Abstract
Background:
The metabolic syndrome is a complex metabolic disturbance due to an interaction between genetic factors, poor dietary habits and physical inactivity.
Aims:
To investigate the role of dietary intake on the prevalence of the metabolic syndrome in a population of elderly, socially active women in Brazil.
Patients and Methods:
A total of 284 women with mean age 69.3 ± 6.3 years were evaluated in a cross-sectional retrospective study. The metabolic syndrome was diagnosed according to criteria of the International Diabetes Federation. The dietary intake was evaluated through a questionnaire for 24-hour dietary recall. The groups with or without the metabolic syndrome were compared for dietary intake and risk factors for metabolic syndrome by the multiple regression model adjusted for age, smoking, physical activity, educational level, total energy intake and fiber contents of the diet. The odds ratio for the presence of the metabolic syndrome was calculated for each nutrient by quartile for total energy intake adjusted by the residue method.
Results:
The prevalence of metabolic syndrome was 32% in the sample. There was not found any association between dietary intake, including all macronutrients and several micronutrients, and the presence of metabolic syndrome.
Conclusion:
No associations were observed between nutritional factors and the prevalence of the metabolic syndrome in elderly women, a result possibly due to the fact that these factors have an influence in earlier phases of life, or to a recent modification of dietary habits, which however was not able to prevent the establishment of the syndrome.
Keywords: Metabolic syndrome, dietary intake, macronutrients, micronutrients, elderly
Introduction
The metabolic syndrome (MS) is a complex metabolic disturbance that includes several risk factors for cardiovascular diseases, such as systemic artery hypertension, atherogenic dyslipidemia, insulin resistance (with or without glucose intolerance) and prothrombotic and proinflammatory tendencies. The syndrome is due to a complex interaction between genetic factors, poor dietary habits and physical inactivity[1,2]. Population studies reported by the National Health and Nutrition Examination Survey (NHANES) have shown that the MS, as defined by the International Diabetes Federation (IDF), has a prevalence of 39% among the US adult population[3]. The estimated prevalence of MS in the Brazilian population is 29.8% (CI95 = 28-32%) and prevalence increased from the youngest (26-34 y) to the oldest (55-64 y) group (15.8% and 48.3%, respectively)[4]. There are scientific evidences showing that some lifestyle behaviors are associated to the risk of having the MS: lack of physical activity, smoking and poor dietary habits, involving particularly excessive intake of carbohydrates and lipids[5]. High carbohydrate ingestion has been correlated with low levels of HDL cholesterol and increased concentration of triglycerides, whereas increased intake of saturated fat associates with hyperinsulinemia[6]. Nevertheless, the precise role of dietary habits in the etiology of the MS is still poorly understood. Investigations have been restricted to a few observational studies in adults, not particularly in the elderly population[7,8]. The present study investigated the influence of nutritional components on the prevalence of MS in a population of elderly women, in the city of Passo Fundo, Brazil.
The aim was to contribute for the establishment of the role of dietary habits in the risk for the metabolic syndrome among the elderly.
Patients and Methods
The population studied was composed of 284 elderly women, aging 60 years or over, socially active and participating of a third age group for recreational activities (Divisão de Apoio ao Idoso) supported by the city hall of Passo Fundo, South Brazil. At the time of this study, there were 1204 participants and the elders were invited to take part of the study.
This study was approved by the Research Ethics Committee of Pontifical Catholic University of Rio Grande do Sul, Brazil, and all participants signed an informed consent form.
Nutritional Evaluation
Dietary habits were recorded through a quantitative questionnaire for 24-hour dietary recall[9]. All questionnaires were recorded by trained dieticians. Besides recording the food ingested during the day, information was collected on the specific characteristics of each meal, such as the way they were prepared and stuffed, use of sugar or sweetener. To reduce the possibility of errors in the research, particularly relating to the representativeness of the dietary habits recorded, soon after the interview the participants were asked if the reported food ingestion represented a usual pattern. In cases in that answers did not match, the participant was asked to provide another dietary recall, so that the usual dietary ingestion could be recorded. Nutritional calculations were performed with the DietWim Professional software version 2.0® (Porto Alegre, RS, Brazil). Nutritional variables selected for this study included total calories, carbohydrates, proteins, lipids, sodium, potassium, magnesium, calcium, zinc and vitamins (A, D, E, C, B6, B9 and B12).
