Abstract
Objective
To examine family conflict, parental blame, and poor family cohesion as predictors of treatment outcome for youth receiving family-focused cognitive behavioral therapy (FCBT) for obsessive compulsive disorder (OCD).
Methods
We analyzed data from a sample of youth who were randomized to FCBT (n = 49; 59% male; mean age = 12.43 years) as part of a larger randomized clinical trial. Youngsters and their families were assessed by an independent evaluator (IE) pre- and post- FCBT using a standardized battery of measures evaluating family functioning and OCD symptom severity. Family conflict and cohesion were measured via parent self-report on the Family Environment Scale (FES; Moos & Moos, 1994) and parental blame was measured using parent self-report on the Parental Attitudes and Behaviors Scale (PABS; Peris, 2008b). Symptom severity was rated by IE’s using the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS; Scahill et al., 1997).
Results
Families with lower levels of parental blame and family conflict and higher levels of family cohesion at baseline were more likely to have a child who responded to FCBT treatment even after adjusting for baseline symptom severity compared to families who endorsed higher levels of dysfunction prior to treatment. In analyses using both categorical and continuous outcome measures, higher levels of family dysfunction and difficulty in higher number of domains of family functioning were associated with lower rates of treatment response. In addition, changes in family cohesion predicted response to FCBT controlling for baseline symptom severity.
Conclusions
Findings speak to the role of the family in treatment for childhood OCD and highlight potential targets for future family interventions.
Keywords: childhood OCD, treatment outcome, predictors, family factors
Exposure-based cognitive behavior therapy (CBT) is well documented as an effective and relatively robust intervention for pediatric obsessive compulsive disorder (OCD; Barrett, Farrell, Pina, Peris, & Piacentini, 2008), and its advantages over SRI medication in terms of safety and response durability make it the current first-line treatment for pediatric OCD (Barrett et al., 2008; Brown et al., 2008; Watson & Rees, 2008). Despite its encouraging success rates, however, large numbers of youth fail to respond to CBT or exhibit only partial response. Indeed, findings from the Pediatric OCD Treatment Study (POTS; POTS Study Group, 2004), the largest pediatric OCD trial to date, indicate that well over half the youth receiving CBT failed to achieve optimal response. Although the addition of sertraline improved clinical outcomes, fully 46% of youth receiving combined treatment were deemed non-remitters. Notably, site effects for CBT and sertraline complicate interpretation of study findings and may contribute to an unduly bleak picture of outcomes. Recent reviews of the clinical trials literature are somewhat more encouraging, suggesting non-response rates for CBT ranging from 14%-54% (Barrett et al., 2008; Storch et al., 2008). Nonetheless, it is clear that there is much to be done to improve treatment outcomes for youth with OCD.
Efforts to improve treatment outcome increasingly have focused on family factors that may be relevant for course of illness and ultimate clinical outcome. Families are integral to all child and adolescent therapy to the extent that they facilitate treatment attendance and homework completion and bridge the gap between treatment sessions and home life. However, families play a particularly important role in CBT for OCD because they frequently are required to aide in or encourage the exposure exercises that are central to the intervention (Choate-Summers et al., 2008; Freeman et al., 2003). These exercises are intrinsically anxiety-provoking for children, and frequently for their parents, and they require family members to manage and tolerate emotional distress while simultaneously problem-solving potential resistance.
Research on pediatric OCD reveals an array of family dynamics that may serve to complicate these tasks (Ivarsson & Larsson, 2008; Lenane, 1989; Piacentini et al., 2003; Storch et al., 2008). Families of youth with OCD are characterized by high rates of family distress, disrupted family functioning, and accommodation of OCD symptoms (Peris et al., 2008a; Piacentini et al., 2003; Storch et al., 2007). In addition, recent research suggests that these families also report high rates of family discord and blame (Peris, Benazon, Langley, Roblek, & Piacentini, 2008b). This is not surprising given the burden of disease associated with OCD and the level of disrupted functioning that these families report (Ivarsson & Larsson, 2008; Piacentini et al., 2003). Indeed, work by Allsopp and Verduyn (1990) found that fully 20% of parents of adolescents with OCD endorsed responding to their children with “open anger,” underscoring the emotional upheaval with which these families contend. The pervasiveness of hostile, blaming response styles and family reports of distress and disrupted interpersonal functioning (Hibbs, Hamburger, & Lenane, 1991; Peris, et al., 2008a, b; Piacentini et al., 2003) make it likely that families will exhibit difficulty across multiple domains of functioning; however, there has been little systematic examination of how family risk factors aggregate in families of youth with OCD.
