Abstract
AIM
To report the effectiveness and safety of primary 23-Gauge (G) vitreoretinal surgery for rhegmatogenous retinal detachment (RRD).
METHODS
In this retrospective study, 49 eyes of 49 consecutive patients who underwent primary 23-G transconjunctival sutureless vitrectomy (TSV) for RRD between January 2007 and July 2009 at our institution were evaluated.
RESULTS
Mean follow-up time was 8.9±7.7 months (1-28 months). Retinal reattachment was achieved with a single operation in 47(95.9%) of 49 eyes. In two eyes (4.1%), retinal redetachment due to new breaks was successfully treated with reoperation using the 23-G TSV system. Mean logMAR visual acuity was 2.01±0.47 preoperatively and 1.3±0.5 postoperatively (P<0.001, Paired t-test). Mean preoperative intraocular pressure (IOP) was 14.1±2.8mmHg. Mean postoperative IOP was 12.3±3.6mmHg at 1 day, 13.1±2.1mmHg at 1 week, 14.3±2.2mmHg at 1 month. Iatrogenic peripheral retinal break was observed in 1 eye (2.0%) intraoperatively. No sutures were required to close the scleral or conjunctival openings, and no eyes required convertion of surgery to 20-G vitrectomy.
CONCLUSION
Primary 23-G TSV system was observed to be effective and safe in the treatment of RRD.
Keywords: pars plana vitrectomy, retinal detachment, rhegmatogenous retinal detachment, transconjunctival sutureless vitrectomy, vitreoretinal surgery, 23-gauge vitrectomy
INTRODUCTION
Primary pars plana vitrectomy (PPV), pneumatic retinopexy and scleral buckling are the treatment options in rhegmatogenous retinal detachment (RRD). The choice of surgical procedure is dependent on the location and number of breaks, quadrant of retinal detachment and presence of proliferative vitreoretinopathy[1]-[7].
Machemer et al[8] first performed PPV in 1971 and standard three-port PPV was developed soon after this innovation[9]. Fujii et al[10],[11] introduced the 25-G transconjunctival sutureless vitrectomy (TSV) in 2002 to minimize surgically induced trauma. Recently, Eckardt[12] developed 23-G TSV using an obliquely entering trocar cannular system and this evolution in vitreoretinal surgery has become increasingly popular in the last few years. Primary 23-Gauge TSV for rhegmatogenous retinal detachment was previously reported in only small number of patients[13],[14]. The purpose of this study was to report the effectiveness and safety of the primary 23-G TSV in the treatment of RRD.
MATERIALS AND METHODS
Materials
In this retrospective non-control study, we evaluated 49 eyes of 49 consecutive patients who underwent primary 23-G TSV for RRD between January 2007 and July 2009 at our institution. Patients with previous retinal detachment surgery were excluded. In our institution, we do not perform scleral buckling surgery in recent years. If the eye is not suitable for pneumatic retinopexy, we perform primary vitrectomy.The indications of primary 23-G TSV for RRD were listed in Table 1. Vitreous hemorrhage in 5 eyes (10.2%), choroidal detachment in 4 eyes (8.2%) and macular hole in 1 eye (2.0%) were the concurrent conditions with RRD.
Table 1. Indications of primary 23-G TSV for RRD.
| Indications | n (%) |
| Pseudophakic retinal detachment | 21(42.8%) |
| Phakic retinal detachment not suitable for pneumatic retinopexy | 15(30.6%) |
| Retinal detachment with giant tear | 3(6.1%) |
| Aphakic retinal detachment | 2(4.1%) |
| Grade C or worse preoperative PVR | 8(16.3%) |
Main outcome measures were anatomical and functional outcomes as well as intraoperative and postoperative complications. Visual acuity improvement was defined as improvement by 2 or more lines. Stable visual acuity was defined as no change or 1 line change in visual acuity. Visual acuity impairment was defined as impairment by 2 or more lines.
The possible merits and risks of the treatment were explained to the patient and an informed consent was obtained in accordance with the Helsinki Declaration prior to inclusion in the study. Institutional Review Board approval was not required for this study.
All patients received a best-corrected Snellen visual acuity measurement, anterior segment examination, intraocular pressure (IOP) measurement with Goldmann applanation tonometry and biomicroscopic evaluation with both fundus non-contact and contact lenses. All IOPs were taken at 08.00-10.00 am. B-scan ultrasonography was performed in all eyes in which visualization of the fundus was not attained. Best-corrected Snellen visual acuities were converted into logMAR (logarithm of the minimum angle of resolution) units. Inferior breaks were located in the inferior 4 clock hours (4-8 o'clock [inclusive]).