All other information was collected through a structured interview. The educational level was classified in three categories (<1, 1-8 and >8 years of formal study). Physical activity was categorized according to type, duration and periodicity, into four groups (<1x/week, 1-2x/week, 3-4x/week and >4x/week). According to smoking habits, the participants were classified as smokers, ex-smokers (if quitting smoke for more than two years) and non-smokers.
Anthropometrical Data
For measurement of weight (kg) and height (m), performed in an electronic anthropometric scale validated with a fixed stadiometer, individuals were barefoot and wearing light clothes. Waist circumference was measured midway between the iliac crest and the lower rib, with relaxed breathing, at approximately 0.1 cm above the umbilicus. Body mass index (BMI) was determined by weight divided by the square height. Blood pressure was measured with an aneroid sphygmomanometer, validated by an institution affiliated to Inmetro (the Brazilian regulatory agency). The mean of two measurements was used to express the systolic and diastolic blood pressures. Hypertension was defined as systolic pressure ≥ 140 mmHg and/or diastolic pressure ≥ 90 mmHg, or by the use of antihypertensive medications.
Biochemical Analyses
Peripheral blood was collected from the participants after at least a 12-hour fast. Analyses were done through enzymatic colorimetric method with commercial kits for total cholesterol (Cod- Ana Labtest®), HDL cholesterol (precipitating HDL-C, Labtest®), triglycerides (TG) (Gpo-Ana) and glucose (PAP Labtest®). LDL cholesterol was calculated with the Friedewald equation in individual with TG levels < 400 mg/dL, (LDL-C = (TG) - Total cholesterol– HDL-C - TG/5).
Diagnostics of the Metabolic Syndrome
The metabolic syndrome was defined according to criteria proposed by the International Diabetes Federation (IDF)[10], which include altered abdominal circumference and two or more of the following components: plasma lipid levels ≥ 100 mg/dl; systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 85 mmHg (or the use of antihypertensive medication); HDL cholesterol < 50 mg/dL for women; triglycerides ≥ 150 mg/dL. Since the population analyzed had European origin, the cutoff for waist circumference used in this study was ≥ 80 cm.
Statistical Analysis
Quantitative data are presented as mean and standard deviation, and categorical data, as frequency and percentages. The chi-squared test and variance analysis (ANOVA) were used for comparison between the MS and without MS groups. The groups with or without metabolic syndrome were compared for macro- and micronutrients intake, with adjustment of all nutrient values by total energy intake using the residue method. This method also allows the establishment of a regression equation between nutrient intake (as dependent variable) and total caloric intake (as independent variable). The presence of MS considering the quartile of nutrients was evaluated by the multiple logistic regression model with ORs adjusted for age, smoking, physical activity, educational level, total energy intake and fiber contents of the diet. The significance level was α=0.05 for a two-tailed test. Data were analyzed with the SPSS software version 11.5 (SPSS Chicago, IL).
