Abstract
Several domains of parenting have been identified as important for adolescent well-being. Whether these same domains are equally beneficial for adolescents with ADHD histories remains an empirical and clinically important question. This study examined whether parental knowledge of their teen’s activities and whereabouts, consistency, support, and parent-adolescent conflict are associated with substance use and delinquency similarly for adolescents with and without a diagnosis of ADHD in childhood. A sample of 242 adolescents, 142 diagnosed with ADHD in childhood and prospectively followed into adolescence, and 100 without ADHD in childhood, were the focus of study. The relations between adolescent-reported outcomes (i.e. substance use and delinquency) and parenting behaviors were tested using latent variable modeling to determine both the effects of general (common) and specific (unique) parenting behaviors for participants with and without a history of ADHD. Adolescents’ report of parental knowledge was a significant correlate of delinquency and substance use above and beyond other parenting variables and the variance in common across the parenting variables. More knowledge was associated with less delinquency and substance use for all participants, but parental knowledge was more strongly associated with alcohol use for adolescents with versus without childhood ADHD. These correlational findings suggest that, despite the increased difficulty of parenting youths with ADHD histories, actions taken by parents and youth to increase parental awareness may provide some protection against behavioral transgressions known to be elevated in this population.
Attention-deficit/hyperactivity disorder (ADHD) is a behavioral syndrome that first appears in childhood and includes symptoms of inattention, impulsivity, hyperactivity, and associated impairments in multiple domains of functioning (American Psychiatric Association, 2000; Barkley, 2003). Rapidly accumulating research has shown that childhood symptoms of ADHD produce academic and social impairments not only in childhood, but also in adolescence (Barkley, 1998; Barkley et al., 2008; Mannuzza & Klein, 1999). For example, children diagnosed with ADHD are at increased risk of engaging in delinquency and substance use as adolescents (Barkley et al., 1990; Biederman et al., 1996; Gittelman et al., 1985; Katusic et al., 2005; Mannuzza et al., 1991; Molina et al., 2007; Molina & Pelham, 2003; Satterfield et al., 1982; Sibley et al., in press). However, very little research has been conducted to understand the factors that might mitigate this ADHD-related risk. In the current study, the role of parenting behaviors is considered.
Functional impairments and behavior problems associated with ADHD, such as low school grades and defiance of authority, are affected by situational and contextual factors in childhood, including the behavior management skills of adults in the child’s environment (Barkley, 2003; Pelham & Fabiano, 2008). In general, behavioral parent training (BPT) is effective at improving the child management skills of parents and the behavior of children with ADHD (Chronis et al., 2004; Pelham et al., 1998). Yet, only a few studies of BPT training have been conducted for parents of adolescents with ADHD, and they reported small effects of treatment on adolescent behavior (Barkley et al., 1992; Barkley et al., 2001). At the same time, no studies have examined whether naturally occurring parenting practices associated with positive adolescent adjustment are associated with better outcomes for adolescents with childhood ADHD. Efficacious parenting in the natural environment may result in beneficial outcomes that are difficult to produce in a treatment-seeking population characterized by significant dysfunction.
Jessor and Jessor’s (1977) problem behavior theory posits links between positive parenting behaviors and low levels of deviant behavior, including substance use. The relation between positive parenting and deviant behavior has been empirically supported in many studies of adolescent delinquency and substance use among normative samples of adolescents. Research has demonstrated that certain types of positive parenting practices, such as nurturance, support, consistent and balanced discipline, and use of an authoritative parenting style, are associated with less involvement in substance use and delinquency in these samples (Bahr & Hoffmann, 2010; Bailey et al., 2009; Mrug et al., 2010; Windle et al., 2010). Although researchers have studied a variety of parenting behaviors in normative community samples, as well as in high risk samples not selected for ADHD, parental monitoring has received the most attention in studies of adolescent delinquency and substance use. However, its relevance to the management of ADHD-related risk is still unknown.
Parental monitoring is often defined as parenting behaviors used to learn about an adolescent’s friends, whereabouts, and activities (Barnes et al., 2006; Stattin & Kerr, 2000). Parents use monitoring strategies, such as verifying a teen’s location and communicating frequently about activities, to enforce rules, to make decisions about management strategies with their teen, and to react promptly when rules are broken. Dishion and colleagues (1988) initially reported that parental monitoring was negatively associated with adolescent participation in deviant behaviors. Subsequently, numerous studies have shown that higher parental monitoring is associated with lower levels of delinquent behavior and substance use in normative samples of adolescents (Dishion & McMahon, 1998; Granic et al., 2003; Nash et al., 2005; Patterson et al., 1989; Waizenhofer et al., 2004). Stattin and Kerr (2000) suggested that parents’ knowledge of their teenager’s activities and whereabouts may depend not only on parents’ active monitoring efforts but also on the adolescent’s willingness to share information with their parents. Thus, adolescent report of parental knowledge has become a key variable in studies of parental monitoring success. Indeed, research has shown strong negative correlations between adolescent-reported parental awareness and delinquency (Lamborn et al., 1991; Steinberg et al., 1994). However, whether this association applies equally to youth with and without ADHD histories is unknown. Moreover, individual characteristics common or suspected among adolescents with ADHD histories (e.g., aggression; stress reaction; poor control of behavior) have been found to be inversely associated with parental monitoring efforts (Eaton et al., 2009; Stattin & Kerr, 2000). Thus, the persistent behavior problems of many adolescents with childhood ADHD might discourage parental efforts to monitor and be knowledgeable. If so, both the levels and the benefits of monitoring and awareness may be compromised for adolescents with ADHD histories.
Other facets of parenting have been identified as important influences on adolescent delinquency and substance use. Consistency in the enforcement of rules and applications of punishments and rewards is one such facet. Previous research has found that consistent application of rules and punishments is related to lower levels of adolescent substance use in community samples (Engels & van der Vorst, 2003; Jackson et al., 1999; van der Vorst et al., 2006; van der Vorst et al., 2009; van der Zwaluw et al., 2008). Prospective longitudinal studies of children’s problem behavior and parenting have shown negative associations between consistent discipline and delinquency and substance use in adolescence (Stice & Barrera, 1995; Stice et al., 1993). Similar associations have been documented for children of elementary school-age, with inconsistency in parenting during childhood associated with greater noncompliance and behavior problems (Danforth et al., 1991; Patterson, 1986; Stormshak et al., 2000; Wahler & Dumas, 1986). Although poor parenting is not believed to be the cause of ADHD (Barkley, 1998), parents of children with ADHD are more likely to utilize negative/ineffective discipline than parents whose children do not have ADHD (Hinshaw et al., 2000; Wells et al., 2000). However, it is unknown whether inconsistent discipline is more common among parents of adolescents with ADHD histories. There is recent promising evidence that behavior therapy for childhood ADHD, which included parent training, leads to lower rates of experimentation with substances in early adolescence (Molina et al., 2007). These findings suggest that parental discipline consistency in adolescence may also have important implications for the management of delinquency and substance use for adolescents with ADHD histories. This possibility has yet to be tested.
Finally, in addition to parental monitoring and parenting consistency, the emotional quality of the parent-adolescent relationship has often been invoked as important in facilitating healthy adjustment in youth (Conger & Ge, 1999). The extent to which adolescents feel that their parents are available for emotional support and assistance with problem-solving is typically considered as a distinct yet important component of the parent-adolescent relationship (Ackard et al., 2006; Letourneau et al., 2001). Studies have shown that adolescent-perceived parental support is associated with lower levels of adolescent substance use and delinquency, even when parental monitoring and use of rules and discipline were controlled (Chassin et al., 2005; Fleming et al., 2002; Hill et al., 2005; Tilson et al., 2004). A component of parent-child relationship quality is the extent to which conflict is experienced (Laursen et al., 1998; Steinberg, 1990). Disagreements and frustration become more magnified in adolescence, even in the context of a supportive relationship (De Goede et al., 2009; Feinberg et al., 2003). Greater levels of parent-teen conflict are frequently associated cross-sectionally and prospectively with delinquency and substance use (Gorman-Smith et al., 1998; McQueen et al., 2003; Steinberg, 2001). Some research has been conducted on the parent-teen relationship in the presence of adolescent ADHD but few studies have tested whether the quality of the relationship matters, above and beyond enforcement of contingencies, for misbehavior. Greater parent-child conflict has been observed in adolescence for those with, versus without, childhood ADHD (Barkley, et al., 1991). Previous work with the current sample reported that perceived social support from parents was lower for adolescents with childhood ADHD than for adolescents without childhood ADHD (Molina et al., 2005), and this lower level of social support was associated with increased smoking among adolescents with childhood ADHD. Beyond this limited research, however, no studies of adolescents with ADHD histories have tested whether parent-adolescent relationship quality, specifically perceived support and conflict, is associated with delinquency and substance use in this at-risk population.
Although parental knowledge, consistency of discipline, support, and conflict are held to be distinct aspects of parenting, they are known to be intercorrelated (Dishion & MacMahon, 1998) and related to similar outcomes. As a result, it is often unclear whether a specific aspect of parenting behavior, such as successful parental monitoring or consistent discipline, is uniquely associated with child outcomes or whether general parenting efficacy across multiple domains of parenting drives child outcomes. Truly efficacious parenting may be a broad behavioral tendency of parents to be consistent in their discipline and aware of their children’s whereabouts in the context of an emotionally supportive relationship. This general parenting efficacy may underlie the positive parenting profile that Baumrind (1991) portrayed decades ago. Certainly, improving the profile of parenting, rather than one specific parenting behavior, is a treatment target in behavioral and family therapies (DeGarmo et al., 2004; Dishion & McMahon, 1998; Kazdin, 1997). If so, and particularly for children with a history of ADHD, this broad parenting efficacy could be most important. For adolescents with ADHD histories, it may be this greater tendency toward a generally more effective parenting style across multiple specific parenting behaviors that matters most for delinquency and substance use outcomes.