Methods
Surgical technique
All of the operations were performed by the same surgeon (A.Y.) under sub-Tenon anesthesia. The 2-step 23-G vitrectomy system (Dutch Ophthalmic Research Center, Zuidland, The Netherlands) was used in all cases. The microcannulas were inserted transconjunctivally with the help of the insertion trocars in the inferotemporal, superotemporal, and superonasal quadrants, 3.5 mm posterior to the limbus in pseudophakic and aphakic eyes, and 4 mm posterior to the limbus in phakic eyes. A special pressure plate was used to laterally displace the conjunctiva in the three sites where the trocars were placed and to hold the conjunctiva against the sclera. A 23-G MVR was inserted tangentially at an angle of approximately 30° paralel to the limbus. The infusion cannula was placed in the inferotemporal quadrant, and plugs were used to temporarily close the other entry sites. High speed vitrectomy probe (2267.NMD06) of surgical system (DORC Associate 2500, Zuidland, The Netherlands) with a cutting rate of 1500-2500 cuts per minute and a vacuum level of 400 mmHg to 500 mmHg was used during PPV. The balanced salt solution (BSS) bottle height was set at 50 cm. Retinal reattachment with perfluorocarbon liquid (PFCL, Okta-line, Bausch&Lomb Surgical, Claremont, California, USA), endolaser photocoagulation (around the tear(s) and 360° peripheral retina), air-PFCL exchange and internal tamponade were performed in all cases. The internal tamponades that were used in the treatment of RRD are silicone oil (Siluron 1000, Fluoron, GmbH, Ulm, Germany), heavy silicone oil (Densiron 68 LV, Fluoron, GmbH, Ulm, Germany), SF6 gas (GOT SF6 multi, Alchimia, Ponte S.Nicolo, Italy), and C3F8 gas (GOT C3F8 multi, Alchimia, Ponte S.Nicolo, Italy.)(Table 2). Silicone oil was used as internal tamponade for patients who will fly, who will not be able to do the head position after gas injection or who need to have early visual rehabilitation. Epiretinal membrane peeling was performed when required. Insertion trocars were removed slightly from the eye at the end of the operation. A gentle massage to the sclerotomy site with a muscle hook was performed to avoid leakage. The conjunctiva overlying the sclerotomy was slightly displaced to disrupt the alignment between both entry sites, and an antibiotic and corticosteroid combination was injected into the subconjunctival space.
Table 2. Internal tamponades used in treatment of RRD.
| Internal tamponade | n (%) |
| Silicone oil | 33 (67.3%) |
| Heavy silicone oil | 2 (4.1%) |
| Sulfur hexafluoride (SF6) gas | 12 (24.5%) |
| Perfluoropropane (C3F8) gas | 2 (4.1%) |
Silicone oil was removed within 2 months after the surgery in all eyes that received silicone oil injection. Single operation success was defined as complete retinal reattachment after silicone oil removal and after complete resorption of the gas following primary 23-G TSV surgery for RRD. Postoperative 1st day, 1st week, 1st month, 3rd month and 3 months intervals thereafter were the time points for examination.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for Social Sciences software (SPSS for Windows, Version 17.0, SPSS Inc., Chicago, IL.). Kolmogorov-Smirnov test was used in testing whether the variables have depicted a normal distribution or not. The repeated one-way ANOVA and the paired samples t-test were used for statistical analysis. P<0.05 was defined as statistically significant.
RESULTS
Mean follow-up time was 8.9±7.7 months (range, 1 to 28 months). Preoperative characteristics of patients: mean age, gender, visual acuity, lens status and duration of retinal detachment were listed in Table 3. Most of the retinal breaks were single and located in superior quadrants. The macula was detached in most of the eyes (Table 4).