Results
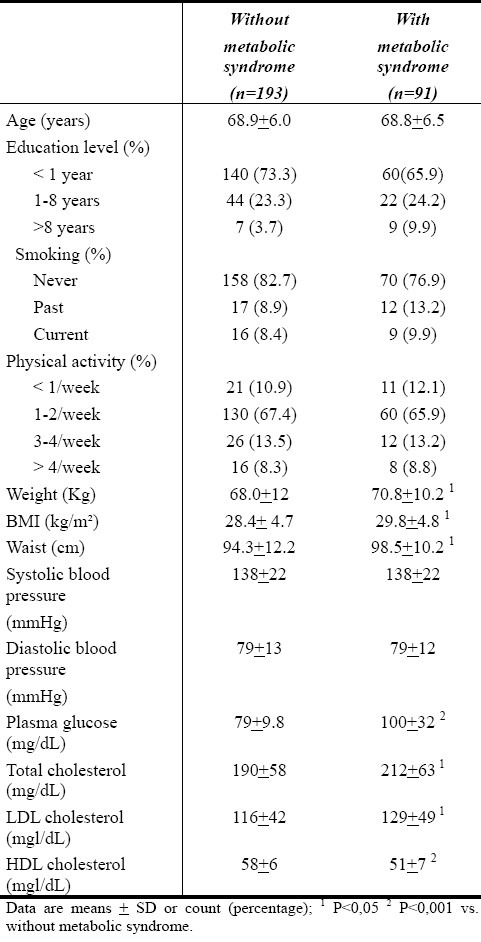
The sample included 284 women. According to the IDF definition[10] 91 (32% of the women) presented MS and 193 (68%) did not. Mean age was 69.3 ± 6.3 years, without differences between the two groups. Women with the MS presented anthropometric measurements such as abdominal circumference and BMI higher than those without the MS (p<0.005 and p<0.04, respectively). Biochemical analyses of total cholesterol, LDL cholesterol, triglycerides, HDL cholesterol and glucose also had less favorable results among women with the MS. No differences were observed for the remaining characteristics. (Table 1).
Table 1.
Characteristics of the study participants
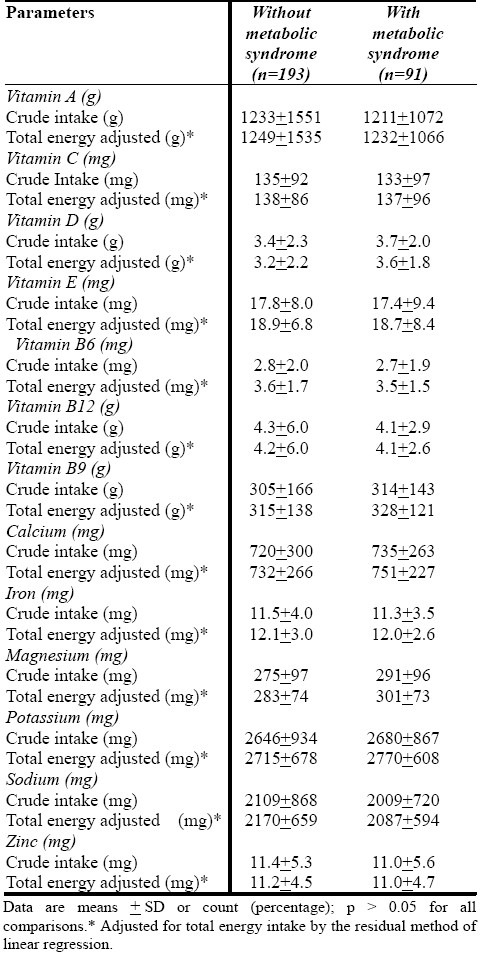
Total energy intake and intake of all macronutrients and several micronutrients, adjusted or not adjusted for total energy intake, were not significantly different among elderly women with or without the metabolic syndrome (Tables 2 and 3).
Table 2.