Finally, it remains unclear whether these widely touted parenting behaviors are similarly associated with adolescent behavior for youth with than for youth without ADHD histories. Previous parenting interventions with high risk samples have had promising results, with the intervention resulting in the use of more positive parenting behaviors and lower rates of behavior problems in children (Dishion et al., 2008; Gardner et al., 2009; Shaw et al., 2006). Within these high risk samples, the greatest effects of improved parenting were found among those at the highest levels of risk for persistent conduct problems. For example, Dishion and colleagues (2008) found that the effects of the Family Check-Up intervention were predominantly in the families in which children had the highest levels of behavior problems at initial assessment. Other high risk populations, such as adolescents with childhood ADHD, are also likely to benefit from positive parenting behaviors. However, if effective parenting strategies yield relatively greater benefits for youth at high risk of delinquency and substance use, the positive yield of successful parenting behaviors may be relatively greater for adolescents with, than without, ADHD histories.
The purpose of this study was to examine whether specific parenting behaviors are related to adolescent substance use and delinquency, above and beyond general parenting efficacy, for adolescents with and without childhood histories of ADHD. A second purpose was to test whether these associations were moderated by the presence or absence of childhood ADHD. These associations were tested using data from a follow-up study of children diagnosed with ADHD during their elementary school-aged years. Higher rates of adolescent alcohol, cigarette, and marijuana use in the adolescents with ADHD histories compared to a demographically similar group of adolescents without ADHD histories were previously reported (Molina & Pelham, 2003). In the current study, these outcomes were examined in relation to parenting practices. These associations were also tested for adolescent delinquency – a well-established mediator of substance use outcomes for teens with ADHD histories (Molina, in press). Between group (ADHD, no ADHD) differences in parenting behaviors were examined to determine whether there are differences in the perception of parenting behaviors between adolescents with and without childhood ADHD. Less parental knowledge, consistency of parental discipline, and parent-child support and more parent-child conflict were expected for adolescents with, compared to adolescents without, childhood ADHD. The direction of the relations between the parenting variables and substance use and delinquency was not expected to vary by ADHD history. However, the magnitude of these associations was expected to be higher for the adolescents with, than without, ADHD histories.
Methods
Participants
Participants were 142 adolescents with a diagnosis of ADHD in childhood and 100 demographically similar adolescents without a diagnosis of ADHD in childhood. Participants with a history of ADHD were recruited as adolescents from the Attention Deficit Disorder clinic records at Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center, for services received between the years of 1987 and 1995. The participants with childhood ADHD were comprehensively diagnosed in a research clinic during childhood using standardized diagnostic procedures and meeting DSM-III-R or DSM-IV criteria for ADHD (APA, 1987; 1994). At follow-up, 69.7% of participants with ADHD histories continued to meet DSM-III-R diagnostic criteria for ADHD (Molina & Pelham, 2003). Participants without a history of ADHD were recruited as adolescents from the greater Pittsburgh area by means of newspaper advertisements (54%), flyers in schools attended by the participants with ADHD histories (9%), advertisements in the university hospital voicemail system or newsletter which reached a large network of hospital staff (26%), or other (e.g., word of mouth; 11%).
Participants with a childhood diagnosis of ADHD were excluded from follow-up if their IQ was less than 80 or if they had a seizure disorder, other neurological problems, or history of pervasive developmental, psychotic, sexual, or organic mental disorders. Participants without a history of ADHD were excluded if they had a history or current diagnosis of ADHD based on parent and teacher reports on standardized measures in addition to the exclusion criteria used with participants with ADHD histories. No statistically significant differences between the participants with and without childhood ADHD were found for adolescent age, sex, race/ethnicity, parent education, and proportion of two-parent household. The mean age for the sample was 15.18 (SD = 1.4), and ages ranged from 13 to 18 years. Most of the adolescents (94%) were male. Eighty-seven percent of the adolescents were Caucasian, 10% were African American, and 3% had other ethnic backgrounds. The majority of the adolescents lived in two-parent households (71%). All of the mothers, and 96% of the fathers, had graduated from high school or received their high school equivalency degree, and 43% of mothers, and 46% of fathers, had graduated from college.
Procedure
All adolescents participated with their parents in a one-time, office-based interview.1 After informed consent was obtained, adolescents, mothers, and fathers were interviewed separately. Paper-and-pencil and interview questions were read aloud to adolescents, who followed along on their own copy of the measures. Interviewers recorded the answers (substance use was an exception). There were no instructions requiring adolescent use of, or abstention from, prescribed psychotropic medications during participation. Confidentiality of information was supported with a Certificate of Confidentiality from the U.S. Department of Health and Human Services with certain exceptions (e.g., suicidality, child abuse), and the protocol was approved by the University of Pittsburgh institutional review board. Additional details regarding participant recruitment and procedures can be found in Molina and Pelham (2003) and Bagwell et al. (2001).
Adolescent, rather than parent, reports of parenting behaviors were used in the current study. Previous research has indicated that adolescent reports of parenting behaviors are more closely related to observed parenting behavior and are stronger predictors of adolescent participation in problem behaviors (Latendresse et al., 2009; Sessa et al., 2001). Previous research has also found that adolescent reports of parenting behaviors are less likely to be influenced by a social desirability response set (Schwarz et al, 1985). Greater variability in adolescent than in mother reports of parenting behaviors was also found in another study of non-referred children in the community (Molina, Donovan, & Belendiuk, 2010).
Measures - Independent Variables
Parental Knowledge
Parents’ knowledge of their adolescent’s activities was assessed with adolescent report on the Parent Awareness of Child’s Activities and Interests (PACAI) scale (Lamborn et al., 1991). The five items from the questionnaire assess the adolescent’s perception of the degree to which parents are actually aware (i.e., “really know”) about their adolescent’s social and/or free-time activities during the past six months (e.g. “During the past 6 months, how much did either of your parents really know who your friends were?” and “During the past 6 months, how much did either of your parents really know what you did with your free time?”). Adolescents responded to the items using a 1 (didn’t know) to 5 (knew all of the time) scale. The Cronbach’s alpha of this scale for this sample was .82. A confirmatory factor analysis (CFA) was conducted to test the fit of a one factor model to these items. The fit statistics confirmed good fit, χ2 (5) = 5.00, p=.42; RMSEA= .002 (CI: .00~.09); CFI = 1.00.
Parental Consistency
Parental consistency was assessed using adolescent report on the consistency subscale of the Children’s Report of Parent Behavior Inventory (CRPBI; Schaefer, 1965). Adolescents reported about both parents with five items measuring consistency in rule application for the past six months (e.g., “My parents soon forgot the rules they had made,” and “My parents changed their minds to make things easier for themselves”). The response scale ranged from 1 (strongly agree) to 5 (strongly disagree). The Cronbach’s alpha of this scale for this sample was .69. A CFA was conducted to test the fit of a one factor model to these items. The fit statistics confirmed good fit, χ2 (5) = 1.96, p=.85; RMSEA= .00 (CI: .00~.05); CFI = 1.00.
Parental Support
Parental support was assessed with seven items adapted from the Network of Relationships Inventory indicating the amount of social support provided to the adolescent by each parent in the last six months (Furman & Buhrmester, 1985). Adolescents responded to the questions using a 1 (little or none) to 5 (the most possible) scale (e.g. “How much does your mother give you good advice about how to handle problems you have?” and “How much can you count on your father to be there when you need him no matter what?”). Responses about mothers and fathers were averaged for each of the seven items. The average correlation between the mother and father items was .46 (all p < .001). The Cronbach’s alpha of this scale for this sample was .79.
The seven items for parental support were reduced to four indicators by averaging selected items that were similar in content. This was done to simplify the number of latent variable indicators for the structural equation model analyses described later. Responses to six of the items were averaged in pairs, resulting in three indicators; a fourth item remained as a single indicator. The four indicators measured parental advice giving (the single item), ability to rely on parents, care and admiration expressed by parents, and enjoying time spent with parents. The fit of a one factor model using these four indicators was acceptable, χ2 (10) = 18.75, p=.04; RMSEA= .06 (CI: .01~.11); CFI = .99.
Parent-Adolescent Conflict
Adolescents reported the extent of conflict that they experienced with each of their parents using the 12 conflict items from the Robin and Foster (1989) Conflict Behavior Questionnaire. Sample items are, “My mom screams a lot.” and “We almost never seem to agree”. The response scale ranged from 1 (strongly agree) to 5 (strongly disagree). Responses about mothers and fathers were averaged for each of the 12 items. The average correlation between the mother and father items was .26 (all p < .001). The Cronbach’s alpha of this scale for this sample was .94. The 12 items were reduced to three indicators based on item content. These three indicators represented general disagreement and frustration (four items), frequency of conflict (three items), and negative behavior by parents (five items). Fit of a one factor model using these 3 indicators could not be evaluated because it was a just-identified model (i.e. the number of estimated parameters was equal to the number of elements in the covariance matrix), resulting in zero degrees of freedom.
