Abstract
A 21-year-old female presented with progressive bilateral visual loss for the past 8 years. The patient had no history of systemic disease, surgery or medications. Complete ophthalmologic examination and topography were performed. On ophthalmic examination, uncorrected visual acuity was counting fingers at 2.5 m (20/50 with pinhole) in the right and left eyes. Both corneas appeared hazy on gross examination. On slit-lamp biomicroscopy, focal grayish-white opacities with indistinct borders were noted in the superficial and deep corneal stroma of both eyes. Both corneas were thin and bulging. Corneal topography showed a pattern consistent with keratoconus. The patient underwent penetrating keratoplasty (PKP). Histopathologic studies after PKP confirmed the diagnosis of macular corneal dystrophy and keratoconus in the same eye. The patient was clinically diagnosed as a case of concurrent macular dystrophy and keratoconus, which is a very rare presentation.
Keywords: Case Report, Cornea, Corneal Dystrophy, Keratoconus, Macular Corneal Dystrophy
INTRODUCTION
Keratoconus (KCN) is a progressive, non-inflammatory corneal stromal thinning disorder which leads to corneal ectasia, with irregular myopic astigmatism and visual impairment as early as in the second decade of life. Although the hereditary pattern is unpredictable, positive family history can be detected in 6–8% of patients.1 However, it is most often an isolated sporadic condition, despite multiple single reports of an association with other systemic or ocular disorders.1,2 Although, keratoconus and corneal dystrophies are rare in the general population, there are reported cases of both occurring in the same eye.3
It is important to report the association of other conditions with keratoconus since many of these combinations could be manifestations of a common pathogenetic mechanism or may represent adjacent genetic defects.1,3 In this report, we present a case with concurrent keratoconus and macular corneal dystrophy (MCD).
CASE REPORT
A 21-year-old female presented with progressive bilateral visual loss for the past 8 years. The patient denied any history of systemic disease, surgery, or medications. There was no consanguinity between her parents. There was no history of a similar disease in her family or pedigree. General physical examination was unremarkable. At the first visit, uncorrected visual acuity (UCVA) was counting fingers at 2.5 m (20/50 with pinhole) in the right and left eyes. Best spectacle visual acuity (BSCVA) and manifest refraction was 20/100 with a correction of -2.00 D in the right eye and 20/70 with a correction of -1.00 D in the left eye. Pupillary reactions and ocular motility were normal. The corneas were hazy bilaterally. On slit-lamp biomicroscopy, focal grayish-white opacities with indistinct borders were noted in the superficial and deep corneal stroma bilaterally. There was diffuse haziness which was more pronounced in the peripheral cornea with greater severity in the left eye. Both eyes were thin and bulging. Incomplete Fleischer's rings were visible at the base of the lesions, and vogt striae were not present [Figure 1]. Intraocular pressures were 8 and 10 mmHg in the right and left eyes, respectively. Objective refraction was not possible and a scissors reflex was present on retinoscopy bilaterally. Despite the hazy media, funduscopy was normal. The patient was clinically diagnosed with macular dystrophy and probable keratoconus (KCN). Corneal topography (EyeSys Vision Inc., Houston, Texas, USA) showed a characteristic pattern of KCN [Figures 2a–d].
Figure 1.
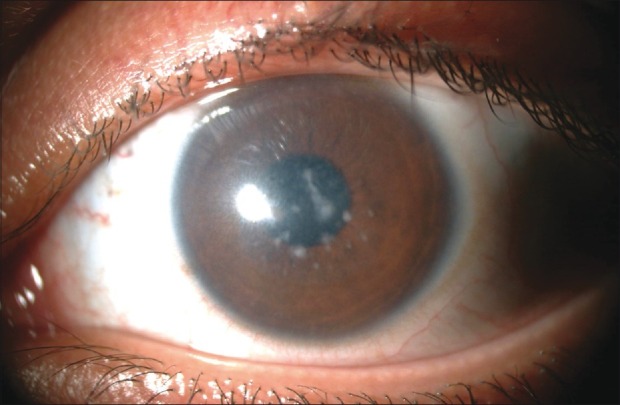
Slit-lamp biomicroscopy showing focal grayish-white opacities with indistinct borders in the superficial and deep corneal stroma. Diffuse haziness especially in the peripheral cornea is notable
Figure 2.