Table 3. Preoperative characteristics of patients underwent primary 23-G TSV for RRD.
| Characteristics | |
| Age (y)* | 55.4±16.8 |
| Sex, n(%) | |
| Female | 28(57.2%) |
| Male | 21(42.8%) |
| Eye, n(%) | |
| Right | 29(59.2%) |
| Left | 20(40.8%) |
| Preoperative logMAR visual acuity* | 2.01±0.47 |
| Mean follow-up time (m)* | 8.9±7.7 |
| Lens status, n(%) | |
| Phakic | 26(53.1%) |
| Pseudophakic | 21(42.8%) |
| Aphakic | 2(4.1%) |
| Duration of retinal detachment (d)* | 49±85(4-365) |
*Mean ± SD; Y = year; m = month; d = day
Table 4. Preoperative characteristics of RRD and retinal break.
| Characteristics | n (%) |
| Location of breaks | |
| Superior | 27 (55.1%) |
| Inferior | 10 (20.4%) |
| Superior and Inferior* | 12 (24.5%) |
| Number of retinal breaks | |
| One | 28 (57. 2%) |
| Multiple | 18 (36.7%) |
| Giant | 3 (6.1%) |
| Quadrant of retinal detachment | |
| 1 quadrant | - |
| 2 quadrant | 14 (28.6%) |
| 3 quadrant | 14 (28.6%) |
| Total | 21 (42.8%) |
| Macular detachment | |
| Macula off | 40 (81.6%) |
| Macula on | 9 (18.4%) |
* Patients with breaks in both superior and inferior quadrants
Single operation success was achieved in 47 (95.9%) of 49 eyes. Retinal redetachment due to a new break was observed postoperative one week in 1 eye and postoperative three weeks in the other eye. These eyes were successfully treated with reoperation using the 23-G TSV system.
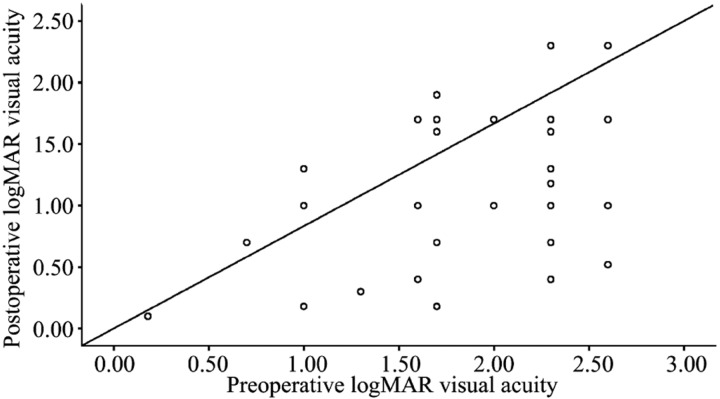
Mean best-corrected logMAR visual acuity ± SD was 2.01±0.47 (counting fingers equivalent) preoperatively and 1.3±0.5 (20/400 equivalent) postoperatively (P<0.001, Paired t-test) (Figure 1). Postoperative visual acuity improved in 41 eyes (83.7%), was stable in 7 eyes (14.3%), and impaired in 1 eye (2.0%). Postoperative visual acuity was 20/40 or better in 4 eyes (8.2%).
Figure 1. Preoperative and postoperative logMAR visual acuities in 49 eyes which underwent 23-G PPV for RRD. Postoperative visual acuity improved in 41 eyes, was stable in 7 eyes, and impaired in 1 eye.
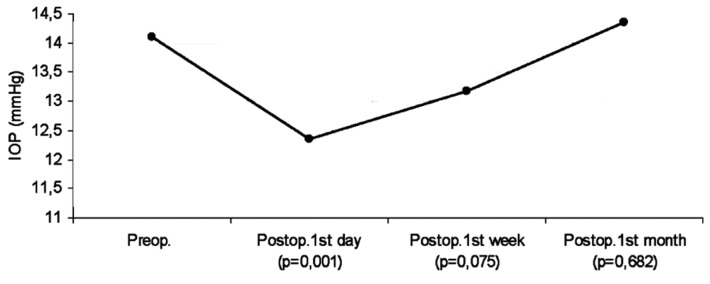
Mean preoperative IOP was 14.1±2.8mmHg. Mean postoperative IOP was 12.3±3.6mmHg at 1 day, 13.1±2.1mmHg at 1 week and 14.3±2.2mmHg at 1 month (Figure 2). As there were differences between repeated measurements (P<0.05, one-way ANOVA test), pairwise comparisons were performed and the results of analysis of IOP changes were given in Table 5. Postoperative hypotony (<8mmHg), which was observed in 1 eye (2.0%) normalized spontaneously within the first postoperative week.
Figure 2. IOP changes after 23-G TSV.