Measures - Dependent Variables
Substance Use
Adolescent report of alcohol, tobacco, and marijuana use was assessed with a paper-and-pencil questionnaire developed for this study as an adaptation and extension of existing measures (e.g., Health Behavior Questionnaire; Jessor, Donovan, & Costa, 1989; National Household Survey of Drug Abuse, National Institute on Drug Abuse, 1992). Frequency of heavy alcohol use was defined as the mean of two questions: (a) “In the past 6 months how many times did you get drunk or ‘very, very high’ on alcohol?” and (b) “In the past 6 months how many times did you drink five or more drinks when you were drinking?” These two items were highly correlated (r = .85, p < .05). Response options for both of these questions ranged from 1 (never) to 9 (more than twice a week). Cigarette use was assessed with one question: “During the past month, how many cigarettes did you smoke on an average day?” Response options ranged from 1 (none) to 7 (about 2 packs or more a day). Marijuana use was assessed with one question: “How often in the past 6 months did you use marijuana?” Response options ranged from 1 (never) to 9 (more than twice a week).
Delinquency
Adolescent delinquency was assessed using maternal report on the Child Behavior Checklist (CBCL; Achenbach & Edelbrock, 1983). The 13 items from the delinquency subscale were used; response options were 0 (not true), 1 (somewhat or sometimes true), or 2 (very true or often true) of their child in the past six months. The final score was the sum of the responses to these items. The items are intended to provide broad but non-redundant coverage of behavioral problems than can be rated with a minimum of inference. Sample items include “Lying or cheating,” “Hangs around with others who get into trouble,” and “Truancy, skips school.”
Analytic Plan
First, between group differences (ADHD vs. no ADHD) in perceived parenting behaviors were examined using independent samples t-tests. Next, a series of structural equation models (SEMs) were estimated to examine the associations between the parenting variables and the adolescent outcomes, followed by testing between group (ADHD vs. no ADHD) equivalence in these associations. Separate models were tested for each of the four outcome variables (alcohol use, cigarette use, marijuana use, and delinquency). Analyses in structural equation modeling (SEM) were conducted using Mplus 3.1 (Muthén & Muthén, 2005). The fit of each model was evaluated with multiple fit statistics, such as the chi-square test of model fit, Root Mean Square Error of Approximation (RMSEA), and the comparative fit index (CFI).
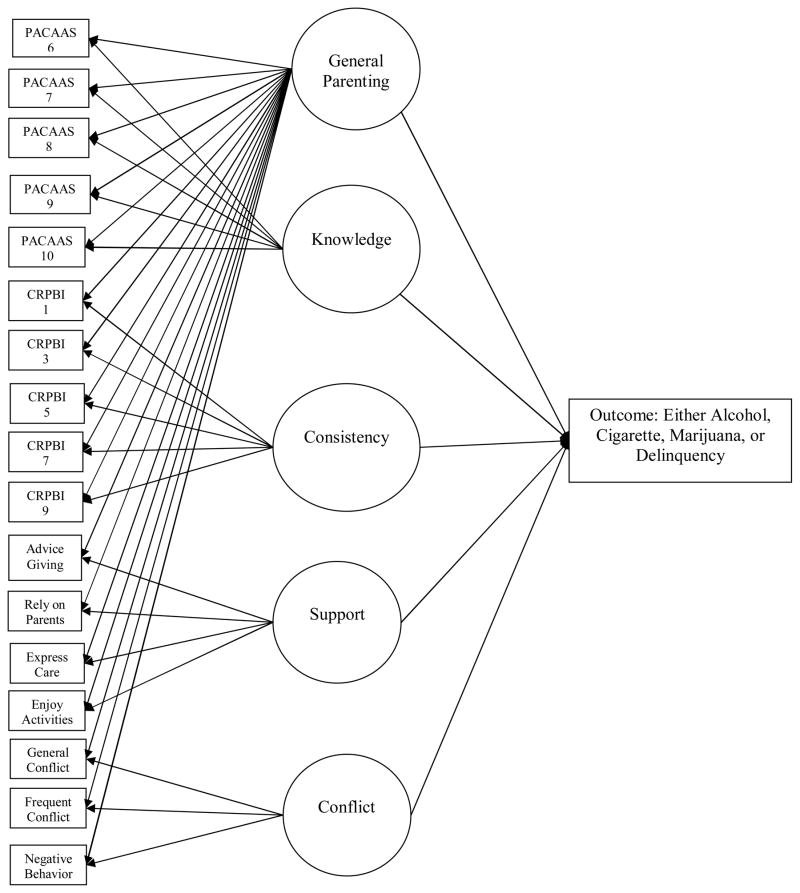
Before our primary analyses investigating the associations between parenting behaviors and outcome variables, parenting behaviors were modeled as a “general-specific” model (Gustafson & Balke, 1993) to reflect the distinctive and yet correlated nature of the different parenting behaviors. Similar to a state-trait model (Schmitt & Steyer, 1993), a general-specific model provides an opportunity to simultaneously model the trait-like general parenting factor that is common to all of the measures of parenting behaviors and several specific parenting factors that are unique to certain aspects of parenting. As can be seen in the measurement model in Figure 1, the general parenting factor is modeled by a latent factor that captures the common variance underlying all of the measured parenting items. Specific parenting factors are modeled as distinctive latent factors underlying only the relevant parenting items. In addition, the general and specific parenting factors are modeled to be uncorrelated, so that the effects of general and specific parenting factors can be examined independently above and beyond controlling for the effects of the other parenting factors (Schmitt & Steyer, 1993). The general-specific model based on parental knowledge, consistency, support, and parent-adolescent conflict fit the data well (χ2 (103) = 135.79, p=.02; RMSEA= .04 (CI: .02~.05); CFI = .98).
Figure 1.
General-Specific Model as Used in the Analyses.
Once a general-specific model for parenting behaviors was established, this model was compared between the participants with and without childhood ADHD and tested for measurement invariance. Partial invariance in the parenting measurement model was supported, as all but three parameters were not significantly different across groups. Specifically, one factor loading (the loading of the single support item on the general parenting factor) and two of the residual variances of the indicators (two of the parental knowledge indicators) were significantly different between the participants with and without ADHD histories. Thus, equivalent parameters were held constant across groups in the subsequent analyses.
To test the hypothesis that childhood ADHD moderates the association between parenting behaviors and adolescent outcomes, each of the substance use variables and the delinquency variable were examined in separate SEM models. All reported results were compared with the results of models tested with robust estimators; the overall patterns of findings were not different. In addition, each model was estimated in a multigroup analysis framework with ADHD as the grouping variable. The equivalence of the relations between the parenting factors and the outcome variables was tested using chi-square difference tests to compare the models with and without equivalence constraints. In the base model, all of the relations between the parenting factors and the outcome variables were freely estimated across groups. In the subsequent models, each relation was constrained to be equal across groups one at a time, followed by testing whether the model fit significantly changed with the additional constraint. Significant moderation by childhood ADHD was supported by a statistically significant change in the chi-square statistic, which indicates between group differences in the path coefficients relating the parenting factors and the outcome variable.
Results
Group differences in parenting behaviors and adolescent outcomes
The results of the ADHD history-no ADHD history group comparisons for the parenting, parent-child relationships, delinquency, and substance use variables are in Table 1. As previously reported for this sample (Molina & Pelham, 2003; Marshal et al., 2003; Molina et al., 2005), the participants with a history of ADHD reported significantly more frequent heavy alcohol use, more cigarette use, and more marijuana use compared to the participants without a history of ADHD. Additionally, the participants with a history of ADHD had significantly higher levels of delinquent behavior on average than did the participants without a history of ADHD based on maternal reports. The magnitudes of these effects were small for heavy alcohol use (d = .39), medium for cigarette use (d = .64), small for marijuana use (d = .48), and large for delinquency (d = 1.78). (“Small,” “medium,” and “large” effect sizes defined per Cohen, 1992).
Table 1.
Descriptive Information and Differences in Predictor and Outcome Variables for Participants with and without childhood ADHD.
| ADHD | No ADHD | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean | SD | Mean | SD | t-test | Cohen’s d | |
| Outcomes | ||||||
| Heavy Alcohol Use | 1.84 | 1.62 | 1.43 | 1.06 | −2.24* | .30 |
| Smoking Quantity | 2.00 | 1.32 | 1.39 | .95 | −3.32* | .53 |
| Marijuana Use | 2.74 | 6.16 | .67 | 3.55 | −2.65** | .41 |
| Delinquency | 3.96 | 3.88 | 1.00 | 1.66 | −7.08*** | .99 |
| Predictors | ||||||
| Parental Knowledge | 3.44 | .97 | 3.77 | .73 | 2.95* | .38 |
| Parental Consistency | 3.41 | .72 | 3.61 | .66 | 2.17* | .29 |
| Parental Support | 3.25 | .74 | 3.64 | .64 | 4.22*** | .56 |
| Parental Conflict | 3.06 | .29 | 3.20 | .21 | 3.90*** | .55 |
p<.10,
p<.05,
p<.01,
p<.001
For all of the parenting measures, a higher score is equal to better parenting behavior; including conflict (i.e. higher score on the conflict measure means less conflict in parent-adolescent relationship).
For the parenting and parent-adolescent relationship variables, the participants with a childhood ADHD diagnosis reported significantly less parental knowledge, less parental consistency, less parental support, and more parent-adolescent conflict (lower scores reflected higher conflict on this measure), on average, than did the participants without a childhood ADHD diagnosis. The magnitudes of these effects were small for parental knowledge (d = .45) and consistency (d = .30) and medium for parental support (d = .61) and parent-adolescent conflict (d = .67) (Cohen, 1992). The finding for parental support was previously published (Molina et al., 2005) but is included here for descriptive purposes.