In addition, although a growing body of research documents the family correlates of childhood OCD, there is relatively less information about how these features relate to treatment outcome. In a recent review of the literature on predictors of treatment response for pediatric OCD, Ginsburg and colleagues (2008) reported that only six of the 21 studies reviewed examined family predictors of treatment outcome and only three of those did so in the context of CBT trials. These trials paint a mixed picture, with Barrett et al. (2005) finding that higher levels of family dysfunction as measured by the Family Assessment Device (Epstein et al., 1983) predicted poorer 18-month follow-up status and Wever and Rey (1997) finding no such links when the Family Environment Scale was used (FES; Moos & Moos, 1994). The third trial by Bolton and colleagues (1995) found no link between parental psychopathology and long-term treatment outcome for adolescents receiving CBT. More recently, several independent research groups have found that higher pre-treatment levels of family accommodation are linked to poorer treatment response (Garcia et al., 2010) and that changes in family accommodation (Merlo et al., 2009; Piacentini et al., under review) predict treatment outcome for youth receiving CBT for OCD. Despite this emerging literature, however, extant research on family predictors of treatment outcome has examined a relatively narrow set of family features and produced an inconclusive pattern of findings.
In light of the general dearth of research on family-level predictors of treatment outcome, it is not surprising that protective factors have been wholly overlooked. That is, no studies of pediatric OCD have examined positive features of the home environment that may support or optimize treatment response. One feature likely to buffer families against the strain imposed by OCD is family cohesion, or the extent to which families support and encourage one another. Considerable literature documents the benefits that accrue to children in homes with high levels of family cohesion, noting its links to higher levels of global child well-being (Vandeleur, Jeanpetre, Perrez, & Schoebi, 2009) and its beneficial effects on both internalizing and externalizing behavior problems over time (Lucia & Breslau, 2006). Indeed, among youth with anxiety and comorbid major depression, family cohesion has been found to predict treatment outcome for youngsters receiving CBT plus imipramine (Bernstein et al., 2001). Conversely, low levels of cohesion have been linked to higher levels of expressed emotion (EE), a known risk factor for relapse, among adolescents with Bipolar Disorder, and there has been a call to include cohesion as a treatment target in family intervention (Sullivan & Miklowitz, 2010). Thus, higher levels of cohesion may buffer children against adverse clinical outcomes and lower levels of cohesion may serve as risk factors for such sequelae. Cohesion is of particular interest in the sphere of pediatric OCD given that youth with OCD have been found to report less warmth and support from their parents compared to youth without the disorder (Valleni-Basile, Garrison, & Jackson, 1995).
In an effort to expand the scope of research examining family predictors of treatment response to encompass a broader range of family features, the present investigation examined family conflict, blame, and cohesion as predictors of treatment outcome for youth with OCD undergoing CBT. Building on research which documents conflict, blame and poor family cohesion as correlates of pediatric OCD (Peris et al., 2008a), we examined each risk indicator separately in relation to treatment outcome, adjusting for underlying symptom severity. In addition, because these variables are likely to be inter-related, we examined the cumulative effects of multiple family risk factors on treatment outcome. We hypothesized that (a) high levels of family conflict and blame, and low levels of cohesion would be independently related to poor treatment outcome, controlling for baseline symptom severity, with poorer functioning on each of these measures linked to poorer treatment outcome; (b) family difficulty in these three areas would tend to cluster with families either have no problems or problems in multiple domains; (c) multidimensional family dysfunction (indicated by higher numbers of domains with poor family functioning) would be associated with poor treatment outcome for youth receiving CBT and (d) that changes in family dynamics as measured via parent self-report pre- and post-treatment would predict treatment outcome.
Method
Participants
Participants were drawn from a larger randomized clinical trial comparing individual cognitive behavioral treatment with a systematic family component (FCBT) to psychoeducation and relaxation training (PRT; full sample n = 71). The primary sample for the current study consisted of the 49 youth ages 8-17 years (Mean age = 12.4 years; SD= 2.6 years) and their families who were randomized to FCBT. The overarching clinical trial was conducted at an OCD specialty program at a large Western academic medical center, and it employed the following inclusion criteria: (1) primary diagnosis of OCD (Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition, DSM-IV; APA, 1994); (2) a Children’s Yale-Brown Obsessive Compulsive Scale (CYBOCS; Scahill et al., 1997) total score > 15; (3) IQ>70; and (4) the absence of any psychotropic medication for OCD at study entry. Youth were permitted to participate if they were taking other psychotropic medications, and 6 participants (8.5%) entered the study on medication. Participants were excluded if they met criteria for any psychiatric illness that contraindicated study participation (e.g., suicidality, psychosis, mania, pervasive developmental delay); other comorbidities (e.g., depression, non-OCD anxiety) were permitted as long as they were secondary to OCD. Of the 49 youth in the FCBT condition, 40.8% were male. Most were identified by parents as Caucasian (77.6%), with the remainder designated as Latino (10.2%), Asian (4.1%), African American (2.0%), and Other (6.1%). The majority of youngsters came from intact homes with 77.8% living with their married biological parents. Although our focus was on the role of family factors in outcome for FCBT, study characteristics for participants in both arms of the study are displayed in Table 1 for reference.
Table 1.