Table 5. Analysis of IOP changes.
| IOP | P* |
| Preoperative- postoperative 1st day | 0.001 |
| Preoperative- postoperative 1st week | 0.075 |
| Preoperative- postoperative 1st month | 0.682 |
| Postoperative 1st day- postoperative 1st week | 0.045 |
| Postoperative 1st day- postoperative 1st month | 0.000 |
| Postoperative 1st week- postoperative 1st month | 0.002 |
* Paired samples t-test, P<0.05 is statistically significant
No major intraoperative complication was encountered except for iatrogenic peripheral retinal break in 1 eye (2.0%). PPV, epiretinal membrane peeling, endolaser photocoagulation, air-PFCL exchange and internal tamponade injection were performed easily. Postoperative complications were cataract formation or progression, macular pucker, silicone oil droplets in anterior chamber, glaucoma controlled by topical medication and transient hypotony (Table 6). Cataract formation or progression was observed in 10 eyes. All of them received cataract surgery during the follow-up period. Subconjunctival leak of silicone oil was not seen in any cases. Leakage, extension, dehiscence and hemorrhage, or vitreous or retinal incarceration at the external side of the sclerotomies was not observed in any eye. The internal side of the sclerotomies was not evaluated by ultrasound biomicroscopy. No sutures were required to close the scleral or conjunctival openings and no eyes required conversion of surgery to 20-G PPV.
Table 6. Intraoperative and postoperative complications of primary 23-G TSV for RRD.
| Complications | n (%) |
| Intraoperative | |
| Iatrogenic retinal tear | 1(2.0%) |
| Postoperative | |
| Cataract formation or progression | 10(38.5%) |
| Redetachment | 2(4.1%) |
| Macular pucker | 3(6.1%) |
| Silicone oil droplets in anterior chamber | 5(10.2%) |
| Glaucoma controlled by topical medication | 2(4.1%) |
| Transient hypotony | 1(2.0%) |
DISCUSSION
In a previous prospective study, in which primary 23-G PPV with intraocular gas tamponade was performed in 24 eyes with RRD, primary and final anatomical success rate was 91.7% and 100%, respectively. Visual acuity improved in 82%, was stable in 9%, and impaired in 9% of eyes[13]. In another study, in which primary 23-G PPV with silicone oil tamponade was performed in 10 eyes with complex RRD, primary success rate was 90% and visual acuity improved in 90% of eyes[14]. Similarly, primary anatomical success rate was 95.9% and final anatomical success rate was 100% in our study. Visual acuity improved in 83.7%, was stable in 14.3%, and impaired in 2% of eyes. Visual acuity was 20/40 or better in 8.2% of eyes after surgery.
The primary and final anatomical success rates of primary PPV in RRD have been reported as 62.6-98.3%[1],[7] and 93-100%[2],[3] with 20-G, 72.2-92.9%[15],[16] and 91.6-100%[17],[18] with 25-G, respectively. Most of these studies did not use silicone oil as the primary tamponade. In our study, silicone oil was used as an internal tamponade in 67.3% of eyes.
The potential advantages of 20-G PPV without scleral buckling over conventional scleral buckling are expected to be the advantages of TSV. These are less operation time, accurate diagnosis of breaks, controlled drainage of subretinal fluid and no postoperative axial length changes. There are several advantages of TSV over 20-G PPV including reduced postoperative inflammatory reaction, absence of suture related irritation and local inflammatory reaction at the sclerotomy sites, reduced postoperative conjunctival injection and pain, improved patient comfort, faster postoperative recovery, reduced surgically induced trauma, insignificant corneal surface and astigmatic changes, and less conjunctival scaring[11],[19]-[21]. Furthermore, there is no limbal stem cell damage due to conjunctival dissection, so it may be advantageous in eyes with corneal or conjunctival diseases such as dry eye.
Therefore, if a primary PPV is appropriate in the management of retinal deteachment, it may be logical to perform it with a TSV system.
In our study no major intraoperative complication was encountered except for peripheral retinal break that was observed in 1 eye (2.0%). Postoperative complications were cataract formation or progression (38.5%), macular pucker (6.1%), silicone oil droplets in anterior chamber (10.2%), glaucoma controlled by topical medication (4.1%) and transient hypotony (2.0%). Intraoperative retinal break, scleral suture requirement, hypotony, cataract, macular pucker, cystoid macular edema, vitreous hemorrhage, retinal redetachment, choroidal detachment, endophthalmitis and glaucoma have been previously reported in several studies with 20-G PPV, 23 and 25-G TSV[1],[3],[7],[13]-[15],[18]-[51].
