 | T2 | −0.024 ± 0.056 | 0.661 | 0.003 ± 0.055 | 0.951 |
| BDNF | rs6265 | A2 | −0.005 ± 0.058 | 0.927 | 0.023 ± 0.057 | 0.682 |
| BDNF | rs1401635 | C | −0.054 ± 0.039 | 0.160 | −0.048 ± 0.038 | 0.205 |
| MTIF3 | rs7988412 | A | 0.028 ± 0.054 | 0.601 | 0.026 ± 0.053 | 0.623 |
| MAP2K5 | rs2241420 | A | −0.023 ± 0.037 | 0.524 | −0.026 ± 0.036 | 0.470 |
| SH2B1 | rs4788099 | G2 | −0.003 ± 0.038 | 0.936 | −0.011 ± 0.037 | 0.758 |
| FTO | rs1421085 | C | 0.125 ± 0.039 | 0.0014 | 0.109 ± 0.038 | 0.0044 |
| FTO | rs3751812 | A | 0.096 ± 0.039 | 0.0143 | 0.081 ± 0.038 | 0.0343 |
| FTO | rs9922708 | A | 0.077 ± 0.037 | 0.0393 | 0.063 ± 0.037 | 0.087 |
| FTO | rs9939609 | A | 0.087 ± 0.037 | 0.0183 | 0.075 ± 0.036 | 0.0373 |
| MC4R | rs17782313 | C | −0.113 ± 0.041 | 0.0063 | −0.112 ± 0.041 | 0.0063 |
| QPCTL/GIPR | rs11672660 | A2 | 0.154 ± 0.054 | 0.0053 | 0.146 ± 0.053 | 0.0063 |
All analyses were conducted with multivariable linear regression with the statistical covariates listed in the table (n = 2075).
Because the marker minor allele frequency fell below 20%, the rare genotype was combined with the intermediate genotype.
P values of nominal significance.
Statistical significance after correction for multiple comparisons, or P ≤ 0.004.
Percentage of energy from fat, carbohydrate, and protein
Genetic associations with percentage of energy from fat, carbohydrate, and protein are presented elsewhere (see Supplemental Table 1 under “Supplemental data” in the online issue). The obesity risk allele at rs1514176 (TNNI3K region) was significantly associated with a lower percentage of energy from protein (P = 0.002; −0.28% per copy). Each copy of the obesity risk allele at FTO rs1421085 was also nominally associated with a greater percentage of energy from fat (P = 0.019; 0.52% per copy). No association with percentage of energy from carbohydrate and no other associations between the obesity risk alleles and percentage of energy from fat or carbohydrate were observed.
Food Guide Pyramid food groups
Several associations of obesity risk alleles with daily servings of breads, cereals, rice and pasta (pyramid food group 1 [PFG1]); dairy products (PFG4); meats, eggs, nuts and beans (PFG5); and fats, oils, and sweets (PFG6) were observed (see Supplemental Table 2 under “Supplemental data” in the online issue). For example, risk variants within BDNF were significantly associated with more servings from the dairy product and the meat, eggs, nuts, and beans food groups (P ≤ 0.004), whereas the risk allele at SH2B1 rs4788099 was also significantly associated with more servings of dairy products (P = 0.001). Statistical adjustment for total caloric intake largely diminished these associations, which suggests that any genetic associations with servings within these food groups were likely mediated via previously noted effects on total caloric intake. In the primary exception, statistical adjustment for total caloric intake did not substantially alter the association of SH2B1 rs4788099 with more servings per day of dairy products (P = 0.002). No associations were observed with servings of vegetables (PFG2) or fruit (PFG3) before or after statistical adjustment for total caloric intake.
DISCUSSION
GWAS have been successful in identifying common genetic variants that are associated with obesity. However, the mechanisms through which these polymorphisms affect obesity remain unclear. Here we report that select obesity genetic risk markers may affect meal patterning and servings per day within specific Food Guide Pyramid food groups, such as dairy products, as measured by an FFQ.
Obesity risk alleles at FTO rs1421085 were significantly associated with a greater number of meals and snacks per day, with nominal associations with greater total caloric intake, greater percentage of energy from fat, and more servings of fats, oils, and sweets. The association of FTO obesity risk SNPs with a greater number of eating occasions was not substantially diminished by adjustment for total caloric intake. The overall picture suggests that variation in FTO may bias meal patterning and perhaps total caloric intake and consumption of sweet or high-fat foods.
Because rs1421085 is in high linkage disequilibrium with rs9939609, our results are largely consistent with prior research in children, which indicates that FTO rs9939609 is associated with a preference for energy-dense food (13), greater consumption of fat and calories (14), consumption of palatable food after having eaten a meal (37), and reduced satiety (15). However, we tested rs9939609 directly in our analyses and found more consistent associations with rs1421085. Previously in adults, no association between FTO rs9939609 and caloric intake or percentage of energy from fat intake has been found (17, 20). Although this suggests that rs1421085 may better capture the effect of this region on dietary intake, the functional significance of this locus in obesity and the role of both rs1421085 and rs9939609 remain to be determined (38, 39).