Descriptive Statistics for Key Measures of Interest
| Measure | FCBT | PRT | Full Sample |
|---|---|---|---|
| N=49 | N=22 | N= 71 | |
| Child Ageb | 12.43 (2.65) | 11.59 (1.99) | 12.17 (2.48) |
| Gender (% Male) | 59.2% | 72.7% | 63.4% |
| Baseline CY-BOCS Total Score | 24.69 (4.81) | 25.27 (4.45) | 24.87 (4.67) |
| Obsessions | 11.63 (2.60) | 12.27 (2.14) | 11.83 (2.47) |
| Compulsions | 13.06 (2.76) | 13.00 (2.92) | 13.04 (2.80) |
| Baseline Family Conflict a, b (FES) | 3.44 (2.20) | 3.72 (2.09) | 3.53 (2.16) |
| Baseline Family Cohesiona (FES) | 6.97 (2.06) | 7.18 (1.92) | 7.03 (2.00) |
| Baseline Parental Blame (PABS)c | 13.63 (6.11) | 12.32 (2.83) | 13.21 (5.32) |
| CGI-I Responder b | 57.1% | 27.3% | 52% |
| Post-treatment Conflictd (FES) | 2.93 (2.00) | 3.76 (2.02) | 3.18 (2.03) |
| Post-treatment Cohesiond (FES) | 7.26 (1.73) | 7.24 (2.02) | 7.26 (1.81) |
Note.
Among youth in the FCBT arm, n=48 for the three family measures and the corresponding values for the full sample are for n = 70; no values were missing for youth in the PRT condition.
Higher scores on the conflict scale indicate lower levels of family conflict.
Indicates significant group differences between the FCBT and PRT groups.
At post treat-treatment, n = 39 for measures of conflict and cohesion in the FCBT group and n =56 for the full sample.
FCBT= Family-focused Cognitive Behavioral Therapy; CY-BOCS = Children’s Yale-Brown Obsessive Compulsive Scale (Scahill et al., 1997). FES= Family Environment Scale (Moos & Moos, 1994). CGI-I = Clinician Global Impressions-Improvement Scale (NIMH, 1985). For the conflict subscale, higher scores indicate lower levels of conflict. PABS= Parental Attitudes and Behaviors Scale (Peris et al., 2008b).
Measures
Anxiety Disorders Interview Schedule Child and Parent Versions (ADIS-C/P; Silverman & Albano, 1996)
The ADIS-C/P is a semi-structured psychiatric diagnostic interview administered separately to parent and child. A clinical severity rating (CSR) of 4 or higher on a 0-8 scale is indicative of clinically significant disorder and was required for a diagnosis of OCD. The ADIS has demonstrated sound psychometric properties (Silverman, Saavedra, & Pina, 2001; Wood et al., 2002). Although we did not conduct a formal reliability assessment, excellent agreement on OCD diagnosis (k = .89) was found between study diagnosticians and a best-estimate derived from case conference consensus in an overlapping sample to the present study (Wood et al., 2002).
Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS; Scahill et al., 1997)
The CY-BOCS is a semi-structured clinician-rated measure consisting of 10 items rated on a 5-point Likert scale. Separate scores are computed for obsessions and compulsions, and a total severity score is determined by summing all 10 items. The CY-BOCS possesses sound internal consistency, and test-re-test- reliability (Scahill et al., 1997; Storch et al., 2004), and it has demonstrated adequate treatment sensitivity (POTS, 2004).Independent rating of 37% of randomly-selected CYBOCS audiotapes (n=26 of full sample) indicated excellent inter-rater reliability for this measure at baseline (n=26; ICC=.96) and post-treatment (n=23; ICC=.99). In the present sample, Cronbach’s α = .73 for the total score.
Family Environment Scale (FES, Moos &Moos, 1994)
The original FES is a 90-item self-report measure designed to tap ten domains of family social functioning. The measure was administered to parents and the following two dimensions were employed in the present study: Cohesion, or the degree to which family members support each other, and Conflict, a measure of overt discord among family members. Internal consistency in the present sample was good to adequate: Cohesion, α = .72, Conflict, α = .68.
Parental Attitudes and Behaviors Scale (PABS; Peris et al., 2008b)
The PABS is a 24-item parent-report measure of attitudes and behaviors related to their child’s OCD. It consists of three scales: Blame, (e.g., “I believe my child does the OCD behaviors on purpose.”), Accommodation, (e.g., “I help to carry out my child’s rituals.”), and Empowerment (e.g., “I tell my child to resist his/her OCD behaviors.”). The PABS has demonstrated good concurrent and predictive validity (Peris et al., 2008b). It was administered at baseline only and the Blame subscale was used the present analyses (α = .88).
Clinical Global Impression –Improvement Scales (CGI-I, NIMH, 1985)
The CGI-I provides a global rating of clinical improvement from baseline with scores ranging from 1 (very much improved) to 7 (very much worse). It has been used widely as a primary measure of treatment outcome across clinical trials for a range of mental health conditions (Brent et al., 2008; POTS Team, 2004; TADS Team 2004; Walkup et al., 2008). Independent Evaluators (IEs) blind to study condition provided a CGI-I rating at weeks 4, 8, and 14 (post-treatment). Participants receiving a CGI-I rating of 1 (very much improved) or 2 (much improved) were considered treatment responders.