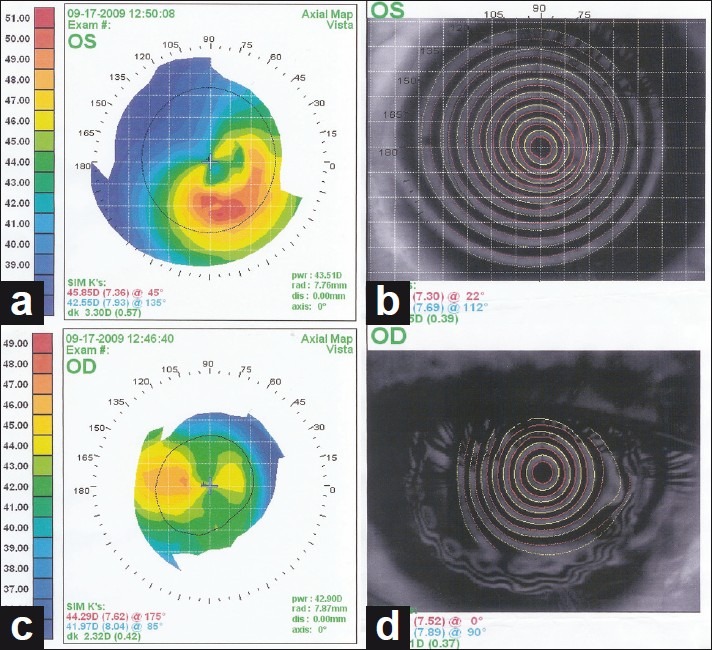
(a-d) Corneal topographies showing inferior steepening consistent with keratoconus in both eyes
Due to the progressive visual loss, the patient underwent penetrating keratoplasty (PKP) in the right eye on January 2009 and three months later in the left eye. The postoperative course was uneventful and there have been no episodes of rejection to date. Histopathologic examination of the corneal buttons indicated a markedly thin cornea with irregular attenuated epithelium and focal Bowman's layer breaks and destruction [Figures 3a and b]. There were diffuse subepithelial and stromal inter-lamellar irregular deposits, which were Periodic Acid-Schiff-reactive [Figure 3c] and intensely blue on alcian blue staining [Figure 3d] which is typical of macular dystrophy. The deposits were also present between endothelial cells that appeared normal. Six months after PKP in the left eye, the UCVA was 20/25 in both eyes. The BCVA with correction of -1.75 -3.00 × 90° was 20/25 in the right eye. Postoperatively the corneas appeared clear bilaterally. To date, there has been no evidence of recurrence of the dystrophy in the grafts.
Figure 3.
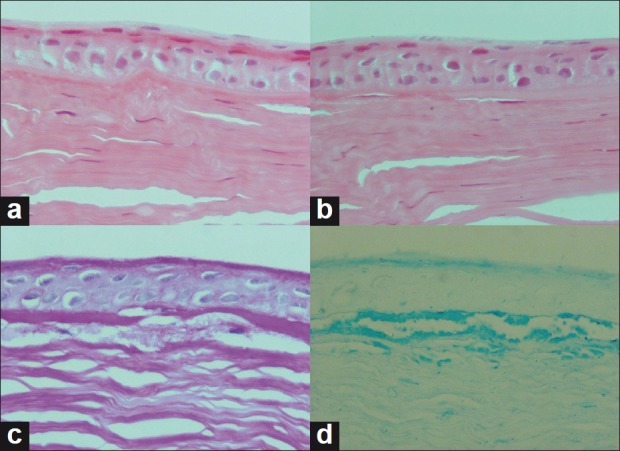
H and E staining of excised corneal buttons showing attenuated and folded Bowman's layer (a) and focal breaks and destruction of Bowman's layer (b), Note the diffuse subepithelial and irregular stromal interlamellar deposits, which are reactive to periodic acid-Schiff (c), Alcian blue staining showing intense blue-colored intrastromal deposits (d)
DISCUSSION
Macular corneal dystrophy is an autosomal recessive disorder characterized by corneal opacities due to intracellular and extracellular deposits within the corneal stroma. Macular dystrophy (MCD) is among the three classic corneal stromal dystrophies but is less common than granular dystrophy or lattice dystrophy. However, there have been reports of higher prevalence of MCD in some regions.4 MCD is characterized by a cloudy, dense stroma with gray-white spots. The macular spots have indistinct edges and the intervening stroma becomes unclear. In MCD the early lesions are central and superficial, with involvement of the peripheral cornea and deep stroma over time. Central corneal thinning confirmed by pachymetry has been previously documented.5 MCD deposits stain easily with alcian blue and colloidal iron and weakly with Periodic Acid-Schiff (PAS). Histochemically, these deposits consist of glycosaminoglycans and resemble keratan sulfate.6