Risk alleles at BDNF rs6265 and rs10767664 predicted a pattern of dietary variables, including servings of meats, eggs, nuts, and beans and servings of dairy products with nominal associations with total caloric intake; servings of breads, cereals, rice, and pasta; and servings of sweets and fats. BDNF and its primary receptor TrkB are expressed key brain regions of the hypothalamus and dorsal vagal complex related to body weight and energy homeostasis (40–44). Targeted disruption of BDNF in transgenic models results in hyperphagia and obesity (45–49). BDNF rs6265 leads to a valine-to-methionine substitution at position 66 (Val66Met) in the prodomain of the gene. Moreover, at least one case study also links rare mutations in BDNF to severe obesity in an 8-y-old girl (50). The associations with servings within the various food groups were diminished on statistical adjustment for total caloric intake, which suggests that the primary effect was on caloric intake but that the total was achieved through servings with the associated food groups.
The risk allele at rs1514176, an intronic SNP located within TNNI3K, was significantly associated with a lower percentage of energy from protein and nominally associated with more daily servings of fats, oils, and sweets. TNNI3K is a cardiac troponin-interacting kinase expressed primarily in the heart (51). Little is currently known about the mechanisms through which this gene region influences obesity. Because protein is considered to be the most satiating macronutrient (52), diets lower in protein intake may actually contribute to increased overall energy intake as a result of reduced overall feelings of fullness and thereby to a greater degree of positive energy balance.
The risk allele at rs4788099 in the SH2B1 region was significantly associated with more daily servings of dairy products. SH2B1 is involved in leptin signaling. Deletions in this region, including SH2B1, have been associated with early-onset obesity (53). Whereas consumption of more daily servings of dairy products, particularly lower-fat dairy products, has been associated with lower adiposity (54), the food group in this investigation contains both low- and high-fat products. Thus, this relation may be driven by greater intake of high-fat dairy product servings.
It was interesting to note that the number of eating episodes was among the dietary phenotypes most strongly associated with genetic polymorphisms. The relation of number of eating occasions and risk of overweight has been debated. In laboratory studies, it has been shown in some but not all (55, 56) studies that spreading the same total caloric intake over a greater number of meals per day may better control appetite. In free-living populations, it is quite plausible that extra eating occasions could promote greater caloric intake and weight gain; however, the data appear mixed. Certain studies find that a greater number of meals per day is associated with lower body weight (57), whereas others find the opposite effect or no association (58, 59).
The strengths of this study included a large ethnically diverse sample inclusive of men and women, control for population stratifications, use of a well-validated FFQ, and genotyping of many genetic markers previously associated with obesity.
Limitations include basing conclusions on a select cohort of individuals (overweight or obese with type 2 diabetes) and, therefore, conclusions may not be generalizable. Similar to other genetic association studies, the size of the cohort may have prevented us from detecting more modest effects. Although we observed consistent patterns of association, many of the associations were of nominal significance and replication in an independent cohort should be conducted to support or refute these results.
Our study was also cross-sectional in design, which prevented us from determining the time precedence of genetic associations with diet and obesity (eg, whether genetic associations with diet preceded genetic associations with obesity, or vice versa). For example, if diet is a mechanism through which these SNPs increase risk of obesity, it would be expected that associations with diet would precede associations with obesity. It is also possible that people with larger body sizes eat more to maintain their weight, in which case genetic associations with obesity would be expected to precede those with diet. These are important questions for future research with longitudinal modeling.
The measurement of dietary intake also has limitations. Whereas the USDA's 5-pass method, 24-h dietary recall is currently considered to be the gold standard of dietary assessment (60, 61), FFQs are usually used in large samples to assess dietary intake over a specified time period because of their low cost, ease of administration (62), and prior validation against the 24-h dietary recall (26). Because FFQs are conducted by self-report, it is recognized that underreporting of dietary intake is common, particularly in individuals who are overweight (63–66), have diabetes (66), and are wanting to reduce their weight (64). It is plausible that a tendency to underreport dietary intake may have influenced our results. Given the variability of body weight in the sample, it is also possible that systematic underreporting may have occurred, such that greater underreporting occurred among those with the highest BMI. Moreover, physical activity and other factors that determine energy expenditure and thereby energy intake may influence the correlation between weight and caloric intake. Nonetheless, underreporting should have restricted the range of self-reported dietary intake in our sample, rendering the detection of significant associations more difficult. Thus, the identification of genetic associations with dietary intake via FFQs suggests that the strength of these associations may improve with more precise measurement.