Procedure
This study was conducted in compliance with the Institutional Review Board and registered with clinicaltrials.gov (NCT00000386). Families interested in the study completed an initial telephone screening to ascertain potential eligibility. They were then invited to the clinic to complete informed consent/assent and a baseline evaluation to determine final study eligibility. Participants were diagnosed using the Anxiety Disorders Interview Schedule, fourth edition (ADIS-IV; Silverman & Albano, 1996), which was administered, along with the Children’s Yale-Brown Obsessive Compulsive Scale (Scahill et al., 1997), by IEs trained according to the procedures outlined by the instruments’ developers. Participants also completed a battery of standardized self-report measures assessing OCD-specific functional impairment, family dynamics, and comorbid symptomatology.
After completion of the baseline assessment and final determination of study eligibility, participants were randomly assigned to twelve sessions over fourteen weeks of either FCBT or PRT comparison treatment. The FCBT condition consisted of 12 90-minute treatment sessions administered over 14 weeks. Each session included 60 minutes of individual child treatment (exposure and response prevention; ERP) and 30 minutes of family treatment addressing the following topics: disengagement from OCD symptoms, reducing blame, differentiating OCD and non-OCD behaviors, limit setting, and identifying and addressing barriers to treatment (see Appendix). The PRT condition followed the same schedule and consisted of more global psychoeducation about OCD and progressive muscle relaxation. Trained evaluators blind to treatment condition conducted assessments at post-treatment and CGI-I ratings of 1 or 2 were used to designate responder status. Additional study details are described by Piacentini et al. (under review).
Results
Data Processing and Preliminary Analyses
Our primary analysis was performed on an intent-to-treat basis, using all available data from the 49 youth randomized to the FCBT condition. Consistent with the analyses in the primary efficacy study (Piacentini et al., submitted) subjects who did not provide data at follow-up were considered non-responders and for continuous measures we used the last observation carried forward (LOCF) for subjects who were missing values at the end of treatment.1 We began by obtaining graphical and descriptive statistics for the key demographic, clinical, and family measures. Table 1 shows baseline means and standard deviations (continuous measures) and frequencies (categorical measures) for all variables and the corresponding values for the family and outcome measures post treatment. While our focus is on the participants in the FCBT condition, we include summary statistics for the PRT comparison group for reference. We were particularly interested in high/low splits for the family functioning variables as we expected that these measures would be correlated such that families would tend to show clusters of dysfunction rather than problems in individual domains. Along these lines, we expected that the effects of family dysfunction on treatment response would be exacerbated by the presence of difficulty in multiple domains of functioning. In the absence of existing clinical cut-offs for families of youth with OCD on our variables of interest, we made an empirical decision based on visual inspection of plots for blame, conflict, and cohesion. The plots for all three measures were unimodal with an approximately symmetric distribution for conflict, some mild left skew for cohesion as measured by the FES, and mild right skew for parental blame as measured by the PABS. For all three measures the means and medians were similar and there were no natural breakpoints in the distributions suggesting a different split. Based on this and on prior experience with the measures, we chose to use the mean as a cut-point in analyses examining high/low splits on family functioning. Missing covariate data at baseline were rare, with one subject having no blame score and one subject missing the conflict and cohesion scores and we therefore used simple mean substitution to fill in these values.
Analyses of Individual Family Risk Factors
To examine links between the individual family functioning measures and FCBT treatment response, our primary analytic technique was logistic regression with CGI-I response status as the outcome and baseline Blame, Cohesion and Conflict as predictors adjusting for baseline symptom severity (CY-BOCS score). In all three models baseline CY-BOCS was not significant but the family measures were: Blame p = .016, Cohesion p = .005, conflict p =.019. As expected, higher levels of parental blame on the PABS were associated with a lower likelihood of treatment response (defined as CGI-I scores = 1 or 2) with an odds ratio of OR = 0.84 per one point increase in raw blame score (adjusted for baseline symptom severity) or OR=.40 for a 1 SD increase in blame levels (standardized effect size). Similarly, higher levels of family conflict on the FES were associated with a lower likelihood of treatment response (OR = .69 per 1 point increase in conflict or OR= .44 for a 1 SD increase), and higher levels of FES cohesion were associated with a higher likelihood of response (OR = 1.94 per one point increase in cohesion or OR =3.74 for a 1 SD increase). Follow-up analyses using only the 41 completers produced the same pattern of effects with only minor changes in the estimates and p-values.
We also performed secondary analyses using linear regression with the 14 week CY-BOCS score as the outcome, each of the family factors as a predictor and baseline CY-BOCS score as a covariate. These analyses were not completely parallel since they assessed total post-treatment symptoms rather than directly examining improvement. The basic pattern of results was the same with the continuous outcome measure except that they were somewhat weaker for blame and conflict and, not surprisingly, the baseline CY-BOCS score was also a significant predictor of the final raw symptom score.