Associations between parenting and adolescent outcomes
Heavy Alcohol Use
The standardized coefficients, R2 statistics, and chi-square difference tests comparing the path coefficients, from the parenting factors to alcohol use, between the participants with and without a childhood ADHD diagnosis can be seen in Table 2. The model for heavy alcohol use fit the data adequately for the entire sample, χ2 (284) = 363.34, p < .01; RMSEA = .05 (CI: .03~.06); CFI = .95. For both the participants with and without childhood ADHD, parental knowledge was significantly and negatively associated with alcohol use above and beyond the general and the other specific parenting behaviors. A chi-square difference test comparing models, one in which the relation between knowledge and heavy alcohol use was freely estimated across groups and another in which the relation was constrained to be equal across groups, was statistically significant, Δχ2 (1) = 3.68, p = .05, indicating that the strength of the relation between knowledge and heavy alcohol use was significantly different between the participants with a history of ADHD and participants without a history of ADHD. The parental knowledge path coefficient for the ADHD group (standardized B = −.69) was larger than the same path coefficient for the group without childhood ADHD (B = −.25). Thus, more parental knowledge was associated with lower levels of alcohol use for both groups, but the association was significantly stronger for the ADHD group than for the group without childhood ADHD. Reflecting this result, the proportion of the variance in alcohol use (R2) explained by the parenting factors was higher for the ADHD group than for the group without childhood ADHD. None of the other parenting variables, including the general parenting factor, were significantly associated with alcohol use for either group.
Table 2.
Standardized regression coefficients, variances, and chi-square difference tests.
| ADHD | no ADHD | ||||
|---|---|---|---|---|---|
|
| |||||
| β | R2 | β | R2 | χ2 Test for Group Differences | |
| Heavy Alcohol Use | .21 | .06 | |||
| General Parenting | −.21 | .02 | 1.41 | ||
| Knowledge | −.69*** | −.25+ | 3.68* | ||
| Consistency | .13 | −.01 | .39 | ||
| Support | .07 | .05 | .04 | ||
| Conflict | −.12 | .02 | .46 | ||
| Cigarette Use | .23 | .12 | |||
| General Parenting | −.05 | −.03 | .003 | ||
| Knowledge | −.60** | −.26* | .84 | ||
| Consistency | .14 | −.07 | .73 | ||
| Support | .14 | .10 | .01 | ||
| Conflict | .01 | .16 | .53 | ||
| Marijuana Use | .20 | .13 | |||
| General Parenting | −.28 | .05 | 1.29 | ||
| Knowledge | −1.06*** | −.47** | 1.35 | ||
| Consistency | .31 | −.22 | 2.69 | ||
| Support | −.13 | .07 | .15 | ||
| Conflict | −.01 | .12 | .10 | ||
| Delinquency | .16 | .13 | |||
| General Parenting | −1.21*** | .03 | 9.41** | ||
| Knowledge | −.87* | −.55** | .02 | ||
| Consistency | .41 | −.12 | 1.42 | ||
| Support | −.02 | −.22 | .26 | ||
| Conflict | .17 | .08 | .05 | ||
p<.10,
p<.05,
p<.01,
p<.001
Chi-square difference tests were conducted to determine if significant differences between ADHD and no ADHD groups for the parenting variables were present. Variance accounted for in the outcome variables by the parenting variables is also reported.
Cigarette Quantity
Similar to the model predicting heavy alcohol use, the fit statistics suggested adequate model fit for the entire sample, χ2 (284) = 357.86, p < .01; RMSEA = .05 (CI: .03~.06); CFI = .95. For both the participants with and without childhood ADHD, knowledge was significantly and negatively associated with cigarette use above and beyond the general and the other specific parenting behaviors. A chi-square difference test comparing models with and without the constraint on the relation between knowledge and cigarette use was not statistically significant, Δχ2 (1) = .84, p = .36, indicating that the strength of the relation between knowledge and cigarette use was not significantly different between the participants with and without a childhood diagnosis of ADHD. These findings show that more parental knowledge was associated with lower levels of cigarette use for both groups, but the association was not significantly stronger for the ADHD group than for the group without childhood ADHD. The proportion of the variance in cigarette use explained by the parenting factors was somewhat larger for the ADHD group than for the group without childhood ADHD. None of the other parenting variables were significantly associated with cigarette use for either group.
Marijuana Use
The fit statistics suggested adequate model fit for the entire sample, χ2 (284) = 349.62, p < .01; RMSEA= .04 (CI: .03~.06); CFI = .96. For both the participants with and without ADHD histories, knowledge was significantly and negatively associated with marijuana use above and beyond the general and the other specific parenting behaviors. A chi-square difference test comparing models with and without the constraint on the relation was not statistically significant, Δχ2 (1) = 1.35, p = .25, indicating that the strength of the relation between knowledge and marijuana use was not significantly different between the participants with and without a childhood diagnosis of ADHD. Similar to the results for heavy alcohol and cigarette use, more parental knowledge was associated with lower levels of marijuana use for both groups. However, like the findings for cigarette use, the association was not significantly stronger for the ADHD group than for the group without childhood ADHD. The proportion of the variance in marijuana use explained by the parenting factors was somewhat larger for the ADHD group than for the group without childhood ADHD. None of the other parenting variables were significantly associated with marijuana use for either group.
Delinquency
The fit statistics suggested adequate model fit, χ2 (284) = 346.68, p < .01; RMSEA= .04 (CI: .02~.06); CFI = .96. For both the participants with and without childhood ADHD, knowledge was significantly and negatively associated with delinquency above and beyond the general and the other specific parenting behaviors. A chi-square difference test comparing models with and without the constraint on the relation was not statistically significant, Δχ2 (1) = .02, p = .88, indicating that the strength of the association between knowledge and delinquency was not significantly different between the participants with and without a history of ADHD. Thus, more parental knowledge was associated with lower levels of delinquency similarly for both groups. For the ADHD group, the general parenting variable was also significantly and negatively associated with a lower delinquency score, but not for the group without childhood ADHD. Despite the stronger association between general parenting and delinquency for the participants with a history of ADHD, the proportions of variance accounted for by parenting were similar between the two groups. Results were compared with age- and sex-adjusted t-scores for the delinquency subscale of the CBCL, and no differences in the overall pattern of the results were found.
Discussion
The purpose of this study was to determine whether positive parenting behaviors are associated with less substance use and delinquency by adolescents with, versus without, childhood ADHD. The shared and unique effects of four parenting variables were examined in relation to four adolescent problem behaviors for which childhood ADHD is a known risk factor. Adolescents with childhood ADHD reported that their parents used lower levels of positive parenting behaviors, including knowledge, consistency, support, and more conflict, and that they engaged in higher levels of problem behaviors, including substance use (alcohol, cigarette, and marijuana use) and delinquency, compared to adolescents without childhood ADHD. The ADHD group differences in substance use were previously reported (Molina & Pelham, 2003). The associations between parenting behaviors and adolescent problem behaviors revealed that parental knowledge, but not the other parenting variables, was significantly related to substance use and delinquency for all adolescents regardless of their ADHD histories. The findings also revealed a relatively stronger relation between parental knowledge and alcohol use for adolescents with, versus without, ADHD histories. To our knowledge, these findings are the first to suggest that parental awareness of their teen’s activities and whereabouts is an important component of a lowered risk environment for substance use and delinquency among youth with childhood ADHD. Other specific parenting behaviors (e.g., discipline consistency, support, and conflict) and general parenting efficacy did not show strong associations with adolescent problem behavior, with the exception of a negative relation between general parenting efficacy and delinquency for adolescents with childhood ADHD.
The lower levels of positive parenting behaviors reported by adolescents with histories of childhood ADHD were consistent with, and expanded upon, prior research reporting higher levels of conflict between children diagnosed with ADHD and their parents (Edwards et al., 2001; Fischer, 1990). There are several explanations for these findings. Prior studies have shown that oppositional behaviors characteristic of some adolescents with childhood ADHD may exacerbate negative/controlling parenting behavior (Barkley & Cunningham, 1979; Lang et al., 1999). Oppositionality by some adolescents with childhood ADHD may amplify the normal strain found in parent-adolescent relationships (Elder et al., 1986). As a result, parents of adolescents with ADHD histories may utilize more negative and fewer positive parenting behaviors. Parents of adolescents with childhood ADHD may also underuse positive parenting strategies due to their own mental health struggles. Parents of children with ADHD have higher rates of antisocial personality disorder, alcoholism, depression, and ADHD (Biederman et al., 1995; Chronis et al. 2003; Cummings & Davies, 1994; Faraone et al., 2005; Marshal et al., under review; Minde et al., 2003, Nigg & Hinshaw, 2003; Pelham et al., 1997; Pelham et al., 1998; Stewart et al., 2006), and these mental health problems are associated with lower levels of positive parenting practices (Arnold et al., 1997; Chronis-Tuscano et al., 2008; Cummings & Davies, 1994; Jackson et al., 1999; Murray & Johnston, 2006; Patterson et al., 1990). Examining parents’ ADHD symptoms, with its concomitant measurement difficulties (Barkley, 1997; Fischer, 1997; Smith et al., 2000; Wender, 1995), and other psychopathology was beyond the scope of the current study. However, these child and parent characteristics, and their potential roles in the associations studied herein, are important to consider in the larger context of the family affected by ADHD. Further investigation of parental psychopathology and gene-environment interactions (Rutter, 2006), as well as longitudinal research that considers bidirectional relations between parenting and child behaviors in families affected by ADHD, would improve understanding of the parenting environment and contributing variables.