Short follow-up time and lack of comparison of eyes treated with 20-G PPV and 25-G TSV were the primary limitations of this study. Our study design was retrospective and postoperative evaluation could not be performed at predetermined time points. Therefore, we could not evaluate the functional outcomes and anatomical results at each follow-up.
In conclusion, 23-G TSV was observed to be safe and effective in the treatment of RRD with or without severe PVR in 49 eyes. Further studies comparing the 23-G TSV system to standard 20-G PPV, 25-G TSV and scleral buckling for RRD with a long follow-up time are required to make a more reliable conclusion.
REFERENCES
- 1.Ahmadieh H, Moradian S, Faghihi H, Parvaresh MM, Ghanbari H, Mehryar M, Heidari E, Behboudi H, Banaee T, Golestan B. Anatomic and visual outcomes of scleral buckling versus primary vitrectomy in pseudophakic and aphakic retinal detachment: six month follow-up results of a single operation-report no. 1. Ophthalmology. 2005;112(8):1421–1429. doi: 10.1016/j.ophtha.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 2.Escoffery RF, Olk RJ, Grand MG, Boniuk I. Vitrectomy without scleral buckling for primary rhegmatogenous retinal detachment. Am J Ophthalmol. 1985;99(3):275–281. doi: 10.1016/0002-9394(85)90356-3. [DOI] [PubMed] [Google Scholar]
- 3.Sharma YR, Karunanithi S, Azad RV, Vohra R, Pal N, Singh DV, Chandra P. Functional and anatomic outcome of scleral buckling versus primary vitrectomy in pseudophakic retinal detachment. Acta Ophthalmol Scand. 2005;83(3):293–297. doi: 10.1111/j.1600-0420.2005.00461.x. [DOI] [PubMed] [Google Scholar]
- 4.Oshima Y, Emi K, Motokura M, Yamanishi S. Survey of surgical indications and results of primary pars plana vitrectomy for rhegmatogenous retinal detachments. Jpn J Ophthalmol. 1999;43(2):120–126. doi: 10.1016/s0021-5155(98)00075-6. [DOI] [PubMed] [Google Scholar]
- 5.Tornambe PE, Hilton GF, the Retinal Detachment StudyGroup Pneumatic retinopexy: a multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology. 1989;96(6):772–784. doi: 10.1016/s0161-6420(89)32820-x. [DOI] [PubMed] [Google Scholar]
- 6.Tornambe PE, Hilton GF, Kelly NF, Salzano TC, Wells JW, Wendel RT. Expanded indications for pneumatic retinopexy. Ophthalmology. 1988;95(5):597–600. doi: 10.1016/s0161-6420(88)33135-0. [DOI] [PubMed] [Google Scholar]
- 7.Martinez-Castillo V, Zapata MA, Boixadera A, Fonollosa A, García-Arumí J. Pars plana vitrectomy, laser retinopexy, and aqueous tamponade for pseudophakic rhegmatogenous retinal detachment. Ophthalmology. 2007;114(2):297–302. doi: 10.1016/j.ophtha.2006.07.037. [DOI] [PubMed] [Google Scholar]
- 8.Machemer R, Buettner H, Norton EW, Parel JM. Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol. 1971;75(4):813–820. [PubMed] [Google Scholar]
- 9.O'Malley C, Heintz RM., Sr Vitrectomy with an alternative instrument system. Ann Ophthalmol 1975; 7(4) 1975;7(4):585–588, 591-594. [PubMed] [Google Scholar]
- 10.Fujii GY, De Juan E, Jr, Humayun MS, Pieramici DJ, Chang TS, Awh C, Ng E, Barnes A, Wu SL, Sommerville DN. A new 25-Gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109(10):1807–1812. doi: 10.1016/s0161-6420(02)01179-x. [DOI] [PubMed] [Google Scholar]
- 11.Fujii GY, De Juan E, Jr, Humayun MS, Chang TS, Pieramici DJ, Barnes A, Kent D. Initial experience using the transconjunctival sutureless vitrectomy system for vitreoretinal surgery. Ophthalmology. 2002;109(10):1814–1820. doi: 10.1016/s0161-6420(02)01119-3. [DOI] [PubMed] [Google Scholar]