Rates of Family Dysfunction
To examine the degree to which risk factors would be clustered in families of youth with OCD, we first looked at correlations among the key study measures (see Table 2). Baseline blame, conflict and cohesion were all strongly significantly correlated with each other at baseline and with post-treatment CY-BOCS score. To examine the cumulative effects of these risk factors we also created a risk scale by dichotomizing the three family variables as described above into high versus low using the sample mean as the cut-point and counting the number of domains in which the families reported problems (0,1, 2 or 3). If risk factors are correlated we would expect to find excess numbers of families with problems in all or no domains. Among families in the FCBT arm, 29% had no elevated risk factors and 20% had elevations in all three domains (see Table 3). To examine this further, we computed the proportion of families rated high on each risk factor using the entire sample. Using a chi-squared goodness of fit test we found that the observed distribution of family risk factors for the FCBT group was significantly different from the expected values under the assumption of independence (X2 (3) = 17.45, p = .0006) with the higher than expected counts corresponding to elevations in all or no domains as noted above. This cumulative count of elevated family dysfunction indicators was used in subsequent analyses.
Table 2.
Bivariate Correlations among Key Study Measures for Youth Randomized to Family Focused CBT
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Baseline CY-BOCS | 1 | ||||
| 2. Baseline Family Conflict | .12 | 1 | |||
| 3. Baseline Family Cohesion | -.05 | -.48** | 1 | ||
| 4. Baseline Parental Blame | .31* | .41* | -.47** | 1 | |
| 5. Post-tx CY-BOCS | .34* | .23 | -.42** | .33* | 1 |
Note: N = 49;
= p < .01,
= p <.05;
CY-BOCS = Children’s Yale-Brown Obsessive Compulsive Scale
Table 3.
Chi-square Analyses of Family Functioning by Treatment Response for the Intent to Treat Sample
| Number of Family Risk Factors | Non-Responder | Responder | Total |
|---|---|---|---|
| 3 | 9 | 1 | 10 |
| 43% | 4% | 20% | |
| 2 | 7 | 6 | 13 |
| 33% | 21% | 27% | |
| 1 | 4 | 8 | 12 |
| 19% | 29% | 24% | |
| 0 | 1 | 13 | 14 |
| 5% | 46% | 29% |
X2(3) = 17.45, p = .001 for comparing non-responders to responders. Table shows counts and column percentages.
Examining Linkages Between Multiple Family Risk Factors and Outcome
Next we examined the relationship between our cumulative count of family dysfunction indicators and treatment outcome. As shown in Table 3, having multiple domains of relatively poorer family functioning is linked to a lower likelihood of treatment response, even when families are systematically involved in treatment. Notably, only 1 of the 10 participants with elevated scores on all three measures of family functioning met criteria for responder status as determined by CGI scores of 1 or 2. By contrast, 93% of participants in families with no elevated family measure scores were designated treatment responders. From another perspective, 81% (21/26) of families with a Family Risk score of 1 or lower responded to treatment as compared to only 30% (7/23) of families with a risk score of 2 or greater, X2 (3) = 17.45, p = .001.
Predicting FCBT Treatment Outcome from Baseline Family Functioning
To formally test the connection between number of domains of dysfunction and treatment response described above, we fit a logistic regression with the CGI-I as the outcome and the cumulative dysfunction score as the predictor adjusting for baseline symptom severity on the CY-BOCS. The overall model was significant (likelihood ratio X2 (2) = 19.74, p < .0001) and family dysfunction was a highly significant predictor (p =.0006). The corresponding odds ratio was OR = .26 meaning there was a 74% reduction in odds of response for each additional domain on which the family showed high levels of dysfunction (OR = .23 for a 1 SD increase on this scale.) Baseline symptom severity did not contribute any additional independent explanatory information about treatment response. Using fitted values from these analyses, we plotted the predicted probability of treatment response as a function of family risk at 4 different levels (0 = no risk elevations to 3 = elevations on all 3 family risk variables). Figure 1 displays these findings for baseline CY-BOCS total scores held constant at 15, 25 and 35, representing the low end, mean, and high-end of values observed in this sample. For youth at all three levels of symptom severity, the likelihood of favorable treatment response declined as the number of family risk factors rose. As before, we also conducted secondary analysis with week 14 CY-BOCS scores as the outcome and the family risk count as the predictor adjusting for baseline symptom severity. As in the logistic regression model above, it was highly significant, (t (46) = 2.87, p <.01).
Figure 1.