In summary, our results suggest that select obesity genetic risk markers—particularly markers within FTO, BDNF, TNNI3K, and SH2B1—predict a pattern of obesogenic dietary intake, including a higher number of eating occasions per day and more servings from calorically dense food groups. If replicated, these results could inform the mechanisms through which these genetic markers are associated with adiposity.
Supplementary Material
Acknowledgments
We acknowledge the Look AHEAD sites that participated in this ancillary study: Johns Hopkins Medical Institutions [Frederick L Brancati (Principal Investigator), Jeff Honas (Program Coordinator), Lawrence J Cheskin (Co-Investigator), Jeanne M Clark (Co-Investigator), Kerry Stewart (Co-Investigator), Richard Rubin (Co-Investigator), Jeanne Charleston, Kathy Horak]; Pennington Biomedical Research Center [George A Bray (Principal Investigator), Kristi Rau (Program Coordinator), Allison Strate (Program Coordinator), Brandi Armand (Program Coordinator), Frank L Greenway (Co-Investigator), Donna H Ryan (Co-Investigator), Donald Williamson (Co-Investigator), Amy Bachand, Michelle Begnaud, Betsy Berhard, Elizabeth Caderette, Barbara Cerniauskas, David Creel, Diane Crow, Helen Guay, Nancy Kora, Kelly LaFleur, Kim Landry, Missy Lingle, Jennifer Perault, Mandy Shipp, Marisa Smith, Elizabeth Tucker]; University of Alabama at Birmingham [Cora E Lewis (Principal Investigator), Sheikilya Thomas (Program Coordinator), Monika Safford (Co-Investigator), Vicki DiLillo, Charlotte Bragg, Amy Dobelstein, Stacey Gilbert, Stephen Glasser, Sara Hannum, Anne Hubbell, Jennifer Jones, DeLavallade Lee, Ruth Luketic, Karen Marshall, L Christie Oden, Janet Raines, Cathy Roche, Janet Truman, Nita Webb, Audrey Wrenn]; Harvard Center, Massachusetts General Hospital [David M Nathan (Principal Investigator), Heather Turgeon (Program Coordinator), Kristina Schumann (Program Coordinator), Enrico Cagliero (Co-Investigator), Linda Delahanty (Co-Investigator), Kathryn Hayward (Co-Investigator), Ellen Anderson (Co-Investigator), Laurie Bissett, Richard Ginsburg, Valerie Goldman, Virginia Harlan, Charles McKitrick, Alan McNamara, Theresa Michel, Alexi Poulos, Barbara Steiner, Joclyn Tosch]; Joslin Diabetes Center [Edward S Horton (Principal Investigator), Sharon D Jackson (Program Coordinator), Osama Hamdy (Co-Investigator), A Enrique Caballero (Co-Investigator), Sarah Bain, Elizabeth Bovaird, Ann Goebel-Fabbri, Lori Lambert, Sarah Ledbury, Maureen Malloy, Kerry Ovalle]; Beth Israel Deaconess Medical Center [George Blackburn (Principal Investigator), Christos Mantzoros (Co-Investigator), Kristinia Day, Ann McNamara]; University of Colorado Health Sciences Center [James O Hill (Principal Investigator), Marsha Miller (Program Coordinator), JoAnn Phillipp (Program Coordinator), Robert Schwartz (Co-Investigator), Brent Van Dorsten (Co-Investigator), Judith Regensteiner (Co-Investigator), Salma Benchekroun, Ligia Coelho, Paulette Cohrs, Elizabeth Daeninck, Amy Fields, Susan Green, April Hamilton, Jere Hamilton, Eugene Leshchinskiy, Michael McDermott, Lindsey Munkwitz, Loretta Rome, Kristin Wallace, Terra Worley]; Baylor College of Medicine [John P Foreyt (Principal Investigator), Rebecca S Reeves (Program Coordinator), Henry Pownall (Co-Investigator), Ashok Balasubramanyam (Co-Investigator), Peter Jones (Co-Investigator), Michele Burrington, Chu-Huang Chen, Allyson Clark, Molly Gee, Sharon Griggs, Michelle Hamilton, Veronica Holley, Jayne Joseph, Patricia Pace, Julieta Palencia, Olga Satterwhite, Jennifer Schmidt, Devin Volding, Carolyn White]; University of Tennessee Health Science Center, University of Tennessee East [Karen C Johnson (Principal Investigator), Carolyn Gresham (Program Coordinator), Stephanie Connelly (Co-Investigator), Amy Brewer, Mace Coday, Lisa Jones, Lynne Lichtermann, Shirley Vosburg, J Lee Taylor]; University of Tennessee Downtown [Abbas E Kitabchi (Principal Investigator), Helen Lambeth (Program Coordinator), Debra Clark, Andrea Crisler, Gracie Cunningham, Donna Green, Debra Force, Robert Kores, Renate Rosenthal, Elizabeth Smith, Maria Sun, Judith Soberman (Co-Investigator)]; University