The parenting behaviors in this study were reported by adolescents. Relying on adolescent perception of parenting practices is a strategy that has gained traction in teen mental health research due to the tendency of parents’ reports to be biased in favor of socially desirable responses (Steinberg, 2001). Moreover, as indicated earlier, adolescent reports of parenting behaviors are more closely related to observed parenting behaviors and are stronger predictors of adolescent participation in problem behaviors (Latendresse et al., 2009; Sessa et al., 2001). Whether adolescents with ADHD histories are capable of judging their parents’ behavior accurately, given their tendency toward positively biased reports about themselves, is a continuing question in the literature (Owens & Hoza, 2003). In a prior study, perceptions of inter-parental discord were correlated similarly between teens and their parents regardless of ADHD history, and ADHD group differences in parents’ relationship difficulties (e.g., frequency of conflict between parents) were only observed on the basis of teen (not mother) report (Wymbs et al., 2008). Thus, for certain parent behaviors, teen perception may be more useful than parent self-report.
When modeling the general and specific parenting behaviors simultaneously, parental knowledge emerged as the parenting variable with the strongest negative associations with adolescent problem behaviors. These associations extend findings from previous research with community samples (Granic et al., 2003; Nash et al., 2005) to the ADHD population. The results suggest the possibility that parent and teen behaviors that promote parental knowledge are uniquely protective for both adolescents with and without childhood ADHD for two behavior domains known to be related and particularly problematic for children with ADHD (substance use and delinquency). These findings are especially meaningful in light of the now-demonstrated persistence of ADHD symptoms and impairments for many children with ADHD (Barkley et al., 1990; Molina et al. 2009), the importance of ADHD symptom persistence and adolescent conduct problems as correlates of adolescent substance use (Molina & Pelham, 2003), the limitations of medication treatment as applied to teenagers with ADHD (Pelham & Fabiano, 2008), and the limited data available about psychosocial treatment efficacy for adolescent ADHD (Pelham & Fabiano, 2008). The negative association between parental knowledge and problem behaviors for adolescents with ADHD histories suggests that increased parental awareness of their teens’ activities and whereabouts, whether through active monitoring efforts or through teen disclosure, might attenuate the impact of these otherwise heightened risks. It is important to note that knowledge was significant when controlling for parenting behaviors thought to encourage adolescent disclosure, such as relational support and low parent-adolescent conflict. As a result, future research should investigate the role of adolescent disclosure in the relations between parental knowledge and adolescent substance use and delinquency.
The protective association between parental knowledge and heavy alcohol use was stronger for the adolescents with, compared to without, childhood ADHD. This stronger association indicates that adolescents with childhood ADHD might benefit more from increased parental monitoring efforts than normative adolescents. If so, this is consistent with the parenting intervention literature in which the greatest effects of improved parenting were found among those at the highest levels of risk for persistent conduct problems (Dishion et al., 2008; Gardner et al., 2009; Shaw et al., 2006). ADHD participants are at increased risk for problem behavior, and persistent ADHD symptoms and concurrent CD are strongly associated with adolescent substance use in this (Molina & Pelham, 2003) and in subsequent (Molina et al., 2007) samples. Thus, parents of these highest risk youth may have more opportunities to affect vulnerability through vigilant monitoring and frequent discourse compared to parents of adolescents without childhood ADHD. It is important for future research to continue to examine the associations between parenting and outcomes for at-risk youth. It is common for adolescents to seek independence (Eccles, 2003); although this independence has positive outcomes for many adolescents, for those at risk for participation in problem behaviors, such as those with ADHD histories, greater independence could be associated with negative outcomes.
Both parental knowledge and general parenting efficacy were significantly related to lower levels of delinquency for the participants with a history of ADHD, but only knowledge was significantly related to delinquency for the nonADHD comparison group. These findings may be driven by the large group difference in delinquency (a full standard deviation) and accompanying increased opportunity to detect more associations between delinquency and parenting relative to substance use and parenting. In addition, delinquency (unlike substance use) was reported by the adolescents’ mothers rather than by the adolescents themselves. Using adolescent-report of delinquency is sometimes discouraged when studying at-risk youth (Hindelang et al., 1981), and the use of maternal report of delinquency might be a strength of the current study. However, this difference in reporters may also explain the lack of a significant relation between general parenting efficacy and delinquency for the nonADHD comparison group. Use of the general-specific model to test the associations between parenting and problem behavior was a unique strength of the study that allowed the relation between general parenting efficacy and delinquency for the ADHD group to be detected. The general-specific parenting model allowed us to separate out the associations between specific parenting behaviors and problems behaviors from the associations between general parenting tendencies and problem behaviors. Thus, the current study also demonstrated the utility of general-specific factor models in examining distinct yet correlated constructs which are prevalent in psychological research.
The negative association between parental knowledge and alcohol use by adolescents with ADHD, if replicated in longitudinal study, suggests potential benefits associated with the teaching of specific parenting behaviors that promote parental awareness (e.g., behavioral parent training) in the treatment of adolescents with childhood ADHD. Previous work has found parent training to be an effective strategy in the treatment of childhood ADHD, but there are very few studies of parent training or family therapy for adolescent ADHD (Fabiano et al., 2009; Pelham & Fabiano, 2008). It is common practice for interventions targeting risk for adolescent delinquency to incorporate parent management training (e.g., Henggeler, 2003). These interventions are associated with improved parenting skills and behavioral outcomes (Connell & Dishion, 2008; Dishion et al., 2003). Similarly, many adolescent substance use interventions incorporating parenting and family work have positive effects on substance use (Winters, 1999). Modifications to existing parent training programs for children with ADHD that incorporate the teaching of developmentally relevant parenting strategies may result in more efficacious outcomes for teens with ADHD. For example, treatment programs could include strategies that not only utilize increased parental monitoring but also encourage parent-adolescent communication about friendships, activities, and whereabouts. As the current study only included adolescents, future research is needed to assess whether specific parenting behaviors have the same impact across development for those with childhood ADHD. The impact of specific parenting behaviors tends to differ with development for typically developing adolescents (Bingham & Shope, 2004). Regardless of the differential impacts of parenting behaviors during development, efforts to support effective parenting in adolescence may be important and could be addressed through the addition of periodic parent training booster sessions to parent training packages delivered in childhood (Conduct Problems Prevention Group, 2007).
Despite the strengths of the current study, certain characteristics of the sample may limit the generalizability of the findings to other populations. First, the sample was primarily male and Caucasian and it was not possible to examine interactions with gender or race/ethnicity. Second, the average education of the parents was higher than that of average parents in Pennsylvania. Considering that parental education is moderately associated with the use of effective parenting practices (Belsky et al., 2006), associations between parenting behaviors and the problem behaviors might have been different in a sample more representative of adult education statewide. Third, the participants with childhood ADHD were recruited from clinic records. Because the parents of the adolescents with childhood ADHD sought treatment for their child’s ADHD, they may not be typical of all parents of adolescents with ADHD histories. Finally, the associations examined were primarily cross-sectional in nature. Although it was beyond the scope of the current study to incorporate additional aspects of parent (e.g., alcoholism, antisociality, ADHD) and child (conduct problem trajectory over time) behaviors and their reciprocal associations over time, future studies would benefit from such examination.
Parenting has been consistently identified as an important influence on adolescent behavior. The current study suggests that parental knowledge is a key component of the parenting environment for adolescents with and without ADHD histories. Moreover, parental knowledge of their teens’ activities and whereabouts may be particularly reflective of ADHD risk of alcohol use. This is a novel and important finding given the risk of substance use among adolescents with childhood ADHD (Molina, in press). Future studies that attempt to distinguish between parental efforts to monitor and teen decisions to disclose may be beneficial. The findings also suggest that the parenting environment continues to play an important role in adolescent behavioral risk and that continued efforts to improve it may be worthwhile.
Acknowledgments
This research was supported by K21 AA00202 and AA0011873 from the National Institute of Alcohol Abuse and Alcoholism and by grant DA12414 from the National Institute on Drug Abuse.
Footnotes
A subset of these participants provided subsequent interviews as part of the Pittsburgh ADHD Longitudinal Study (Molina et al., 2007).