Daily intake energy and selected nutrients of the study participants
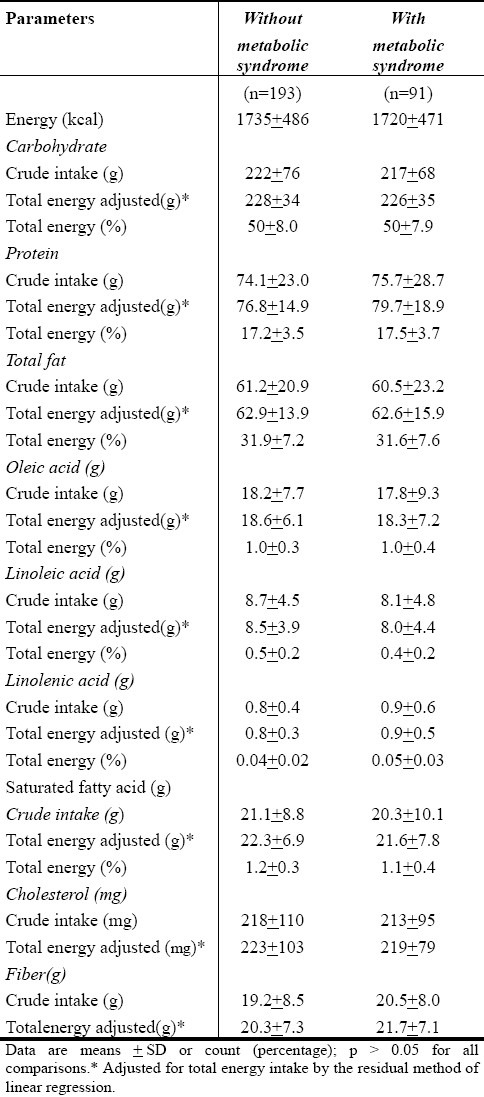
Table 3.
Daily intake energy and selected nutrients of the study participants
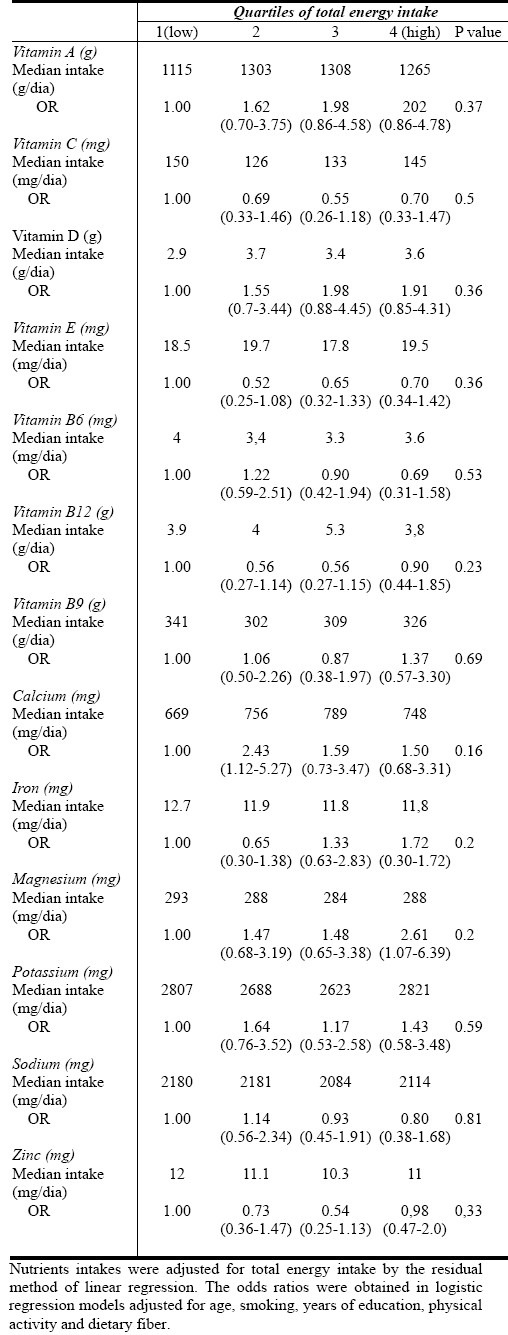
The risk for the metabolic syndrome was not statistically different in relation to quartiles of intake of all macronutrients and several diet micronutrients adjusted for total energy intake, age, smoking, educational level, physical activity and fibers in the diet (Tables 4 and 5).
Table 4.