of Minnesota [Robert W Jeffery (Principal Investigator), Carolyn Thorson (Program Coordinator), John P Bantle (Co-Investigator), J Bruce Redmon (Co-Investigator), Richard S Crow (Co-Investigator), Scott Crow (Co-Investigator), Susan K Raatz (Co-Investigator), Kerrin Brelje, Carolyne Campbell, Jeanne Carls, Tara Carmean-Mihm, Emily Finch, Anna Fox, Elizabeth Hoelscher, La Donna James, Vicki A Maddy, Therese Ockenden, Birgitta I Rice, Ann D Tucker, Mary Susan Voeller, Cara Walcheck]; St Luke's Roosevelt Hospital Center [Xavier Pi-Sunyer (Principal Investigator), Jennifer Patricio (Program Coordinator), Stanley Heshka (Co-Investigator), Carmen Pal (Co-Investigator), Lynn Allen, Diane Hirsch, Mary Anne Holowaty]; University of Pennsylvania [Thomas A Wadden (Principal Investigator), Barbara J Maschak-Carey (Program Coordinator), Stanley Schwartz (Co-Investigator), Gary D Foster (Co-Investigator), Robert I Berkowitz (Co-Investigator), Henry Glick (Co-Investigator), Shiriki K Kumanyika (Co-Investigator), Johanna Brock, Helen Chomentowski, Vicki Clark, Canice Crerand, Renee Davenport, Andrea Diamond, Anthony Fabricatore, Louise Hesson, Stephanie Krauthamer-Ewing, Robert Kuehnel, Patricia Lipschutz, Monica Mullen, Leslie Womble, Nayyar Iqbal]; University of Pittsburgh [David E Kelley (Principal Investigator), Jacqueline Wesche-Thobaben (Program Coordinator), Lewis Kuller (Co-Investigator), Andrea Kriska (Co-Investigator), Janet Bonk, Rebecca Danchenko, Daniel Edmundowicz (Co-Investigator), Mary L Klem (Co-Investigator), Monica E Yamamoto (Co-Investigator), Barb Elnyczky, George A Grove, Pat Harper, Janet Krulia, Juliet Mancino, Anne Mathews, Tracey Y Murray, Joan R Ritchea, Jennifer Rush, Karen Vujevich, Donna Wolf]; Miriam Hospital/Brown Medical School [Rena R Wing (Principal Investigator), Renee Bright (Program Coordinator), Vincent Pera (Co-Investigator), John Jakicic (Co-Investigator), Deborah Tate (Co-Investigator), Amy Gorin (Co-Investigator), Kara Gallagher (Co-Investigator), Amy Bach, Barbara Bancroft, Anna Bertorelli, Richard Carey, Tatum Charron, Heather Chenot, Kimberley Chula-Maguire, Pamela Coward, Lisa Cronkite, Julie Currin, Maureen Daly, Caitlin Egan, Erica Ferguson, Linda Foss, Jennifer Gauvin, Don Kieffer, Lauren Lessard, Deborah Maier, JP Massaro, Tammy Monk, Rob Nicholson, Erin Patterson, Suzanne Phelan, Hollie Raynor, Douglas Raynor, Natalie Robinson, Deborah Robles, Jane Tavares]; University of Texas Health Science Center at San Antonio [Steven M. Haffner (Principal Investigator), Maria G Montez (Program Coordinator), Carlos Lorenzo (Co-Investigator)]; University of Washington/VA Puget Sound Health Care System [Steven Kahn (Principal Investigator), Brenda Montgomery (Program Coordinator), Robert Knopp (Co-Investigator), Edward Lipkin (Co-Investigator), Matthew L Maciejewski (Co-Investigator), Dace Trence (Co-Investigator), Terry Barrett, Joli Bartell, Diane Greenberg, Anne Murillo, Betty Ann Richmond, April Thomas]; Coordinating Center, Wake Forest University [Mark A Espeland (Principal Investigator), Judy L Bahnson (Program Coordinator), Lynne Wagenknecht (Co-Investigator), David Reboussin (Co-Investigator), W Jack Rejeski (Co-Investigator), Alain Bertoni (Co-Investigator), Wei Lang (Co-Investigator), Gary Miller (Co-Investigator), David Lefkowitz (Co-Investigator), Patrick S Reynolds (Co-Investigator), Paul Ribisl (Co-Investigator), Mara Vitolins (Co-Investigator), Michael Booth (Program Coordinator), Kathy M Dotson (Program Coordinator), Amelia Hodges (Program Coordinator), Carrie C Williams (Program Coordinator), Jerry M Barnes, Patricia A Feeney, Jason Griffin, Lea Harvin, William Herman, Patricia Hogan, Sarah Jaramillo, Mark King, Kathy Lane, Rebecca Neiberg, Andrea Ruggiero, Christian Speas, Michael P Walkup, Karen Wall, Michelle Ward, Delia S West, Terri Windham]; Central Laboratory, Northwest Lipid Research Laboratories [Santica M Marcovina (Principal Investigator), Greg Strylewicz]. All other Look AHEAD staff are listed alphabetically by site. These nongovernmental agencies had no role in the design, implementation, analysis, or interpretation of the data.