References
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University Associates in Psychiatry; 1983. [Google Scholar]
- Ackard DM, Neumark-Sztainer D, Story M, Perry C. Parent-child connectedness and behavioral and emotional health among adolescents. American Journal of Preventive Medicine. 2006;30:59–66. doi: 10.1016/j.amepre.2005.09.013. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. Washington, DC: American Psychiatric Association; 1987. rev. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revised. [Google Scholar]
- Arnold EH, O’Leary SG, Edwards GH. Father involvement and self-reported parenting of children with Attention Deficit-Hyperactivity Disorder. Journal of Consulting and Clinical Psychology. 1997;65:337–342. doi: 10.1037/0022-006X.65.2.337. [DOI] [PubMed] [Google Scholar]
- Bagwell C, Molina BSG, Pelham WE, Hoza B. Attention-deficit hyperactivity disorder and problems in peer relations: Predictions from childhood to adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1285–1292. doi: 10.1097/00004583-200111000-00008. [DOI] [PubMed] [Google Scholar]
- Bahr SJ, Hoffmann JP. Parenting style, religiosity, peers, and adolescent heavy drinking. Journal of Studies on Alcohol and Drugs. 2010;71:539–543. doi: 10.15288/jsad.2010.71.539. [DOI] [PubMed] [Google Scholar]
- Bailey JA, Hill KG, Oesterle S, Hawkins JD. Parenting practices and problem behavior across three generations: Monitoring, harsh discipline, and drug use in the intergenerational transmission of externalizing behavior. Developmental Psychology. 2009;45:1214–1226. doi: 10.1037/a0016129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA. ADHD and the nature of self-control. New York: Guilford; 1997. [Google Scholar]
- Barkley RA. Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment. 2. New York: Guilford Press; 1998. [Google Scholar]
- Barkley RA. Attention-Deficit/Hyperactivity Disorder. In: Mash EJ, Barkley RA, editors. Child Psychopathology. 2. New York: Guildford Press; 2003. pp. 75–143. [Google Scholar]
- Barkley RA, Cunningham CE. The effects of methylphenidate on the mother-child interactions of hyperactive children. Archives of General Psychiatry. 1979;36:201–208. doi: 10.1001/archpsyc.1979.01780020091010. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Edwards G, Laneri M, Fletcher K, Metevia L. The efficacy of problem-solving communication training alone, behavior management training alone, and their combination for parent–adolescent conflict in teenagers with ADHD and ODD. Journal of Consulting and Clinical Psychology. 2001;69:926–941. [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria, I: An 8 year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria, III: Mother-child interactions, family conflicts, and maternal psychopathology. Journal of Child Psychology and Psychiatry. 1991;32:233–256. doi: 10.1111/j.1469-7610.1991.tb00304.x. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Guevremont DC, Anastopoulos AD, Fletcher KE. A comparison of three family therapy programs for treating family conflicts in adolescents with attention-deficit hyperactivity disorder. Journal of Consulting and Clinical Psychology. 1992;60:450–462. doi: 10.1037/0022-006X.60.3.450. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, Fischer M. ADHD in adults: What the science says. New York: Guilford Press; 2008. [Google Scholar]
- Barnes GM, Hoffman JH, Welte JW, Farrell MP, Dintcheff BA. Effects of parental monitoring and peer deviance on substance use and delinquency. Journal of Marriage and Family. 2006;68:1084–1104. [Google Scholar]
- Baumrind D. Effective parenting during the early adolescent transition. In: Cowan PA, Hetherington EM, editors. Family transitions. Hillsdale, NJ: Lawrence Erlbaum; 1991. pp. 111–163. [Google Scholar]
- Belsky J, Bell B, Bradley RH, Stallard N, Stewart-Brown SL. Socioeconomic risk, parenting during the preschool years and child health age 6 years. European Journal of Public Health. 2006;17:508–513. doi: 10.1093/eurpub/ckl261. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone S, Milberger S, Guite J, Mick E, Chen L, Mennin D, Marrs A, Ouellette C, Moore P, Spencer T, Norman D, Wilens T, Kraus I, Perrin J. A prospective 4-year follow-up study of Attention-Deficit Hyperactivity and Related Disorders. Archives of General Psychiatry. 1996;53:437–446. doi: 10.1001/archpsyc.1996.01830050073012. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Mick E, Spencer T, Wilens T, Kiely K, Guite J, Ablon JS, Reed E, Warburton R. High risk for attention deficit hyperactivity disorder among children of parents with childhood onset of the disorder: A pilot study. American Journal of Psychiatry. 1995;152:431–435. doi: 10.1176/ajp.152.3.431. [DOI] [PubMed] [Google Scholar]
- Bingham CR, Shope JT. Adolescent developmental antecedents of risky driving among young adults. Journal of Studies on Alcohol. 2004;65:84–94. doi: 10.15288/jsa.2004.65.84. [DOI] [PubMed] [Google Scholar]
- Chassin L, Presson CC, Rose J, Sherman SJ, Davis MJ, Gonzalez JL. Parenting style and smoking-specific parenting practices as predictors of adolescent smoking onset. Journal of Pediatric Psychology. 2005;30:333–344. doi: 10.1093/jpepsy/jsi028. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Chacko A, Fabiano GA, Wymbs BT, Pelham WE. Enhancements to the behavioral parent training paradigm for families of children with ADHD: Review and future directions. Clinical Child and Family Psychology Review. 2004;7:1–27. doi: 10.1023/b:ccfp.0000020190.60808.a4. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Lahey BB, Pelham WE, Kipp H, Baumann BL, Lee SS. Psychopathology and substance abuse in parents of young children with attention-deficit hypactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1424–1432. doi: 10.1097/00004583-200312000-00009. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Raggi VL, Clarke TL, Rooney ME, Diaz Y, Pian J. Associations between maternal attention-deficit/hyperactivity disorder symptoms and parenting. Journal of Abnormal Child Psychology. 2008;36:1237–1250. doi: 10.1007/s10802-008-9246-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Connell A, Dishion TJ. Reducing depression among at-risk early adolescents: Three-year effects of a family-centered intervention embedded within schools. Journal of Family Psychology. 2008;22:574–585. doi: 10.1037/0893-3200.22.3.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conduct Problems Prevention Research Group. Fast track randomized controlled trial to prevent externalizing psychiatric disorders: Findings from grades 3 to 9. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1250–1262. doi: 10.1097/chi.0b013e31813e5d39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger RD, Ge X. Conflict and cohesion in parent-adolescent relations: Changes in emotional expression from early to midadolescence. In: Cox MJ, Brooks-Gunn J, editors. Conflict and cohesion in families: Causes and consequences. Mahwah, NJ: Erlbaum; 1999. pp. 185–206. [Google Scholar]
- Cummings EM, Davies PT. Maternal depression and child development. The Journal of Child Psychology and Psychiatry. 1994;35:73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Danforth JS, Barkley RA, Stokes TF. Observations of parent-child interactions with hyperactive children: Research and clinical implications. Clinical Psychology Review. 1991;11:703–727. [Google Scholar]
- DeGarmo DS, Patterson GR, Forgatch MS. How do outcomes in a specified parent training intervention maintain or wane over time? Prevention Science. 2004;5:73–89. doi: 10.1023/b:prev.0000023078.30191.e0. [DOI] [PubMed] [Google Scholar]
- De Goede IH, Branje SJ, Meeus WH. Developmental changes in adolescents’ perceptions of relationships with their parents. Journal of Youth and Adolescence. 2009;38:75–88. doi: 10.1007/s10964-008-9286-7. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, McMahon RJ. Parental monitoring and the prevention of child and adolescent problem behavior: A conceptual and empirical formulation. Clinical Child and Family Psychology Review. 1998;1:61–75. doi: 10.1023/a:1021800432380. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Nelson SE, Kavanagh K. The family check-up with high-risk young adolescents: Preventing early-onset substance use by parent monitoring [Special issue] Behavior Therapy. 2003;34:553–571. [Google Scholar]
- Dishion TJ, Patterson GR, Reid JB. Parent and peer factors associated with drug sampling in early adolescence: Implications for treatment. In: Rahdert ER, Grabowski J, editors. Adolescent drug abuse: Analyses of treatment research (NIDA Research Monograph No. 77) Washington, DC: U.S. Government Printing Office; 1988. pp. 69–93. [PubMed] [Google Scholar]
- Dishion TJ, Shaw D, Connell A, Gardner F, Weaver C, Wilson M. The family check-up with high-risk indigent families: Preventing problem behavior by increasing parents’ positive behavior support in early childhood. Child Development. 2008;79:1395–1414. doi: 10.1111/j.1467-8624.2008.01195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Johnson W, McGue M, Iacono WG. Parental monitoring, personality, and delinquency: Further support for a reconceptualization of monitoring. Journal of Research in Personality. 2009;43:49–59. doi: 10.1016/j.jrp.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles J, Wigfield A, Byrnes J. Cognitive development in adolescence. In: Lerner RM, Easterbrooks MA, Mistry J, editors. Handbook of psychology: Vol. 6. Developmental psychology. New York: Wiley; 2003. pp. 325–350. [Google Scholar]
- Edwards G, Barkley RA, Laneri M, Fletcher K, Metevia L. Parent-adolescent conflict in teenagers with ADHD and ODD. Journal of Abnormal Child Psychology. 2001;29:557–572. doi: 10.1023/a:1012285326937. [DOI] [PubMed] [Google Scholar]
- Elder GH, Jr, Caspi A, Nguyen TV. Resourceful and vulnerable children: Family influences in stressful times. In: Silbereisen RK, Eyferth K, editors. Development as action in context. Berlin: Springer Verlag; 1986. pp. 167–186. [Google Scholar]
