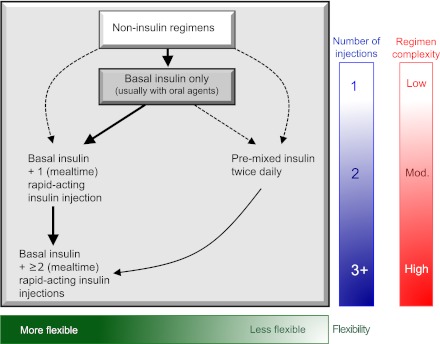
Figure 3.
Sequential insulin strategies in type 2 diabetes. Basal insulin alone is usually the optimal initial regimen, beginning at 0.1–0.2 units/kg body weight, depending on the degree of hyperglycemia. It is usually prescribed in conjunction with one to two noninsulin agents. In patients willing to take more than one injection and who have higher HbA1c levels (≥9.0%), twice-daily premixed insulin or a more advanced basal plus mealtime insulin regimen could also be considered (curved dashed arrow lines). When basal insulin has been titrated to an acceptable fasting glucose but HbA1c remains above target, consider proceeding to basal plus mealtime insulin, consisting of one to three injections of rapid-acting analogs (see text for details). A less studied alternative—progression from basal insulin to a twice-daily premixed insulin—could be also considered (straight dashed arrow line); if this is unsuccessful, move to basal plus mealtime insulin. The figure describes the number of injections required at each stage, together with the relative complexity and flexibility. Once a strategy is initiated, titration of the insulin dose is important, with dose adjustments made based on the prevailing glucose levels as reported by the patient. Noninsulin agents may be continued, although insulin secretagogues (sulfonylureas, meglitinides) are typically stopped once more complex regimens beyond basal insulin are utilized. Comprehensive education regarding self-monitoring of blood glucose, diet, exercise, and the avoidance of, and response to, hypoglycemia are critical in any patient on insulin therapy. Mod., moderate.