The authors’ responsibilities were as follows—JMM, GDP, IP, GSH, and RRW: designed the research; GDP and IP: analyzed the data; JMM, GDP, IP, GSH, HAR, LMD, LJC, AB, LEW, and RRW: wrote the manuscript; and JMM: had primary responsibility for the final content. All authors read and approved the final manuscript. None of the authors had a conflict of interest to declare.
Footnotes
Abbreviations used: bp, base pair; CEU, US residents of European ancestry; FFQ, food-frequency questionnaire; GWAS, genome-wide association study; IBC, ITMAT-Broad-CARe array chip; Look AHEAD, Action for Health in Diabetes; MAF, minor allele frequency; PFG, pyramid food group; SNP, single nucleotide polymorphism; YRI, Yoruba people of Ibadan.
REFERENCES
- 1.Cannon CP. Obesity-related cardiometabolic complications. Clin Cornerstone 2008;9:11–19. [DOI] [PubMed] [Google Scholar]
- 2.Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, Perry JR, Elliott KS, Lango H, Rayner NW, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 2007;316:889–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loos RJ, Lindgren CM, Li S, Wheeler E, Zhao JH, Prokopenko I, Inouye M, Freathy RM, Attwood AP, Beckmann JS, et al. Common variants near MC4R are associated with fat mass, weight and risk of obesity. Nat Genet 2008;40:768–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sabatti C, Service SK, Hartikainen AL, Pouta A, Ripatti S, Brodsky J, Jones CG, Zaitlen NA, Varilo T, Kaakinen M, et al. Genome-wide association analysis of metabolic traits in a birth cohort from a founder population. Nat Genet 2009;41:35–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scuteri A, Sanna S, Chen WM, Uda M, Albai G, Strait J, Najjar S, Nagaraja R, Orru M, Usala G, et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genet 2007;3:e115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Speliotes EK, Willer CJ, Berndt SI, Monda KL, Thorleifsson G, Jackson AU, Allen HL, Lindgren CM, Luan J, Magi R, et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet 2010;42:937–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thorleifsson G, Walters GB, Gudbjartsson DF, Steinthorsdottir V, Sulem P, Helgadottir A, Styrkarsdottir U, Gretarsdottir S, Thorlacius S, Jonsdottir I, et al. Genome-wide association yields new sequence variants at seven loci that associate with measures of obesity. Nat Genet 2009;41:18–24 [DOI] [PubMed] [Google Scholar]
- 8.Willer CJ, Speliotes EK, Loos RJ, Li S, Lindgren CM, Heid IM, Berndt SI, Elliott AL, Jackson AU, Lamina C, et al. Six new loci associated with body mass index highlight a neuronal influence on body weight regulation. Nat Genet 2009;41:25–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herbert A, Gerry NP, McQueen MB, Heid IM, Pfeufer A, Illig T, Wichmann HE, Meitinger T, Hunter D, Hu FB, et al. A common genetic variant is associated with adult and childhood obesity. Science 2006;312:279–83 [DOI] [PubMed] [Google Scholar]
- 10.Franks PW, Jablonski KA, Delahanty L, Hanson RL, Kahn SE, Altshuler D, Knowler WC, Florez JC. The Pro12Ala variant at the peroxisome proliferator-activated receptor gamma gene and change in obesity-related traits in the Diabetes Prevention Program. Diabetologia 2007;50:2451–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Franks PW, Jablonski KA, Delahanty LM, McAteer JB, Kahn SE, Knowler WC, Florez JC. Assessing gene-treatment interactions at the FTO and INSIG2 loci on obesity-related traits in the Diabetes Prevention Program. Diabetologia 2008;51:2214–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindi VI, Uusitupa MI, Lindstrom J, Louheranta A, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, et al. Association of the Pro12Ala polymorphism in the PPAR-gamma2 gene with 3-year incidence of type 2 diabetes and body weight change in the Finnish Diabetes Prevention Study. Diabetes 2002;51:2581–6 [DOI] [PubMed] [Google Scholar]
- 13.Cecil JE, Tavendale R, Watt P, Hetherington MM, Palmer CN. An obesity-associated FTO gene variant and increased energy intake in children. N Engl J Med 2008;359:2558–66 [DOI] [PubMed] [Google Scholar]