Keratoconus is a non-inflammatory, corneal ectasia. The etiology remains unclear but is likely multifactorial, and the pathogenesis is characterized by an area of protrusion associated with loss of stromal substance. Histopathologic changes include fragmentation of Bowman's layer, stromal and epithelial thinning, folding or rupture of Descemet's membrane and a variable amount of scarring, especially in the anterior stroma; with normal endothelium.3,4
Keratoconus can occur in association with a variety of ocular and systemic diseases. Systemic associations include atopy,2 Down syndrome,7 Ehlers-Danlos syndrome,8 mitral valve prolapse,9 Marfan syndrome,10 osteogenesis imperfecta type I11 and other disorders of connective tissue. Several studies have reported the association of keratoconus with atopic characteristics, vernal conjunctivitis, asthma, hay fever and atopic dermatitis.2 Keratoconus can occur in the presence of isolated ocular pathologies such as retinitis pigmentosa, Leber's congenital amaurosis, vernal keratoconjunctivitis, and corneal dystrophies.3
Associations with corneal dystrophies include granular, posterior polymorphous, fleck, Fuchs and lattice dystrophies.3 The association between macular dystrophy and keratoconus has been described previously in 2 case reports.4,12 The causes of this association remains unknown but may include a poorly understood molecular mechanism, or genetic linkage. Some have postulated abnormal synthetic activity of keratocytes and degeneration of defective basal epithelial cells in both granular corneal dystrophy and keratoconus.13 Javadi et al.,4 noted the interesting biochemical similarities between these two entities such as decreased levels of keratan sulfate and an increased ratio of dermatan to keratan sulfate. They4 hypothesized that a biochemical alteration in collagen fibril size or packing induced by the abnormal deposits in macular dystrophy may predispose to thinning and ectasia. Alternately, this association may be caused by a single genetic alteration. Based on genetic studies, distinct mutations on chromosome 16q22 can cause both types of corneal dystrophies.14 This locus contains a carbohydrate sulfotransferase gene (CHST6) which encodes an enzyme called corneal N-acetylglucosamine 6-sulfotransferase (C-GlcNAc 6ST).15 Based on genetic studies it is apparent that some distinct clinicopathologic corneal dystrophies are caused by different mutations on the same locus.14 Future molecular and genetic studies may elucidate this association.