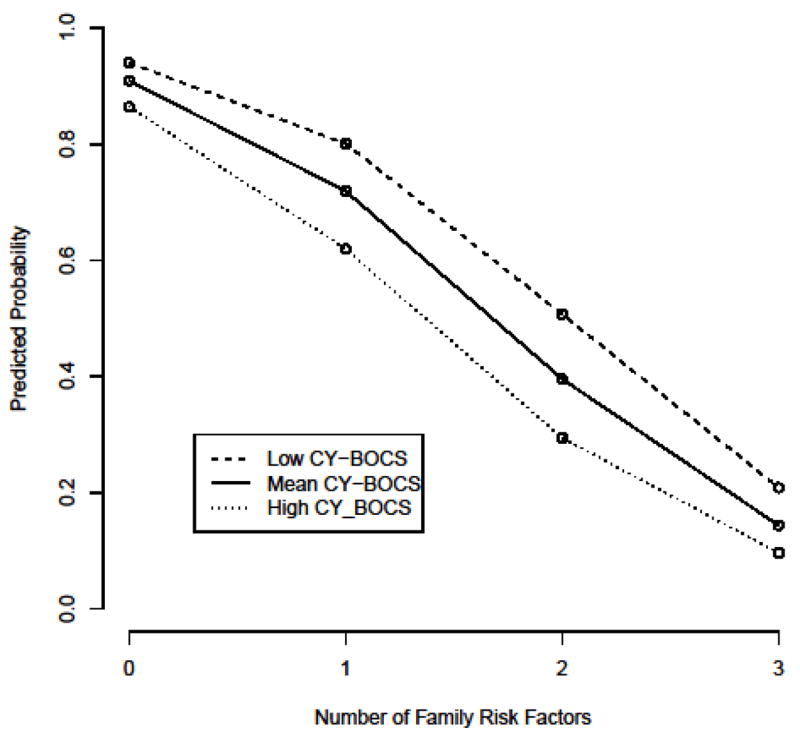
Predicted Probability of Treatment Response as a Function of Level of Family Dysfunction
Changes in Family Functioning as Predictors of FCBT Response
To examine whether changes in family conflict and cohesion pre- and post-treatment predicted acute treatment outcome, we ran logistic regression analyses with CGI-I responder status as the outcome. As this was an intent-to-treat analysis, participants who were missing follow-up data were assumed to have the same scores pre- and post-treatment. Changes in family cohesion significantly predicted treatment outcome after controlling for baseline symptom severity (p = .041, OR = 1.94 per 1 point increase in cohesion, OR = 3.74 per 1 SD change); however, changes in family conflict did not (p = .52, OR = 0.87). This may be due in part to the fact that changes in family cohesion and conflict over time were not statistically significant so that there may have been insufficient variability in conflict correlate with outcome. Parallel analyses were not run using the blame variable as the PABS was administered only at baseline.
Discussion
This study examined three indices of family functioning and their relationship to treatment outcome for youth receiving FCBT for OCD. In keeping with our hypotheses, families with lower levels of parental blame and family conflict and higher levels of family cohesion at baseline were more likely to have a child who responded to FCBT compared to families who endorsed higher levels of dysfunction prior to treatment. It was common for families to report difficulty in more than one domain of family functioning, and endorsement of multiple domains of dysfunction was associated with lower likelihood of treatment response. Indeed, children in families who demonstrated higher levels of functioning on all three family features assessed in this study, had a 93% response to FCBT. By contrast, youth in families with poorer functioning on all three family risk factors demonstrated only a 10% response rate. There was partial support for the hypothesis that changes in family functioning would predict treatment outcome, with changes in cohesion predicting clinical response but changes in family conflict showing no such links.
These findings speak to the important role of the family in treatment for childhood OCD, providing preliminary evidence that negative family dynamics may attenuate clinical outcomes. Symptoms of OCD impose a significant burden on both children and their families, and it is not uncommon for negative family dynamics to emerge in their wake. Prior research points to the tendency for some parents to blame their children for OCD symptoms (Peris et al., 2008a) and to respond to them with open anger and hostility (Allsopp & Verduyn, 1990). These negative interpersonal dynamics may not emerge for all families of youth with OCD—53% of families in the present sample reported zero or one family risk factors--and their prevalence may be somewhat over-estimated in older studies due to methodology and sampling (e.g., Hibbs et al., 1991). However, in cases where they do exist, they merit concern. Maladaptive family dynamics are specifically problematic for treatment because they are likely to create an emotionally charged environment that challenges the child’s ability to work on exposure exercises and the parent’s ability to provide support and assistance with them. Certainly there is evidence that parents who report higher levels of family conflict may have a more difficult time refraining from accommodation, a behavior likely to maintain OCD symptoms (Peris et al., 2008b). Several existing family treatments for pediatric OCD have produced encouraging reductions in symptom severity in part by providing families with strategies for disengaging from OC symptoms and supporting exposure-based exercises (Barrett et al., 2004; Storch et al., 2007; Storch et al., 2010). The present findings suggest that negative family dynamics may play their own role in influencing the treatment process and thus merit their own direct intervention. Indeed, two of the three family features we examined (cohesion and conflict) were not correlated with the child’s symptom severity at baseline suggesting that they are not merely markers of OCD severity.
The specific family features examined herein mark an expansion of previous research on family factors related to childhood OCD. With limited exception (e.g., Hibbs et al., 1991), the study of family-level variables associated with OCD has focused on accommodation (Storch et al., 2007; Peris et al., 2008a) or OCD-specific family impairment (Piacentini et al., 2007); affective family dynamics have received less attention. The present study provides evidence that the emotional climate at home—as measured via conflict, blame, and low levels of support or cohesion—may also be relevant for treatment outcome. These particular features of the home environment may be seen as an indication of family members’ ability to cope with the stress and upheaval caused by OCD and to manage emotions effectively. Given that parents are key agents in the coaching of emotion regulation (Eisenberg, Cumberland, & Spinrad, 1998; Fox & Calkins, 2003) and that CBT treatment for OCD involves confronting and tolerating uncomfortable emotions, the role of affective family dynamics in the treatment process merits further attention. Certainly the present findings are in keeping with research on other child and adolescent disorders indicating that affective dynamics such as expressed emotion and family conflict may moderate treatment outcome for youth receiving evidence-based psychosocial intervention (e.g., Feeny et al., 2009; Miklowitz et al., 2009).