- 14.Timpson NJ, Emmett PM, Frayling TM, Rogers I, Hattersley AT, McCarthy MI, Davey Smith G. The fat mass- and obesity-associated locus and dietary intake in children. Am J Clin Nutr 2008;88:971–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wardle J, Cooke L. Genetic and environmental determinants of children's food preferences. Br J Nutr 2008;99(Suppl 1):S15–21 [DOI] [PubMed] [Google Scholar]
- 16.Wardle J, Carnell S, Haworth CM, Farooqi IS, O'Rahilly S, Plomin R. Obesity associated genetic variation in FTO is associated with diminished satiety. J Clin Endocrinol Metab 2008;93:3640–3 [DOI] [PubMed] [Google Scholar]
- 17.Liu G, Zhu H, Lagou V, Gutin B, Stallmann-Jorgensen IS, Treiber FA, Dong Y, Snieder H. FTO variant rs9939609 is associated with body mass index and waist circumference, but not with energy intake or physical activity in European- and African-American youth. BMC Med Genet 2010;11:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qi L, Kraft P, Hunter DJ, Hu FB. The common obesity variant near MC4R gene is associated with higher intakes of total energy and dietary fat, weight change and diabetes risk in women. Hum Mol Genet 2008;17:3502–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tenesa A, Campbell H, Theodoratou E, Dunlop L, Cetnarskyj R, Farrington SM, Dunlop MG. Common genetic variants at the MC4R locus are associated with obesity, but not with dietary energy intake or colorectal cancer in the Scottish population. Int J Obes (Lond) 2009;33:284–8 [DOI] [PubMed] [Google Scholar]
- 20.Bauer F, Elbers CC, Adan RA, Loos RJ, Onland-Moret NC, Grobbee DE, van Vliet-Ostaptchouk JV, Wijmenga C, van der Schouw YT. Obesity genes identified in genome-wide association studies are associated with adiposity measures and potentially with nutrient-specific food preference. Am J Clin Nutr 2009;90:951–9 [DOI] [PubMed] [Google Scholar]
- 21.Keating BJ, Tischfield S, Murray SS, Bhangale T, Price TS, Glessner JT, Galver L, Barrett JC, Grant SF, Farlow DN, et al. Concept, design and implementation of a cardiovascular gene-centric 50 k SNP array for large-scale genomic association studies. PLoS ONE 2008;3:e3583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ryan DH, Espeland MA, Foster GD, Haffner SM, Hubbard VS, Johnson KC, Kahn SE, Knowler WC, Yanovski SZ. Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Control Clin Trials 2003;24:610–28 [DOI] [PubMed] [Google Scholar]
- 23.Bray G, Gregg E, Haffner S, Pi-Sunyer XF. WagenKnecht LE, Walkup M, Wing R. Baseline characteristics of the randomised cohort from the Look AHEAD (Action for Health in Diabetes) study. Diab Vasc Dis Res 2006;3:202–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vitolins MZ, Anderson AM, Delahanty L, Raynor H, Miller GD, Mobley C, Reeves R, Yamamoto M, Champagne C, Wing RR, et al. Action for Health in Diabetes (Look AHEAD) trial: baseline evaluation of selected nutrients and food group intake. J Am Diet Assoc 2009;109:1367–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Block G, Hartman AA. DIETSYS version 3.0 user's guide. Bethesda, MD: National Cancer Institute, 1994 [Google Scholar]
- 26.Mayer-Davis EJ, Vitolins MZ, Carmichael SL, Hemphill S, Tsaroucha G, Rushing J, Levin S. Validity and reproducibility of a food frequency interview in a Multi-Cultural Epidemiology Study. Ann Epidemiol 1999;9:314–24 [DOI] [PubMed] [Google Scholar]
- 27.USDA The Food Guide Pyramid. Washington, DC: US Department of Agriculture Center for Nutrition Policy and Promotion, 2000 [Google Scholar]
- 28.Dina C, Meyre D, Gallina S, Durand E, Korner A, Jacobson P, Carlsson LM, Kiess W, Vatin V, Lecoeur C, et al. Variation in FTO contributes to childhood obesity and severe adult obesity. Nat Genet 2007;39:724–6 [DOI] [PubMed] [Google Scholar]
- 29.Meyre D, Delplanque J, Chevre JC, Lecoeur C, Lobbens S, Gallina S, Durand E, Vatin V, Degraeve F, Proenca C, et al. Genome-wide association study for early-onset and morbid adult obesity identifies three new risk loci in European populations. Nat Genet 2009;41:157–9 [DOI] [PubMed] [Google Scholar]
- 30.Johnson AD, Handsaker RE, Pulit SL, Nizzari MM, O'Donnell CJ, de Bakker PI. SNAP: a web-based tool for identification and annotation of proxy SNPs using HapMap. Bioinformatics 2008;24:2938–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions. In: Le Cam LM, Neyman J, eds. Proceedings of the Fifth Berkley Symposium on Mathematical Statistics and Probability. Berkeley, CA: University of California Press, 1967;I:221–33.