- 12.Eckardt C. Transconjunctival suturless 23-gauge vitrectomy. Retina. 2005;25(2):208–211. doi: 10.1097/00006982-200502000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Tsang CW, Cheung BT, Lam RF, Lee GK, Yuen CY, Lai TY, Lam DS. Primary 23-gauge transconjunctival sutureless vitrectomy for rhegmatogenous retinal detachment. Retina. 2008;28(8):1075–1081. doi: 10.1097/IAE.0b013e31817b98ba. [DOI] [PubMed] [Google Scholar]
- 14.Oliveira LB, Reis PA. Silicone oil tamponade in 23-gauge transconjunctival sutureless vitrectomy. Retina. 2007;27(8):1054–1058. doi: 10.1097/IAE.0b013e318113235e. [DOI] [PubMed] [Google Scholar]
- 15.Shah CP, Ho AC, Regillo CD, Fineman MS, Vander JF, Brown GC. Short-term outcomes of 25-gauge vitrectomy with silicone oil for repair of complicated retinal detachment. Retina. 2008;28(5):723–728. doi: 10.1097/IAE.0b013e318166976d. [DOI] [PubMed] [Google Scholar]
- 16.Miller DM, Riemann CD, Foster RE, Petersen MR. Primary repair of retinal detachment with 25-gauge pars plana vitrectomy. Retina. 2008;28(7):931–936. doi: 10.1097/IAE.0b013e31816b313a. [DOI] [PubMed] [Google Scholar]
- 17.Kapran Z, Acar N, Altan T, Unver YB, Yurttaser S. 25-Gauge sutureless vitrectomy with oblique sclerotomies for the management of retinal detachment in pseudophakic and phakic eyes. Eur J Ophthalmol. 2009;19(5):853–860. doi: 10.1177/112067210901900527. [DOI] [PubMed] [Google Scholar]
- 18.Von Fricken MA, Kunjukunju N, Weber C, Ko G. 25-Gauge sutureless vitrectomy versus 20-gauge vitrectomy for the repair of primary rhegmatogenous retinal detachment. Retina. 2009;29(4):444–450. doi: 10.1097/IAE.0b013e318196b19c. [DOI] [PubMed] [Google Scholar]
- 19.Wimpissinger B, Kellner L, Brannath W, Krepler K, Stolba U, Mihalics C, Binder S. 23-gauge versus 20-gauge system for pars plana vitrectomy: a prospective randomised clinical trial. Br J Ophthalmol. 2008;92(11):1483–1487. doi: 10.1136/bjo.2008.140509. [DOI] [PubMed] [Google Scholar]
- 20.Yanyali A, Celik E, Horozoglu F, Nohutcu AF. Corneal topographic changes after transconjunctival (25-gauge) sutureless vitrectomy. Am J Ophthalmol. 2005;140(5):939–941. doi: 10.1016/j.ajo.2005.05.042. [DOI] [PubMed] [Google Scholar]
- 21.Fine HF, Iranmanesh R, Iturralde D, Spaide RF. Outcomes of 77 consecutive cases of 23-gauge transconjunctival vitrectomy surgery for posterior segment disease. Ophthalmology. 2007;114(6):1197–1200. doi: 10.1016/j.ophtha.2007.02.020. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto T, Hitani K, Tsukahara I, Yamamoto S, Kawasaki R, Yamashita H, Takeuchi S. Early postoperative retinal thickness changes and complications after vitrectomy for diabetic macular edema. Am J Ophthalmol. 2003;135(1):14–19. doi: 10.1016/s0002-9394(02)01819-6. [DOI] [PubMed] [Google Scholar]
- 23.Brazitikos PD, Androudi S, D'Amico DJ, Papadopoulos N, Dimitrakos SA, Dereklis DL, Alexandridis A, Lake S, Stangos NT. Perfluorocarbon liquid utilization in primary vitrectomy repair of retinal detachment with multiple breaks. Retina. 2003;23(5):615–621. doi: 10.1097/00006982-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Konstantinidis L, Berguiga M, Beknazar E, Wolfensberger TJ. Anatomic and functional outcome after 23-gauge vitrectomy, peeling, and intravitreal triamcinolone for idiopathic macular epiretinal membrane. Retina. 2009;29(8):1119–1127. doi: 10.1097/IAE.0b013e3181ac23da. [DOI] [PubMed] [Google Scholar]