Using confocal microscopy, Balestrazzi et al.,12 found highly reflective scar tissue that extended from the basal membrane to the underlying stroma. They12 suggested this observation was a focal rupture of Bowman's membrane that is visible in both keratoconus and macular dystrophy. In fact, the main histopathologic alteration of macular dystrophy is represented by focal ruptures of Bowman's membrane that may be irregular, thinned or absent in some areas.12 Macular dystrophy is a stromal dystrophy that is histopathologically characterized by an accumulation of glycosaminoglycans between the stromal lamellae, hence, the deposits may be a large extracellular accumulation of abnormal material.12
The incidence of combined keratoconus and other dystrophies may be higher than suggested by the relative paucity of reports because mild keratoconus can be overlooked on a routine examination. Clinically, these cases demonstrate the importance of excluding corneal dystrophy as a cause of visual complaints in keratoconic patients and excluding keratoconus as an unrecognized cause of visual loss in patients with corneal dystrophies. Corneal topography, confocal microscopy and thorough slit-lamp examination are helpful in determining the coexistence and severity of both disorders. The correct diagnosis of both disorders leads to the most appropriate treatment.3
Although it is not possible to completely rule out a coincidental association between both diseases, considering our observations to earlier case reports strengthens the possibility of an association between these two diseases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Bawazeer AM, Hodge WG, Lorimer B. Atopy and keratoconus: a multivariate analysis. Br J Ophthalmol. 2000;84:834–6. doi: 10.1136/bjo.84.8.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cremona FA, Ghosheh FR, Rapuano CJ, Eagle RC, Jr, Hammersmith KM, Laibson PR, et al. Keratoconus associated with other corneal dystrophies. Cornea. 2009;28:127–35. doi: 10.1097/ICO.0b013e3181859935. [DOI] [PubMed] [Google Scholar]
- 4.Javadi MA, Rafeéi AB, Kamalian N, Karimian F, Jáfarinasab MR, Yazdani S. Concomitant keratoconus and macular corneal dystrophy. Cornea. 2004;23:508–12. doi: 10.1097/01.ico.0000114124.63670.dd. [DOI] [PubMed] [Google Scholar]
- 5.Donnenfeld ED, Cohen EJ, Ingraham HJ, Poleski SA, Goldsmith E, Laibson PR. Corneal thinning in macular corneal dystrophy. Am J Ophthalmol. 1986;101:112–3. doi: 10.1016/0002-9394(86)90473-3. [DOI] [PubMed] [Google Scholar]
- 6.Klintworth GK, Smith CF. Macular corneal dystrophy.Studies of sulfated glycosaminoglycans in corneal explant and confluent stromal cell cultures. Am J Pathol. 1977;89:167–82. [PMC free article] [PubMed] [Google Scholar]
- 7.Stoiber J, Muss W, Ruckhofer J, Grabner G. Acute keratoconus with perforation in a patient with Down's syndrome. Br J Ophthalmol. 2003;87:120. doi: 10.1136/bjo.87.1.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robertson I. Keratoconus and the Ehlers-Danlos syndrome: A new aspect of keratoconus. Med J Aust. 1975;1:571–3. doi: 10.5694/j.1326-5377.1975.tb111590.x. [DOI] [PubMed] [Google Scholar]
- 9.Beardsley TL, Foulks GN. An association of keratoconus and mitral valve prolapse. Ophthalmology. 1982;89:35–7. doi: 10.1016/s0161-6420(82)34857-5. [DOI] [PubMed] [Google Scholar]
- 10.Kenyon KR, Hersh PS, Starck T, Fogle JA. Corneal dysgeneses, dystrophies, and degenerations. In: Tasman WJ, Jaeger EA, editors. Duane's Clinical Ophthalmology. Vol. 4. Philadelphia: Lippincott Williams and Wilkins; 1997. pp. 8–14. Chapter 16. [Google Scholar]
- 11.Nucci P, Brancato R. Keratoconus and congenital hip dysplasia. Am J Ophthalmol. 1991;111:775–6. doi: 10.1016/s0002-9394(14)76792-3. [DOI] [PubMed] [Google Scholar]
- 12.Balestrazzi A, Martone G, Traversi C, Haka G, Toti P, Caporossi A. Keratoconus associated with corneal macular dystrophy: In vivo confocal microscopic evaluation. Eur J Ophthalmol. 2006;16:745–50. doi: 10.1177/112067210601600514. [DOI] [PubMed] [Google Scholar]
- 13.Mitsui M, Sakimoto T, Sawa M, Katami M. Familial case of keratoconus with corneal granular dystrophy. Jpn J Ophthalmol. 1998;42:385–8. doi: 10.1016/s0021-5155(98)00028-8. [DOI] [PubMed] [Google Scholar]
- 14.Klintworth GK. Advances in the molecular genetics of corneal dystrophies. Am J Ophthalmol. 1999;128:747–54. doi: 10.1016/s0002-9394(99)00358-x. [DOI] [PubMed] [Google Scholar]
- 15.Akama TO, Nishida K, Nakayama J, Watanabe H, Ozaki K, Nakamura T, et al. Macular corneal dystrophy type I and type II are caused by distinct mutations in a new sulphotransferase gene. Nat Genet. 2000;26:237–41. doi: 10.1038/79987. [DOI] [PubMed] [Google Scholar]