- 32.White H. Estimation, inference and specification analysis. Cambridge, United Kingdom: Cambridge University Press, 1994 [Google Scholar]
- 33.Li J, Ji L. Adjusting multiple testing in multilocus analyses using the eigenvalues of a correlation matrix. Heredity 2005;95:221–7 [DOI] [PubMed] [Google Scholar]
- 34.Sidak Z. Rectangular confidence region for the means of multivariate normal distributions. J Am Stat Assoc 1967;62:626–33 [Google Scholar]
- 35.TIBCO Software I TIBCO Spotfire SPLUS 8.2 for Solaris/Linux user's guide. Palo Alto, CA: TIBCO Software, Inc, 2010 [Google Scholar]
- 36.Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D. Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet 2006;38:904–9 [DOI] [PubMed] [Google Scholar]
- 37.Wardle J, Llewellyn C, Sanderson S, Plomin R. The FTO gene and measured food intake in children. Int J Obes (Lond) 2009;33:42–5 [DOI] [PubMed] [Google Scholar]
- 38.Fawcett KA, Barroso I. The genetics of obesity: FTO leads the way. Trends Genet 2010;26:266–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tung YC, Yeo GS. From GWAS to biology: lessons from FTO. Ann N Y Acad Sci 2011;1220:162–71 [DOI] [PubMed] [Google Scholar]
- 40.Bariohay B, Lebrun B, Moyse E, Jean A. Brain-derived neurotrophic factor plays a role as an anorexigenic factor in the dorsal vagal complex. Endocrinology 2005;146:5612–20 [DOI] [PubMed] [Google Scholar]
- 41.Bariohay B, Roux J, Tardivel C, Trouslard J, Jean A, Lebrun B. Brain-derived neurotrophic factor/tropomyosin-related kinase receptor type B signaling is a downstream effector of the brainstem melanocortin system in food intake control. Endocrinology 2009;150:2646–53 [DOI] [PubMed] [Google Scholar]
- 42.Huang EJ, Reichardt LF. Trk receptors: roles in neuronal signal transduction. Annu Rev Biochem 2003;72:609–42 [DOI] [PubMed] [Google Scholar]
- 43.Lebrun B, Bariohay B, Moyse E, Jean A. Brain-derived neurotrophic factor (BDNF) and food intake regulation: a minireview. Auton Neurosci 2006;126-127:30–8 [DOI] [PubMed] [Google Scholar]
- 44.Conner JM, Lauterborn JC, Yan Q, Gall CM, Varon S. Distribution of brain-derived neurotrophic factor (BDNF) protein and mRNA in the normal adult rat CNS: evidence for anterograde axonal transport. J Neurosci 1997;17:2295–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fox EA, Byerly MS. A mechanism underlying mature-onset obesity: evidence from the hyperphagic phenotype of brain-derived neurotrophic factor mutants. Am J Physiol Regul Integr Comp Physiol 2004;286:R994–1004 [DOI] [PubMed] [Google Scholar]
- 46.Kernie SG, Liebl DJ, Parada LF. BDNF regulates eating behavior and locomotor activity in mice. EMBO J 2000;19:1290–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lyons WE, Mamounas LA, Ricaurte GA, Coppola V, Reid SW, Bora SH, Wihler C, Koliatsos VE, Tessarollo L. Brain-derived neurotrophic factor-deficient mice develop aggressiveness and hyperphagia in conjunction with brain serotonergic abnormalities. Proc Natl Acad Sci USA 1999;96:15239–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Unger TJ, Calderon GA, Bradley LC, Sena-Esteves M, Rios M. Selective deletion of Bdnf in the ventromedial and dorsomedial hypothalamus of adult mice results in hyperphagic behavior and obesity. J Neurosci 2007;27:14265–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xu B, Goulding EH, Zang K, Cepoi D, Cone RD, Jones KR, Tecott LH, Reichardt LF. Brain-derived neurotrophic factor regulates energy balance downstream of melanocortin-4 receptor. Nat Neurosci 2003;6:736–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gray J, Yeo GS, Cox JJ, Morton J, Adlam AL, Keogh JM, Yanovski JA, El Gharbawy A, Han JC, Tung YC, et al. Hyperphagia, severe obesity, impaired cognitive function, and hyperactivity associated with functional loss of one copy of the brain-derived neurotrophic factor (BDNF) gene. Diabetes 2006;55:3366–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lai ZF, Chen YZ, Feng LP, Meng XM, Ding JF, Wang LY, Ye J, Li P, Cheng XS, Kitamoto Y, et al. Overexpression of TNNI3K, a cardiac-specific MAP kinase, promotes P19CL6-derived cardiac myogenesis and prevents myocardial infarction-induced injury. Am J Physiol Heart Circ Physiol 2008;295:H708–16 [DOI] [PubMed] [Google Scholar]
