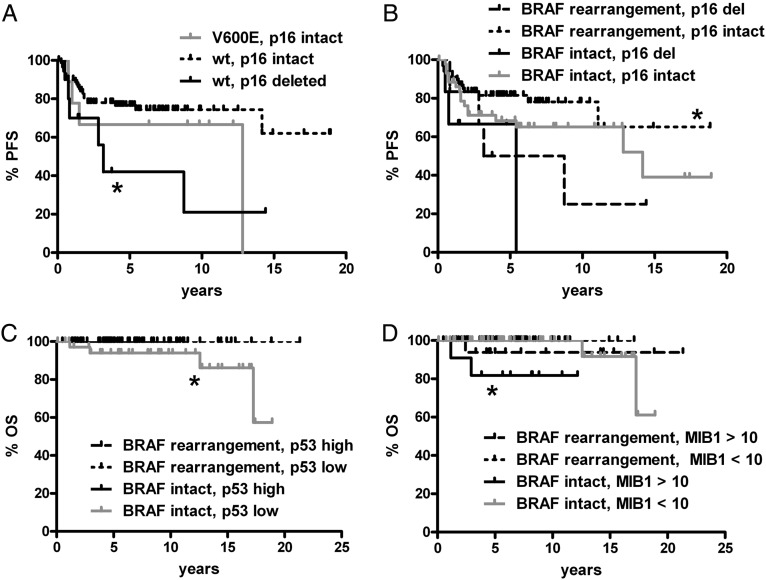
Fig. 7.
Significant PFS and OS associations in pediatric low-grade gliomas by BRAF V600E or rearrangement and p16, p53, or MIB1. All subregions were pooled together; all comparisons not marked with an asterisk (or not shown) are not significant. (A) Tumors without BRAF V600E (wild type [wt] BRAF) but with p16 deletion had shorter PFS than wt BRAF tumors where p16 was intact (*P = .02 vs V600E, p16 intact). There was only 1 case with concomitant V600E mutation and p16 deletion—a left temporal PXA that progressed after 5.4 years, though the patient is alive 10.3 years after original surgery. (B) Likewise, tumors that had both BRAF rearrangement and intact p16 had better PFS than those with p16 deletion regardless of BRAF status (*P = .049 vs BRAF rearrangement, p16 deleted; *0.03 vs BRAF intact, p16 deleted). (C) OS (*P = .03) was shorter in gliomas with intact BRAF and low p53 expression compared with those with low p53 and BRAF rearrangement. PFS also showed a strong trend in the same direction (P = .06, not shown). (D) Tumors with intact BRAF and high MIB1 proliferation index had shorter OS than tumors with a lower proliferation index and either intact or rearranged BRAF (*P = .007 and .0008, respectively). There was also a trend toward worse OS in BRAF-rearranged tumors when MIB1 was high compared with BRAF-rearranged tumors with low MIB1 (P = .06). Del, deleted.