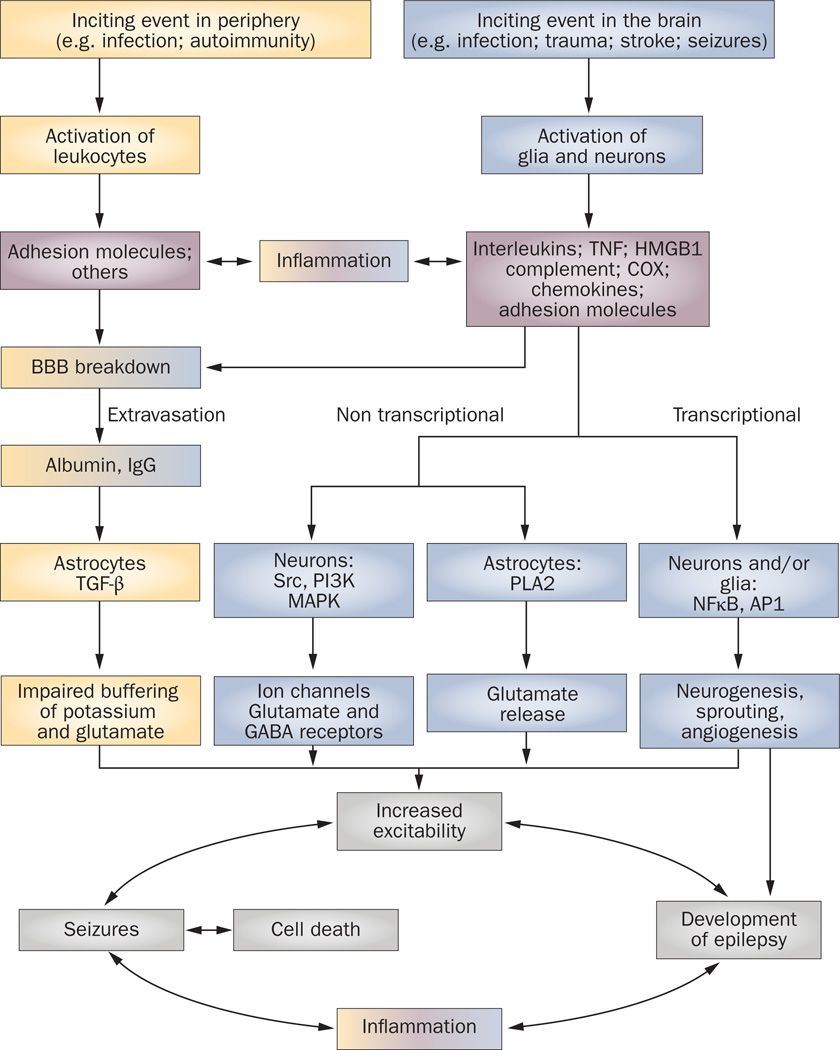
Figure 1. Pathophysiological cascade of inflammatory events in epilepsy.
Pathological events intiated in the CNS by local injuries, or peripherally following infections or as a result of autoimmune disorder, can lead to activation of brain cells or leukocytes, respectively. These cells release inflammatory mediators into the brain or blood, thereby eliciting a cascade of inflammatory events that cause a spectrum of physiopathological outcomes. The effects of brain inflammation contribute to the generation of individual seizures and cell death, which, in turn, activates further inflammation, thereby establishing a vicious circle of events that contributes to the development of epilepsy. The peripheral pathway is shown in yellow, the CNS pathway is shown in blue, and the inflammatory molecules are shown in pink. The merged colors indicate the contribution of each pathway to inflammation and BBB damage. Abbreviations: AP1, activator protein 1; BBB, blood–brain barrier; COX, cyclooxygenase; GABA, γ-aminobutyric acid; HMGB1, high-mobility group box 1; MAPK, mitogen-activated protein kinase; NFκB, nuclear factor kappa B; PI3K, phosphoinositide 3-kinase; PLA2, phospholipases A2; TGF-β, transforming growth factor β; TNF, tumor necrosis factor.