- 25.Kusuhara S, Ooto S, Kimura D, Itoi K, Mukuno H, Miyamoto N, Akimoto M, Kuriyama S, Takagi H. Outcomes of 23- and 25-gauge transconjunctival sutureless vitrectomies for idiopathic macular holes. Br J Ophthalmol. 2008;92(9):1261–1264. doi: 10.1136/bjo.2008.140533. [DOI] [PubMed] [Google Scholar]
- 26.Guyomarch J, Delyfer MN, Korobelnik JF. Outcomes of 110 consecutive 25-gauge transconjunctival sutureless pars plana vitrectomies. J Fr Ophtalmol. 2008;31(5):473–480. doi: 10.1016/s0181-5512(08)72463-x. [DOI] [PubMed] [Google Scholar]
- 27.Gupta OP, Weichel ED, Regillo CD, Fineman MS, Kaiser RS, Ho AC, McNamara JA, Vander JE. Postoperative complications associated with 25-gauge pars plana vitrectomy. Ophthalmic Surg Lasers Imaging. 2007;38(4):270–275. doi: 10.3928/15428877-20070701-01. [DOI] [PubMed] [Google Scholar]
- 28.Lott MN, Manning MH, Singh J, Singh J, Zhang H, Singh H, Marcus DM. 23-gauge vitrectomy in 100 eyes: short-term visual outcomes and complications. Retina. 2008;28(9):1193–1200. doi: 10.1097/IAE.0b013e31817c5a28. [DOI] [PubMed] [Google Scholar]
- 29.Yanyali A, Celik E, Horozoglu F, Oner S, Nohutcu AF. 25-Gauge transconjunctival sutureless pars plana vitrectomy. Eur J Ophthalmol. 2006;16(1):141–147. doi: 10.1177/112067210601600123. [DOI] [PubMed] [Google Scholar]
- 30.Oshima Y, Ohji M, Tano Y. Surgical outcomes of 25-gauge transconjunctival vitrectomy combined with cataract surgery for vitreoretinal diseases. Ann Acad Med Singapore. 2006;35(3):175–180. [PubMed] [Google Scholar]
- 31.Misra A, Ho-Yen G, Burton RL. 23-gauge sutureless vitrectomy and 20-gauge vitrectomy: a case series comparison. Eye. 2009;23(5):1187–1191. doi: 10.1038/eye.2008.175. [DOI] [PubMed] [Google Scholar]
- 32.La Heij EC, Hendrikse F, Kessels AG. Results and complications of temporary silicone oil tamponade in patients with complicated retinal detachments. Retina. 2001;21(2):107–114. doi: 10.1097/00006982-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Singh CN, Lezzi R, Mahmoud TH. Intraocular pressure instability after 23-gauge vitrectomy. Retina. 2010;30(4):629–634. doi: 10.1097/IAE.0b013e3181c106de. [DOI] [PubMed] [Google Scholar]
- 34.Schweitzer C, Delyfer MN, Colin J, Korobelnik JF. 23-Gauge transconjunctival sutureless pars plana vitrectomy: results of a prospective study. Eye. 2009;23(12):2206–2214. doi: 10.1038/eye.2008.431. [DOI] [PubMed] [Google Scholar]
- 35.Horozoglu F, Yanyali A, Celik E, Aytug B, Nohutcu AF. Primary 25-gauge transconjunctival sutureless vitrectomy in pseudophakic retinal detachment. Indian J Ophthalmol. 2007;55(5):337–340. doi: 10.4103/0301-4738.33818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O'Reilly P, Beatty S. Transconjunctival sutureless vitrectomy: initial experience and surgical tips. Eye. 2007;21(4):518–521. doi: 10.1038/sj.eye.6702255. [DOI] [PubMed] [Google Scholar]
- 37.Azad RV, Chanana B, Sharma YR, Vohra R. Primary vitrectomy versus conventional retinal detachment surgery in phakic rhegmatogenous retinal detachment. Acta Ophthalmol Scand. 2007;85(5):540–545. doi: 10.1111/j.1600-0420.2007.00888.x. [DOI] [PubMed] [Google Scholar]
- 38.Rizzo S, Genovesi-Ebert F, Vento A, Cresti F, Di Bartolo E, Belting C. A new heavy silicone oil (HWS 46-3000) used as a prolonged internal tamponade agent in complicated vitreoretinal surgery: a pilot study. Retina. 2007;27(5):613–620. doi: 10.1097/01.iae.0000251228.33870.64. [DOI] [PubMed] [Google Scholar]