ORs of metabolic syndrome according to quartiles of total energy intake
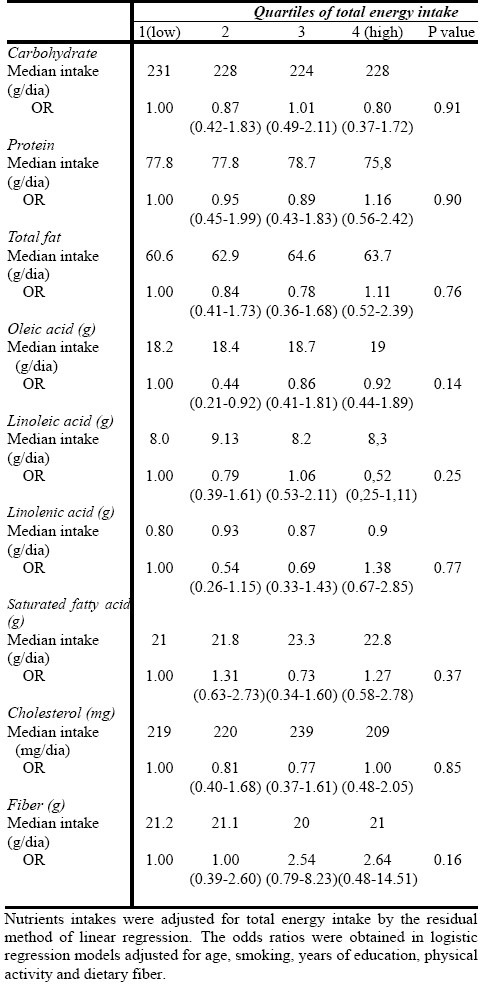
Table 5.
ORs of metabolic syndrome according to quartiles of total energy intake
Discussion
In this study, we evaluated the relationship between dietary components and the metabolic syndrome in the elder women and found no associations between the syndrome and intake of all macronutrients and several micronutrients.
The prevalence of the MS defined according to IDF criteria[10] in the sample of 284 elderly women with mean age of 68.9 years was 32%, similar to results in industrialized countries such as the USA (22.8% to 39.0%)[3,11].
The etiology of the MS is still poorly understood, but it seems to be due to a complex interaction among genetic and environmental factors, which include dietary habits[1,2]. Recent studies have shown that increased total carbohydrate intake may result in altered levels of plasma lipids, lipoprotein concentration and glucose metabolism, leading to the establishment of the MS in some individuals[12]. Although dietary factors are associated to individual components of the MS, such as diabetes mellitus type 2, blood hypertension, dyslipidemia and obesity[13], their role in the etiopathogeny of the combination of these components - the metabolic syndrome - is not well known[14]. Some studies have investigated this question in adult populations, observing some associations between dietary components and the MS[15,16]. No association was observed between total carbohydrate intake and fiber contents of the diet and the MS. Similar results were reported by MC Keown[14], who however observed a relationship between the intake of integral grains and a low prevalence of the MS. Since the present study investigated the association between the MS and nutrients, but not specific types of meals, we could not corroborate those findings.
Interestingly, individuals with or without the metabolic syndrome presented similar intake of carbohydrate, which was higher than the Recommended Dietary Allowances (RDIs)[17], suggesting some type of gene-nutrition interaction. Concerning lipids, some studies have shown an association between the intake of linoleic acid and reduced risk for the MS[18,19]. A similar association was reported by Freire and colleagues[16], who also suggested that total dietary fat may increase the risk for the MS. In humans, a detrimental role for saturated fat and a beneficial effect of polyunsaturated fats are still under debate[20]. The present study did not find any association; both groups presented similar levels of intake of total lipids and linoleic acid, which was in agreement with nutritional recommendations.
In this study, the intake of antioxidant vitamins (A, E, C) by individuals with or without the MS was also investigated. Epidemiological evidences show that antioxidants have a protective role in the physiopathology of several diseases[21]. Ford et al (2003)[22] examined the plasma concentration of antioxidants and their dietary ingestion. The results showed an association between the presence of MS and a low plasma concentration of antioxidants, but not with the intake of vitamins C, E and A. The results of this study corroborate these findings, since no relationship was observed between the MS and ingestion of vitamins C, E and A. The plasma concentration of these vitamins was not analyzed.