The present finding that increasing levels of family dysfunction are linked to diminished treatment response underscores the importance of assessing multiple domains of family functioning at the outset of treatment. Such assessment may be used to identify areas of family strength and weakness and to personalize subsequent interventions. Several researchers have noted that family-focused treatments for OCD, while recommended by expert consensus (AACAP, 1998; Barrett et al., 2008; March et al., 1997), frequently fail to produce significant changes in family functioning (Barrett et al., 2008; Piacentini, March, Peris & Franklin, in press). Indeed, in the context of the present family-focused intervention for childhood OCD, families demonstrated minimal changes in conflict and cohesion post-treatment. While the reason for this larger pattern of findings is not entirely clear, it may be that current interventions, including our own, do not target the relevant variables or do not tackle them with sufficient intensity. The present findings suggest that blame, conflict, and cohesion may be important family targets, and they highlight changes in family cohesion as particularly important to clinical outcome. As current protocols rely primarily on psychoeducation and general behavior management techniques, there may be a need to employ a broader set of strategies aimed at emotion regulation and problem solving. In addition, as changes in family cohesion were found to predict treatment outcome, future interventions may need to emphasize strategies that help families build positivity and supportiveness in the home environment.
Several study limitations are worth noting. First, focus on the youth randomized to FCBT resulted in a relatively small sample size. Second, measures of family dynamics relied on self-report and future work will need to incorporate clinical interview and behavioral observation to refine assessment of relevant family features. Third, despite the longitudinal design, it is likely that multiple factors affect how youth respond to treatment and causality cannot be inferred from the present findings linking family functioning to treatment outcome. Fourth, levels of family dysfunction were assessed using high/low splits based on the sample mean. Given that these are not clinical cut-offs for family functioning, and indeed, such cut-offs do not exist with respect to families of youth with OCD, interpretation of the present findings should proceed with caution. Fifth, the CGI-I, while widely used in clinical trials research is a broad measure of global improvement and more fine grained assessment of treatment response—particularly in functional domains—would be helpful in future research. Finally, because this study was conducted in the context of a family-focused CBT intervention and the comparison group was relatively small by design, it is unclear whether these family variables retain a similarly important role for individually delivered child CBT. It may be the case that integrating high conflict, less cohesive families into a child’s treatment has an adverse effect on the clinical response because it requires the child to work on treatment tasks in a challenging family context, but that these treatment tasks (e.g., exposure exercises) become easier when extricated from difficult family dynamics. Future research will need to examine links between affective family dynamics for youth in traditional child-focused CBT, and to examine who benefits most from interventions aimed at these features.
These limitations notwithstanding, the present findings provide compelling preliminary evidence for links between higher levels of family dysfunction and lower rates of treatment response for youth receiving FCBT for OCD. They point to affective features of the home environment that may influence how youth fare in treatment, and highlight conflict, blame, and cohesion as potential targets of future treatments. Given that current family treatments have had limited success changing family dynamics (Barrett et al., 2008) and that the incremental benefit of family treatment over individual child treatment for OCD has yet to be established, emphasis on these family features may help to improve treatment outcomes for youth with OCD. Further work is needed to examine the role of conflict, blame, and cohesion in childhood OCD and the mechanisms by which negative family dynamics unfold.
Acknowledgments
This research was supported by NIMH grants K23 MH085058 (Peris) R01 MH58549 (Piacentini).