- Engels RCME, van der Vorst H. The roles of parents in adolescent and peer alcohol consumption. Netherlands’ Journal of Social Sciences. 2003;39:53–68. [Google Scholar]
- Fabiano GA, Pelham WE, Coles EK, Gnagy EM, Chronis-Tuscano A, O’Connor BC. A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clinical Psychology Review. 2009;29:129–140. doi: 10.1016/j.cpr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, Sklar P. Molecular genetics of attention-deficit/hyperactivity disorder. Biological Psychiatry. 2005;57:1313–1323. doi: 10.1016/j.biopsych.2004.11.024. [DOI] [PubMed] [Google Scholar]
- Feinberg ME, McHale SM, Crouter AC, Cumsille P. Sibling differentiation: Sibling and parent relationship trajectories in adolescence. Child Development. 2003;74:1261–1274. doi: 10.1111/1467-8624.00606. [DOI] [PubMed] [Google Scholar]
- Fischer M. Parenting stress and the child with attention deficit hyperactivity disorder. Journal of Clinical Child Psychology. 1990;19:337–346. [Google Scholar]
- Fischer M. Persistence of ADHD into adulthood: It depends on whom you ask. The ADHD Report. 1997;5:8–10. [Google Scholar]
- Fleming CB, Kim H, Harachi TW, Catalano RF. Family processes for children in early elementary school as predictors of smoking. Journal of Adolescent Health. 2002;30(3):184–189. doi: 10.1016/s1054-139x(01)00327-5. [DOI] [PubMed] [Google Scholar]
- Furman W, Buhrmester D. Children’s perceptions of the personal relationships in their social network. Developmental Psychology. 1985;21(6):1016–1024. [Google Scholar]
- Gardner F, Connell A, Trentacosta CJ, Shaw DS, Dishion TJ, Wilson MN. Moderators of outcome in a brief family-centered intervention for preventing early problem behavior. Journal of Consulting and Clinical Psychology. 2009;77:543–553. doi: 10.1037/a0015622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granic I, Dishion TJ, Hollenstion T. The family ecology of adolescence: A dynamic systems perspective on normative development. In: Adams GR, Berzonsky MD, editors. Blackwell handbook of adolescence. Malden, MA: Blackwell; 2003. pp. 60–91. [Google Scholar]
- Gittelman R, Mannuzza S, Shenker R, Bonagura N. Hyperactive boys almost grown up. I. Psychiatric status. Archives of General Psychology. 1985;42:937–947. doi: 10.1001/archpsyc.1985.01790330017002. [DOI] [PubMed] [Google Scholar]
- Gorman-Smith D, Tolan PH, Loeber R, Henry DB. Relation of family problems to patterns of delinquent involvement among urban youth. Journal of Abnormal Child Psychology. 1998;26:319–333. doi: 10.1023/a:1021995621302. [DOI] [PubMed] [Google Scholar]
- Gustafsson JE, Balke G. General and specific abilities as predictors of school achievement. Multivariate Behavioral Research. 1993;28:407–434. doi: 10.1207/s15327906mbr2804_2. [DOI] [PubMed] [Google Scholar]
- Henggeler SW. Commentary on Ellis and colleagues: Adapting multisystemic therapy for challenging clinical problems in children and adolescents. Journal of Pediatric Psychology. 2003;28:295–297. [Google Scholar]
- Hill KG, Hawkins JD, Catalano RF, Abbott RD, Guo J. Family influences on the risk of daily smoking initiation. Journal of Adolescent Health. 2005;37:202–210. doi: 10.1016/j.jadohealth.2004.08.014. [DOI] [PubMed] [Google Scholar]
- Hindelang MJ, Hirschi T, Weis JG. Measuring Delinquency. Thousand Oaks, CA: Sage; 1981. [Google Scholar]
- Hinshaw SP, Owens EB, Wells KC, Kraemer HC, Abikoff HB, Arnold LE, Conners CK, Elliott G, Greenhill LL, Hechtman L, Hoza B, Jensen PS, March JS, Newcorn JH, Pelham WE, Swanson JM, Vitiello B, Wigal T. Family processes and treatment outcomes in the MTA: Negative/ineffective parenting practices in relation to multimodal treatment. Journal of Abnormal Child. 2000;28:555–568. doi: 10.1023/a:1005183115230. [DOI] [PubMed] [Google Scholar]
- Jackson C, Henriksen L, Dickinson D. Alcohol-specific socialization, parenting behaviors and alcohol use by children. Journal of Studies on Alcohol. 1999;60:362–367. doi: 10.15288/jsa.1999.60.362. [DOI] [PubMed] [Google Scholar]
- Jessor R, Donovan JE, Costa FM. Health Behavior Questionnaire. Boulder: Institute of Behavioral Science, University of Colorado; 1989. [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development. New York: Academic Press, Inc; 1977. [Google Scholar]
- Katusic SK, Barbaresi WJ, Colligan RC, Weaver AL, Leibson CL, Jacobsen SJ. Psychostimulant treatment and risk for substance abuse among young adults with a history of attention-deficit/hyperactivity disorder: A population-based, birth cohort study. Journal of Child and Adolescent Psychopharmacology. 2005;15:764–776. doi: 10.1089/cap.2005.15.764. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Parent management training: Evidence, outcomes, and issues. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1349–1356. doi: 10.1097/00004583-199710000-00016. [DOI] [PubMed] [Google Scholar]
- Lamborn S, Mounts NS, Steinberg L, Dornbusch S. Patterns of competence and adjustment among adolescents from authoritative, authoritarian indulgent and neglectful families. Child Development. 1991;62:1049–1055. doi: 10.1111/j.1467-8624.1991.tb01588.x. [DOI] [PubMed] [Google Scholar]
- Lang AR, Pelham WE, Atkeson BM, Murphy DA. Effects of alcohol intoxication on parenting behavior interactions with child confederates exhibiting normal or deviant behaviors. Journal of Abnormal Child Psychology. 1999;27:177–189. doi: 10.1023/a:1021996122095. [DOI] [PubMed] [Google Scholar]
- Latendresse SJ, Rose RJ, Viken RJ, Pulkkinen L, Kaprio J, Dick DM. Parental socialization and adolescents’ alcohol use behaviors: Predictive disparities in parents’ versus adolescents’ perceptions of the parenting environment. Journal of Clinical Child and Adolescent Psychology. 2009;38:232–244. doi: 10.1080/15374410802698404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laursen B, Coy KC, Collins WA. Reconsidering changes in parent-child conflict across adolescence: A meta-analysis. Child Development. 1998;69:817–832. [PMC free article] [PubMed] [Google Scholar]
- Letourneau N, Drummond J, Fleming D, Kysela G, McDonald L, Stewart M. Supporting parents: Can intervention improve parent-child relationships? Journal of Family Nursing. 2001;7:159–187. [Google Scholar]
- Mannuzza S, Klein RG. Adolescent and adult outcomes in attention-deficit/hyperactivity disorder. In: Quay HC, Hogan AE, editors. Handbook of disruptive behavior disorders. New York: Kluwer Academic/Plenum; 1999. pp. 279–294. [Google Scholar]
- Mannuzza S, Klein RG, Bonagura N, Malloy P, Giampino TL, Addalli KA. Hyperactive boys almost grown up. V. Replication of psychiatric status. Archives of General Psychiatry. 1991;48:77–83. doi: 10.1001/archpsyc.1991.01810250079012. [DOI] [PubMed] [Google Scholar]
- Marshal MP, Molina B, Pelham WE. Deviant peer affiliation as a risk factor for substance use in adolescents with childhood ADHD. Psychology of Addictive Behaviors. 2003;17:293–302. doi: 10.1037/0893-164X.17.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Molina BSG, Pelham WE. Antisocial alcoholism in mothers and fathers of children with ADHD. Journal of Attention Disorders (under review) [Google Scholar]
- McQueen A, Getz JG, Bray JH. Acculturation, substance use, and deviant behavior: Examining separation and family conflict as mediators. Child Development. 2003;74:1737–1750. doi: 10.1046/j.1467-8624.2003.00635.x. [DOI] [PubMed] [Google Scholar]
- Minde K, Eakin L, Hechtman L, Ochs E, Bouffard R, Greenfield B, Looper K. The psychosocial functioning of children and spouses of adults with ADHD. Journal of Child Psychology and Psychiatry. 2003;44:637–646. doi: 10.1111/1469-7610.00150. [DOI] [PubMed] [Google Scholar]
- Molina BSG. Delinquency and substance use in ADHD: Adolescent and young adult outcomes in developmental context. In: Evans SW, Hoza B, editors. Attention Deficit Hyperactivity Disorder: State of the Science & Best Practices. Vol. 2. New York: Civic Research Institute; (in press) [Google Scholar]
- Molina BSG, Donovan JE, Belendiuk KA. Familial loading for alcoholism and offspring behavior: Mediating and moderating influences. Alcoholism: Clinical and Experimental Research. 2010;34:1972–1984. doi: 10.1111/j.1530-0277.2010.01287.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Flory K, Hinshaw SP, Greiner AR, Arnold LE, Swanson JM, Hechtman L, Jensen PS, Vitiello B, Hoza B, Pelham WE, Elliott GR, Wells KC, Abikoff HB, Gibbons RD, Marcus S, Conners CK, Epstein JN, Greenhill LL, March JS, Newcorn JH, Severe JB, Wigal T. Delinquent behavior and emerging substance use in the MTA at 36 months: Prevalence, course, and treatment effects. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1028–1040. doi: 10.1097/chi.0b013e3180686d96. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, Epstein JN, Hoza B, Hechtman L, Abikoff HB, Elliott GR, Greenhill LL, Newcorn JH, Wells KC, Wigal T, Gibbons RD, Hur K, Houck PR MTA Cooperative Group. The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48:484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Marshal MP, Pelham WE, Wirth RJ. Coping skills and parent support mediate the association between childhood ADHD and adolescent cigarette use. Journal of Pediatric Psychology. 2005;30:345–357. doi: 10.1093/jpepsy/jsi029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE. Childhood predictors of substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology. 2003;112:497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- Mrug S, Gaines J, Wei Su, Windle M. School-level substance use: Effects on early adolescents’ alcohol, tobacco, and marijuana use. Journal of Studies on Alcohol and Drugs. 2010;71:488–495. doi: 10.15288/jsad.2010.71.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray C, Johnston C. Parenting in mothers with and without Attention-Deficit/Hyperactivity Disorder. Journal of Abnormal Psychology. 2006;115:52–61. doi: 10.1037/0021-843X.115.1.52. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus: Statistical analysis with latent variables: User’s guide. Los Angeles, CA: Muthen & Muthen; 2005. [Google Scholar]