Some studies have shown an inverse association between the serum concentration of vitamin D and the prevalence of the metabolic syndrome[23,24]. Low serum concentrations of vitamin D are associated to dysfunction ofpancreas cells and deficient secretion and activity of insulin[24]. In a study with 126 individuals, those with hypovitaminosis D presented a 3-fold higher probability to have MS than individuals with normal concentrations of vitamin D[23]. In another study, by Liu et al (2005)[25], no significant associations were seen between the intake of vitamin D and the prevalence of MS, but a relationship between the ingestion of calcium and milk products and low prevalence of the MS was observed. The present study did not observe associations between the ingestion of calcium and vitamin D and the prevalence of the metabolic syndrome.
Several studies have shown a positive effect of magnesium in several mechanisms involved with the lipidic metabolism, such as glucose intolerance and insulin homeostasis[26,27]. Song et al (2005) showed an inverse association between the intake of magnesium and prevalence of the MS[28]. The results of this study did not show a significant relationship between magnesium ingestion and the MS.
According to most literature reports, the prevalence of MS is not associated with macronutrients and micronutrients present in the diet, but with the type of food ingested[7,8,16,29].
The results of the present study did not disagree with other studies evaluating the relationship between dietary components and the prevalence of the metabolic syndrome among younger adults[7,19,29]. The absence of a relationship between dietary components and the MS in older individuals, shown by these results, may be due to particular characteristics of this age group, which had not been previously investigated. It is possible that the nutritional factors associated to MS have an influence in younger ages (even since intrauterine life, as suggested by some studies), but not in more advanced age as in older individuals. As suggested by Barker et al (1989)[30], environmental factors and particularly nutrition may exert their effects in earlier phases of the development, when they become associated to risks for early onset of cardiovascular disease and metabolic alterations, or premature death (young adults). According to this hypothesis, alterations in nutrition and in the endocrine situation during fetal life result in developmental adaptations which permanently modify structure, physiology and metabolism later in life.
It is also possible that the lack of association between nutritional factors and the MS, observed in the present study, is due to a modification induced in the dietary habits of the participants by previous medical recommendation, motivated by the risk of diseases such as the MS, but which have not been able to prevent the establishment of the syndrome. The method used in this work to analyze dietary habits, the 24-hour dietary recall, may be a limiting factor for not representing the global diet of the participants.
Conclusion
The results of this study suggest that dietary factors do not have an important influence on the risk for the metabolic syndrome in elderly women, and that the condition is due to more a complex interaction of other factors such as lifestyle, genetic susceptibility and metabolism. Multidimensional, longitudinal prospective studies involving groups in different ages, and with the investigation of several aspects such as nutritional habits, lifestyle, genetic factors and metabolism, are necessary for a better understanding of the etiology of the metabolic syndrome.
Acknowledgement
Neide Maria Bruscato participated in the conception and design of the study, performed the acquisition, analysis and interpretation of data and wrote a substantial portion of the manuscript. José Luiz da Costa Vieira performed the analysis and interpretation of data, carried out the statistical analysis, has been involved in revising critically the manuscript and wrote a substantial portion of the manuscript. Nair Mônica Ribascik do Nascimento performed the acquisition of data and has been involved in revising critically the manuscript. Margô Etiene Pazatto Canto performed the acquisition of data and has been involved in revising critically the manuscript. Júlio César Stobbe participated in the conception and design of the study, performed the acquisition of data and has been involved in revising critically the manuscript. Maria Gabriela Gotlieb performed the acquisition of data and has been involved in revising critically the manuscript. Mário Bernardo Wagner performed the analysis and interpretation of data, carried out the statistical analysis and has been involved in revising critically the manuscript. Roberta Rigo Dalacorte performed the analysis and interpretation of data and has been involved in revising critically the manuscript. There was no outside funding/support for this study.