- 39.Tewari A, Shah GK, Fang A. Visual outcomes with 23-gauge transconjunctival sutureless vitrectomy. Retina. 2008;28(2):258–262. doi: 10.1097/IAE.0b013e318159ec5a. [DOI] [PubMed] [Google Scholar]
- 40.Ibarra MS, Hermel M, Prenner JL, Hassan TS. Longer-term outcomes of transconjunctival sutureless 25-gauge vitrectomy. Am J Ophthalmol. 2005;139(5):831–836. doi: 10.1016/j.ajo.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 41.Campo RV, Sipperley JO, Sneed SR, Park DW, Dugel PU, Jacobsen J, Flindall RJ. Pars plana vitrectomy without scleral buckle for pseudophakic retinal detachments. Ophthalmology. 1999;106(9):1811–1815. doi: 10.1016/S0161-6420(99)90353-6. [DOI] [PubMed] [Google Scholar]
- 42.Lai MM, Ruby AJ, Sarrafizadeh R, Urban KE, Hassan TS, Drenser KA, Garretson BR. Repair of primary rhegmatogenous retinal detachment using 25-gauge transconjunctival sutureless vitrectomy. Retina. 2008;28(5):729–734. doi: 10.1097/IAE.0b013e318162b01c. [DOI] [PubMed] [Google Scholar]
- 43.Haas A, Seidel G, Steinbrugger I, Maier R, Gasser-Steiner V, Wedrich A, Weger M. Twenty-three-gauge and 20-gauge vitrectomy in epiretinal membrane surgery. Retina. 2010;30(1):112–116. doi: 10.1097/IAE.0b013e3181b32ebf. [DOI] [PubMed] [Google Scholar]
- 44.Parolini B, Prigione G, Romanelli F, Cereda MG, Sartore M, Pertile G. Postoperative complications and intraocular pressure in 943 consecutive cases of 23-gauge transconjunctival pars plana vitrectomy with 1-year follow-up. Retina. 2010;30(1):107–111. doi: 10.1097/IAE.0b013e3181b21082. [DOI] [PubMed] [Google Scholar]
- 45.Millsap CM, Peyman GA, Mehta NJ, Greve MD, Lee KJ, Ma PE, Dunlap WA. Perfluoroperhydrophenanthrene (Vitreon) in the management of giant retinal tears: results of a collaborative study. Ophthalmic Surg. 1993;24(11):759–763. [PubMed] [Google Scholar]
- 46.Cheung BT, Lai TY, Yuen CY, Lai WW, Tsang CW, Lam DS. Results of high-density silicone oil as a tamponade agent in macular hole retinal detachment in patients with high myopia. Br J Ophthalmol. 2007;91(6):719–721. doi: 10.1136/bjo.2006.111526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lommatzsch A, Heimes B, Trieschmann M, Spital G, Pauleikhoff D. Long-term results after pars plana vitrectomy with 25 gauge technique. Ophthalmologe. 2008;105(5):445–451. doi: 10.1007/s00347-007-1629-3. [DOI] [PubMed] [Google Scholar]
- 48.Valmaggia C. Pars plana vitrectomy with 25-gauge instruments in the treatment of idiopathic epiretinal membranes. Klin Monbl Augenheilkd. 2007;224(4):292–296. doi: 10.1055/s-2007-962957. [DOI] [PubMed] [Google Scholar]
- 49.Scott IU, Flynn HW, Jr, Dev S, Shaikh S, Mittra RA, Arevalo JF, Kychenthal A, Acar N. Endophthalmitis after 25-gauge and 20-gauge pars plana vitrectomy: incidence and outcomes. Retina. 2008;28(1):138–142. doi: 10.1097/IAE.0b013e31815e9313. [DOI] [PubMed] [Google Scholar]
- 50.Wolf S, Schön V, Meier P, Wiedemann P. Silicone oil-RMN3 mixture (“heavy silicone oil”) as internal tamponade for complicated retinal detachment. Retina. 2003;23(3):335–342. doi: 10.1097/00006982-200306000-00008. [DOI] [PubMed] [Google Scholar]
- 51.Honavar SG, Goyal M, Majji AB, Sen PK, Naduvilath T, Dandona L. Glaucoma after pars plana vitrectomy and silicone oil injection for complicated retinal detachments. Ophthalmology. 1999;106(1):169–176. doi: 10.1016/S0161-6420(99)90017-9. [DOI] [PubMed] [Google Scholar]