- Nash SG, McQueen A, Bray JH. Pathways to adolescent alcohol use: Family environment, peer influence, and parental expectations. Journal of Adolescent Health. 2005;37:19–28. doi: 10.1016/j.jadohealth.2004.06.004. [DOI] [PubMed] [Google Scholar]
- National Household Survey on Drug Abuse (NHSDA) OMB No. 0930–0110. Washington, DC: U.S. Department of Health and Human Services, Public Health Service, and Alcohol, Drug Abuse and Mental Health Administration. National Institute on Drug Abuse; 1992. [Google Scholar]
- Nigg JT, Hinshaw SP. Parent personality traits and psychopathology associated with antisocial behaviors in childhood attention-deficit hyperactivity disorder. The Journal of Child Psychology and Psychiatry. 2003;39:145–159. [PubMed] [Google Scholar]
- Owens JS, Hoza B. The role of inattention and hyperactivity/impulsivity in the positive illusory bias. Journal of Consulting and Clinical Psychology. 2003;71:680–691. doi: 10.1037/0022-006x.71.4.680. [DOI] [PubMed] [Google Scholar]
- Patterson GR. Performance models for antisocial boys. American Psychologist. 1986;41:432–444. doi: 10.1037//0003-066x.41.4.432. [DOI] [PubMed] [Google Scholar]
- Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44:329–335. doi: 10.1037//0003-066x.44.2.329. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Fabiano GA. Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology. 2008;37:184–214. doi: 10.1080/15374410701818681. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Lang AR, Atkeson B, Murphy DA, Gnagy EM, Greiner AR, Vodde-Hamilton M, Greenslade KE. Effects of deviant child behavior on parental distress and alcohol consumption in laboratory interactions. Journal of Abnormal Child Psychology. 1997;25:413–424. doi: 10.1023/a:1025789108958. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Lang AR, Atkeson B, Murphy DA, Gnagy EM, Greiner AR, Vodde-Hamilton M, Greenslade KE. Effects of deviant child behavior on parental alcohol consumption: Stress-induced drinking in parents of ADHD children. American Journal of Addictions. 1998;7:103–114. [PubMed] [Google Scholar]
- Robin AL, Foster SL. Negotiating parent-adolescent conflict: A behavioral-family systems approach. NY: Guilford Press; 1989. [Google Scholar]
- Rutter M. Implications of resilience concepts for scientific understanding. Annals of the New York Academy of Sciences. 2006;1094:1–12. doi: 10.1196/annals.1376.002. [DOI] [PubMed] [Google Scholar]
- Satterfield JH, Hoppe CM, Schell AM. A prospective study of delinquency in 110 adolescent boys with attention deficit disorder and 88 normal adolescent boys. The American Journal of Psychiatry. 1982;139:795–798. doi: 10.1176/ajp.139.6.795. [DOI] [PubMed] [Google Scholar]
- Schaefer ES. Children’s reports of parental behavior: An inventory. Child Development. 1965;36:413–424. [PubMed] [Google Scholar]
- Schmitt MJ, Steyer R. A latent state-trait model (not only) for social desirability. Personality and Inidividual Differences. 1993;14:519–529. [Google Scholar]
- Schwarz JC, Barton-Henry ML, Pruzinsky T. Assessing child-rearing behaviors: A comparison of ratings made by mother, father, child, and sibling on the CRPBI. Child Development. 1985;56:462–479. [PubMed] [Google Scholar]
- Sessa FM, Avenevoli S, Steinberg L, Morris AS. Correspondence among informants on parenting: Preschool children, mothers, and observers. Journal of Family Psychology. 2001;15:53–68. doi: 10.1037//0893-3200.15.1.53. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Dishion TJ, Supplee L, Gardner F, Arnds K. Randomized trial of a family-centered approach to the prevention of early conduct problems: 2-year effects of the family check-up in early childhood. Journal of Consulting and Clinical Psychology. 2006;74:1–9. doi: 10.1037/0022-006X.74.1.1. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Biswas A, MacLean MG, Babinski DE, Karch KM. The delinquency outcomes of boys with ADHD with and without comorbidity. Journal of Abnormal Child Psychology. doi: 10.1007/s10802-010-9443-9. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BH, Pelham WE, Gnagy E, Molina B, Evans S. The reliability, validity, and unique contributions of self-report by adolescents receiving treatment for attention-deficit/hyperactivity disorder. Journal of Consulting and Clinical Psychology. 2000;68:489–499. doi: 10.1037/0022-006X.68.3.489. [DOI] [PubMed] [Google Scholar]
- Stattin H, Kerr M. Parental monitoring: A reinterpretation. Child Development. 2000;71:1072–1085. doi: 10.1111/1467-8624.00210. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Autonomy, conflict, and harmony in the family relationship. In: Feldman S, Elliot G, editors. At the threshold: The developing adolescent. Cambridge, MA: Harvard University Press; 1990. pp. 255–276. [Google Scholar]
- Steinberg L. We know some things: Parent-adolescent relationships in retrospect and prospect. Journal of Research on Adolescence. 2001;11:1–19. [Google Scholar]
- Steinberg L, Lamborn SD, Darling N, Mounts NS, Dornbusch SM. Overtime changes in adjustment and competence among adolescents from authoritative, authoritarian, indulgent, and neglectful families. Child Development. 1994;65:754–770. doi: 10.1111/j.1467-8624.1994.tb00781.x. [DOI] [PubMed] [Google Scholar]
- Stewart MA, Susan deBlois C, Cummings C. Psychiatric disorder in the parents of hyperactive boys and those with conduct disorder. The Journal of Child Psychology and Psychiatry. 2006;21:283292. doi: 10.1111/j.1469-7610.1980.tb00033.x. [DOI] [PubMed] [Google Scholar]
- Stice E, Barrera M. A longitudinal examination of the reciprocal relations between perceived parenting and adolescents’ substance use and externalizing behaviors. Developmental Psychology. 1995;31:322–334. [Google Scholar]
- Stice E, Barrera M, Chassin L. Relation of parental support and control adolescents’ externalizing symptomatology and substance use: A longitudinal examination of curvilinear effects. Journal of Abnormal Child Psychology. 1993;21:609–629. doi: 10.1007/BF00916446. [DOI] [PubMed] [Google Scholar]
- Stormshak EA, Bierman KL, McMahon RJ, Lengua LJ. Parenting practices and child disruptive behavior problems in early elementary school. Journal of Clinical Child Psychology. 2000;29:17–29. doi: 10.1207/S15374424jccp2901_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilson EC, McBride CM, Lipkus IM, Catalano RF. Testing the interaction between parent-child relationship factors and parent smoking to predict youth smoking. Journal of Adolescent Health. 2004;35:182–189. doi: 10.1016/j.jadohealth.2003.09.014. [DOI] [PubMed] [Google Scholar]
- van der Vorst H, Engels RCME, Meeus W, Dekovic M, Vermulst A. Parental attachment, parental control, and early development of alcohol use: A longitudinal study. Psychology of Addictive Behaviors. 2006;20:107–116. doi: 10.1037/0893-164X.20.2.107. [DOI] [PubMed] [Google Scholar]
- van der Vorst H, Vermulst A, Meeus W, Deković M, Engels RCME. Identification and prediction of drinking trajectories in early and mid-adolescence. Journal of Clinical Child & Adolescent Psychology. 2009;38:329–341. doi: 10.1080/15374410902851648. [DOI] [PubMed] [Google Scholar]
- van der Zwaluw CS, Scholte RHJ, Vermulst AA, Buitelaar JK, Verkes RJ, Engels RCME. Parental problem drinking, parenting, and adolescent alcohol use. Journal of Behavioral Medicine. 2008;31:189–200. doi: 10.1007/s10865-007-9146-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahler RG, Dumas JE. Maintenance factors in coercive mother-child interactions: The compliance and predictability hypothesis. Journal of Applied Behavior Analysis. 1986;19:13–22. doi: 10.1901/jaba.1986.19-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waizenhofer RN, Buchanan CM, Jackson-Newsom J. Mothers’ and fathers’ knowledge of adolescents’ daily activities: Its sources and its links with adolescent adjustment. Journal of Family Psychology. 2004;18:348–360. doi: 10.1037/0893-3200.18.2.348. [DOI] [PubMed] [Google Scholar]
- Windle M, Brener N, Cuccaro P, Dittus P, Kanouse DE, Murray N, Wallander J, Schuster MA. Parenting predictors of early-adolescents’ health behaviors: Simultaneous group comparisons across sex and ethnic groups. Journal of Youth and Adolescence. 2010;39:594–606. doi: 10.1007/s10964-009-9414-z. [DOI] [PubMed] [Google Scholar]
- Winters KC. Treating adolescents with substance use disorders: An overview of practice issues and treatment outcome. Substance Abuse. 1999;20:203–225. doi: 10.1080/08897079909511407. [DOI] [PubMed] [Google Scholar]
- Wells KC, Epstein JN, Hinshaw SP, Conners CK, Klaric J, Abikoff HB, Abramowitz A, Arnold LE, Elliott G, Greenhill LL, Hechtman L, Hoza B, Jensen PS, March JS, Pelham W, Pfiffner L, Severe J, Swanson JM, Vitiello B, Wigal T. Parenting and family stress treatment outcomes in attention deficit hyperactivity disorder (adhd): An empirical analysis in the MTA study. Journal of Abnormal Child Psychology. 2000;28:543–553. doi: 10.1023/a:1005131131159. [DOI] [PubMed] [Google Scholar]
- Wells KC, Pelham WE, Kotkin RA, Hoza B, Abikoff HB, Abramowitz A, Arnold LE, Cantwell DP, Conners CK, Carmen RD, Elliot G, Greenhill LL, Hechtman L, Hibbs E, Hinshaw SP, Jensen PS, March J, Swanson J, Schiller E. Psychosocial treatment strategies in the MTA study: Rationale, methods, and critical issues in design and implementation. Journal of Abnormal Child Psychology. 2000;28:483–506. doi: 10.1023/a:1005174913412. [DOI] [PubMed] [Google Scholar]
- Wender P. Attention deficit hyperactivity disorder in adults. New York: Oxford University Press; 1995. [Google Scholar]
- Wymbs BT, Pelham WE, Molina BSG, Gnagy EM. Mother and adolescent reports of interparental discord among parents of adolescents with and without attention-deficit/hyperactivity disorder. Journal of Emotional and Behavioral Disorders. 2008;16:29–41. doi: 10.1177/1063426607310849. [DOI] [PMC free article] [PubMed] [Google Scholar]