References
- 1.Groop L. Genetics of the metabolic syndrome. Br J Nutr. 2000;83(Suppl 1):S39–48. doi: 10.1017/s0007114500000945. [DOI] [PubMed] [Google Scholar]
- 2.Lidfeldt J, Nyberg P, Nerbrand C, Samsioe G, Schersten B, Agardh CD. Socio-demographic and psychosocial factors are associated with features of the metabolic syndrome.The Women's Health in the Lund Area (WHILA) study. Diabetes Obes Metab. 2003;5(2):106–112. doi: 10.1046/j.1463-1326.2003.00250.x. [DOI] [PubMed] [Google Scholar]
- 3.Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care. 2005;28(11):2745–2749. doi: 10.2337/diacare.28.11.2745. [DOI] [PubMed] [Google Scholar]
- 4.Salaroli LB, Barbosa GC, Mill JG, Molina MC. Prevalence of metabolic syndrome in population-based study, Vitoria, ES-Brazil. Arq Bras Endocrinol Metabol. 2007;51(7):1143–1152. doi: 10.1590/s0004-27302007000700018. [DOI] [PubMed] [Google Scholar]
- 5.Zhu S, St-Onge MP, Heshka S, Heymsfield SB. Lifestyle behaviors associated with lower risk of having the metabolic syndrome. Metabolism. 2004;53(11):1503–1511. doi: 10.1016/j.metabol.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Riccardi G, Giacco R, Rivellese AA. Dietary fat, insulin sensitivity and the metabolic syndrome. Clin Nutr. 2004;23(4):447–456. doi: 10.1016/j.clnu.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Mennen L, Lafay L, Feskens EJM, Novak M, Lépinay P, Balkau B. Possible protective effect of bread and dairy products on the risk of the metabolic syndrome. Nutr Res. 2000;(20):335–347. [Google Scholar]
- 8.Esmaillzadeh A, Mirmiran P, Azizi F. Whole-grain intake and the prevalence of hypertriglyceridemic waist phenotype in Tehranian adults. Am J Clin Nutr. 2005;81(1):55–63. doi: 10.1093/ajcn/81.1.55. [DOI] [PubMed] [Google Scholar]
- 9.Karvetti RL, Knuts LR. Validity of the 24-hour dietary recall. J Am Diet Assoc. 1985;85(11):1437–1442. [PubMed] [Google Scholar]
- 10.Alberti KG, Zimmet P, Shaw J. The metabolic syndrome--a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 11.Adams RJ, Appleton S, Wilson DH, et al. Population comparison of two clinical approaches to the metabolic syndrome: implications of the new International Diabetes Federation consensus definition. Diabetes Care. 2005;28(11):2777–2779. doi: 10.2337/diacare.28.11.2777. [DOI] [PubMed] [Google Scholar]
- 12.Mittendorfer B, Sidossis LS. Mechanism for the increase in plasma triacylglycerol concentrations after consumption of short-term, high-carbohydrate diets. Am J Clin Nutr. 2001;73(5):892–899. doi: 10.1093/ajcn/73.5.892. [DOI] [PubMed] [Google Scholar]
- 13.Montonen J, Knekt P, Jarvinen R, Reunanen A. Dietary antioxidant intake and risk of type 2 diabetes. Diabetes Care. 2004;27(2):362–366. doi: 10.2337/diacare.27.2.362. [DOI] [PubMed] [Google Scholar]
- 14.McKeown NM, Meigs JB, Liu S, Saltzman E, Wilson PW, Jacques PF. Carbohydrate nutrition, insulin resistance, and the prevalence of the metabolic syndrome in the Framingham Offspring Cohort. Diabetes Care. 2004;27(2):538–546. doi: 10.2337/diacare.27.2.538. [DOI] [PubMed] [Google Scholar]
- 15.Yoo S, Nicklas T, Baranowski T, et al. Comparison of dietary intakes associated with metabolic syndrome risk factors in young adults: the Bogalusa Heart Study. Am J Clin Nutr. 2004;80(4):841–848. doi: 10.1093/ajcn/80.4.841. [DOI] [PubMed] [Google Scholar]