- 52.Paddon-Jones D, Westman E, Mattes RD, Wolfe RR, Astrup A, Westerterp-Plantenga M. Protein, weight management, and satiety. Am J Clin Nutr 2008;87(suppl):1558S–61S [DOI] [PubMed] [Google Scholar]
- 53.Bachmann-Gagescu R, Mefford HC, Cowan C, Glew GM, Hing AV, Wallace S, Bader PI, Hamati A, Reitnauer PJ, Smith R, et al. Recurrent 200-kb deletions of 16p11.2 that include the SH2B1 gene are associated with developmental delay and obesity. Genet Med 2010;12:641–7 [DOI] [PubMed] [Google Scholar]
- 54.Louie JC, Flood VM, Hector DJ, Rangan AM, Gill TP. Dairy consumption and overweight and obesity: a systematic review of prospective cohort studies. Obes Rev 2011;12:e582–92 [DOI] [PubMed] [Google Scholar]
- 55.Leidy HJ, Armstrong CL, Tang M, Mattes RD, Campbell WW. The influence of higher protein intake and greater eating frequency on appetite control in overweight and obese men. Obesity (Silver Spring) 2010;18:1725–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lemmens SG, Martens EA, Born JM, Martens MJ, Westerterp-Plantenga MS. Staggered meal consumption facilitates appetite control without affecting postprandial energy intake. J Nutr 2011;141:482–8 [DOI] [PubMed] [Google Scholar]
- 57.Holmbäck I, Ericson U, Gullberg B, Wirfalt E. A high eating frequency is associated with an overall healthy lifestyle in middle-aged men and women and reduced likelihood of general and central obesity in men. Br J Nutr 2010;104:1065–73 [DOI] [PubMed] [Google Scholar]
- 58.Mills JP, Perry CD, Reicks M. Eating frequency is associated with energy intake but not obesity in midlife women. Obesity (Silver Spring) 2011;19:552–9 [DOI] [PubMed] [Google Scholar]
- 59.Howarth NC, Huang TT, Roberts SB, Lin BH, McCrory MA. Eating patterns and dietary composition in relation to BMI in younger and older adults. Int J Obes (Lond) 2007;31:675–84 [DOI] [PubMed] [Google Scholar]
- 60.Subar AF, Kipnis V, Troiano RP, Midthune D, Scoeller DA, Bingham S, Sharbaugh CO, Trabulsi J, Runswick S, Ballard-Barbash R, et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. Am J Epidemiol 2003;158:1–13 [DOI] [PubMed] [Google Scholar]
- 61.Shai I, Rosner BA, Shahar DR, Vardi H, Azrad AB, Kanfi A, Schwarzfuchs D, Fraser D. Dietary evaluation and attenuation of relative risk: multiple comparisons between blood and urinary biomarkers, food frequency, and 24-hour recall questionnaires: the DEARR Study. J Nutr 2005;135:573–9 [DOI] [PubMed] [Google Scholar]
- 62.Tooze JA, Subar AF, Thompson FE, Troiano R, Schatzkin A, Kipnis V. Psychosocial predictors of energy underreporting in a large doubly labeled water study. Am J Clin Nutr 2004;79:795–804 [DOI] [PubMed] [Google Scholar]
- 63.Bedard D, Shatenstien B, Nadon S. Underreporting of energy intake from a self-administered food-frequency questionnaire completed by adults in Montreal. Public Health Nutr 2004;7:675–81 [DOI] [PubMed] [Google Scholar]
- 64.Johansson L, Solvoll K, Aa Bjorneboe GE, Drevon CA. Under- and overreporting of energy intake related to weight status and lifestyle in a nationwide sample. Am J Clin Nutr 1998;68:266–74 [DOI] [PubMed] [Google Scholar]
- 65.Olafsdottir AS, Thorsdottir I, Gunnarsdottir I, Thorgeirsdottir H, Steingrimsdottir L. Comparison of women's diet assessed by FFQs and 24-hour recalls with and without underreporters: associations and biomarkers. Ann Nutr Metab 2006;50:450–60 [DOI] [PubMed] [Google Scholar]
- 66.Yannakoulia M, Panagiotakos DB, Pitsavos C, Bathrellou E, Chrysohoou C, Skoumas Y, Stefanadis C. Low energy reporting related to lifestyle, clinical, and pychosocial factors in a randomly selected population sample of Greek adults: The ATTICA study. J Am Coll Nutr 2007;26:327–33 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.