- 16.Freire RD, Cardoso MA, Gimeno SG, Ferreira SR. Dietary fat is associated with metabolic syndrome in Japanese Brazilians. Diabetes Care. 2005;28(7):1779–1785. doi: 10.2337/diacare.28.7.1779. [DOI] [PubMed] [Google Scholar]
- 17.Meacham SL, Johnson LJ, Kruskall LJ. Recommended dietary allowances--then and now: a review. J Agromedicine. 2002;8(2):85–93. doi: 10.1300/J096v08n02_11. [DOI] [PubMed] [Google Scholar]
- 18.Laaksonen DE, Lakka TA, Lakka HM, et al. Serum fatty acid composition predicts development of impaired fasting glycaemia and diabetes in middle-aged men. Diabet Med. 2002;19(6):456–464. doi: 10.1046/j.1464-5491.2002.00707.x. [DOI] [PubMed] [Google Scholar]
- 19.Wang L, Folsom AR, Zheng ZJ, Pankow JS, Eckfeldt JH. Plasma fatty acid composition and incidence of diabetes in middle-aged adults: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Clin Nutr. 2003;78(1):91–98. doi: 10.1093/ajcn/78.1.91. [DOI] [PubMed] [Google Scholar]
- 20.Costa MB, Ferreira SR, Franco LJ, Gimeno SG, Iunes M. Dietary patterns in a high-risk population for glucose intolerance.Japanese-Brazilian Diabetes Study Group. J Epidemiol. 2000;10(2):111–117. doi: 10.2188/jea.10.111. [DOI] [PubMed] [Google Scholar]
- 21.Reitman A, Friedrich I, Ben-Amotz A, Levy Y. Low plasma antioxidants and normal plasma B vitamins and homocysteine in patients with severe obesity. Isr Med Assoc J. 2002;4(8):590–593. [PubMed] [Google Scholar]
- 22.Ford ES, Mokdad AH, Giles WH, Brown DW. The metabolic syndrome and antioxidant concentrations: findings from the Third National Health and Nutrition Examination Survey. Diabetes. 2003;52(9):2346–2352. doi: 10.2337/diabetes.52.9.2346. [DOI] [PubMed] [Google Scholar]
- 23.Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr. 2004;79(5):820–825. doi: 10.1093/ajcn/79.5.820. [DOI] [PubMed] [Google Scholar]
- 24.Ford ES, Ajani UA, McGuire LC, Liu S. Concentrations of serum vitamin D and the metabolic syndrome among U.S. adults. Diabetes Care. 2005;28(5):1228–1230. doi: 10.2337/diacare.28.5.1228. [DOI] [PubMed] [Google Scholar]
- 25.Liu S, Song Y, Ford ES, Manson JE, Buring JE, Ridker PM. Dietary calcium, vitamin D, and the prevalence of metabolic syndrome in middle-aged and older U.S. women. Diabetes Care. 2005;28(12):2926–2932. doi: 10.2337/diacare.28.12.2926. [DOI] [PubMed] [Google Scholar]
- 26.Barbagallo M, Dominguez LJ, Galioto A, et al. Role of magnesium in insulin action, diabetes and cardio-metabolic syndrome X. Mol Aspects Med. 2003;24(1-3):39–52. doi: 10.1016/s0098-2997(02)00090-0. [DOI] [PubMed] [Google Scholar]
- 27.Touyz RM. Role of magnesium in the pathogenesis of hypertension. Mol Aspects Med. 2003;24(1-3):107–136. doi: 10.1016/s0098-2997(02)00094-8. [DOI] [PubMed] [Google Scholar]
- 28.Song Y, Ridker PM, Manson JE, Cook NR, Buring JE, Liu S. Magnesium intake, C-reactive protein, and the prevalence of metabolic syndrome in middle-aged and older U.S. women. Diabetes Care. 2005;28(6):1438–1444. doi: 10.2337/diacare.28.6.1438. [DOI] [PubMed] [Google Scholar]
- 29.Pereira MA, Jacobs DR, Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA. 2002;287(16):2081–2089. doi: 10.1001/jama.287.16.2081. [DOI] [PubMed] [Google Scholar]
- 30.Barker DJ, Osmond C, Golding J, Kuh D, Wadsworth ME. Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ. 1989;298(6673):564–567. doi: 10.1136/bmj.298.6673.564. [DOI] [PMC free article] [PubMed] [Google Scholar]