Appendix
Overview of Family Content in FCBT Sessions
Session 1: Initial psychoeducation about OCD and ERP treatment rationale
Session 2: Discussing impact of OCD on individual and family functioning
Session 3: Addressing negative attributions about children with OCD
Session 4: Minimizing blame
Session 5: Disengaging from accommodation
Session 6: Child’s responsibility for treatment/behavior management
Session 7: Addressing secondary gain
Session 8: Differentiating OCD and non-OCD behaviors
Session 9: Family self-care
Session 10: Review of family problems related to OCD/problem solving
Session 11: Relapse prevention
Session 12: Graduation
Footnotes
Parallel analyses were conducted using the 41 treatment completers in the FCBT condition and revealed a similar pattern of findings.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
References
- American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:27S–45S. doi: 10.1097/00004583-199810001-00003. [DOI] [PubMed] [Google Scholar]
- Allsopp M, Verduyn C. Adolescents with obsessive-compulsive disorder: a case note review of consecutive patients referred to a provincial regional adolescent psychiatry unit. Journal of Adolescence. 1990;13:157–169. doi: 10.1016/0140-1971(90)90005-r. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. [Google Scholar]
- Barrett P, Farrell L, Dadds M, Boulter N. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: long-term follow-up and predictors of outcome. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:1005–1014. doi: 10.1097/01.chi.0000172555.26349.94. [DOI] [PubMed] [Google Scholar]
- Barrett PM, Farrell L, Pina AA, Peris TS, Piacentini J. Evidence-based psychosocial treatments for child and adolescent obsessive compulsive disorder. Journal of Clinical Child and Adolescent Psychology Special Issue: Evidence-based psychosocial treatments for children and adolescents: A ten year update. 2008;37:131–155. doi: 10.1080/15374410701817956. [DOI] [PubMed] [Google Scholar]
- Bernstein GA, Hektner JM, Borchardt CM, McMillan MH. Treatment of school refusal: one-year follow-up. Journal of the American Academy of child and Adolescent Psychiatry. 2001;40:206–213. doi: 10.1097/00004583-200102000-00015. [DOI] [PubMed] [Google Scholar]
- Brown R, Antonuccio D, DuPaul G, Fristad M, King C, Leslie L, McCormick G, Pelham W, Piacentini J, Vitiello B. Childhood Mental Health Disorders: Evidence Base and Contextual Factors for Psychosocial, Psychopharmacological, and Combined Interventions. Washington DC: American Psychological Association Press; 2008. [Google Scholar]
- Choate-Summers ML, Freeman JB, Garcia AM, Coyne L, Przeworski A, Leonard HL. Clinical considerations when tailoring cognitive behavioral treatment for young children with obsessive compulsive disorder. Education & Treatment of Children. 2008;31:395–416. [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychological Inquiry. 1998;9:241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. Journal of Marital and Family Therapy. 1983;9:171–180. [Google Scholar]
- Feeny NC, Silva SG, Reinecke MA, McNulty S, Findling RL, et al. An exploratory analysis of the impact of family functioning on treatment for depression in adolescents. Journal of Clinical Child and Adolescent Psychology. 2009;38:814–825. doi: 10.1080/15374410903297148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox NA, Clakins SD. The development of self-control of emotion: Intrinsic and extrinsic influences. Motivation and Emotion. 2003;27:7–26. [Google Scholar]
- Freeman J, Garcia A, Fucci C, Karitani M, Miller L, Leonard HL. Family-based treatment of early-onset obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology. 2003;13:71–80. doi: 10.1089/104454603322126368. [DOI] [PubMed] [Google Scholar]
- Garcia AM, Sapyta JJ, Moore PS, Freeman JB, Franklin ME, March JS, Foa EB. Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1024–1033. doi: 10.1016/j.jaac.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Kingery JN, Drake KL, Grados MA. Predictors of treatment response in pediatric obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:868–878. doi: 10.1097/CHI.0b013e3181799ebd. [DOI] [PubMed] [Google Scholar]
- Hibbs E, Hamburger S, Lenane M. Determinants of expressed emotion in families of disturbed and normal children. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1991;32:757–770. doi: 10.1111/j.1469-7610.1991.tb01900.x. [DOI] [PubMed] [Google Scholar]
- Ivarsson T, Larsson B. The Obsessive-Compulsive Symptom (OCS) scale of the Child Behavior Checklist: a comparison between Swedish children with Obsessive-Compulsive Disorder from a specialized unit, regular outpatients and a school sample. Journal of Anxiety Disorders. 2008;22:1172–1179. doi: 10.1016/j.janxdis.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Lenane M. Families and obsessive compulsive disorder. In: Rapoport JL, editor. Obsessive-Compulsive Disorder in Children and Adolescents. Washington, DC: American Psychiatric Press; 1989. pp. 237–249. [Google Scholar]
- Lucia VC, Breslau N. Family cohesion and children’s behavior problems: A longitudinal investigation. Psychiatry Research. 2006;141:141–9 10. doi: 10.1016/j.psychres.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. Journal of Consulting & Clinical Psychology. 2009;77:355–360. doi: 10.1037/a0012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Axelson DA, George EL, Taylor DO, Schneck CD, Sullivan AE, Birmaher B. Expressed emotion moderates the effects of family-focused treatment for bipolar adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:643–651. doi: 10.1097/CHI.0b013e3181a0ab9d. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale manual. 3. Palo Alto, CA: Consulting Psychologists Press; 1994. [Google Scholar]
- NIMH. Clinical Global Impressions Scale. Psychopharmacology Bulletin. 1985;21:839–843. [Google Scholar]
- Pediatric OCD Treatment Study Team. Cognitive-behavioral therapy, sertraline, and their combination for children and adolescents with obsessive compulsive disorder: The Pediatric OCD Treatment Study (POTS) randomized controlled trial. Journal of the American Medical Association. 2004;292:1969–1976. doi: 10.1001/jama.292.16.1969. [DOI] [PubMed] [Google Scholar]
- Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J. Correlates of family accommodation of childhood obsessive compulsive disorder: Parent, child, and family characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 2008a;47:1173–1181. doi: 10.1097/CHI.0b013e3181825a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Roblek T, Langley A, Benazon N, Piacentini J. Parental responses to obsessive compulsive disorder: development and validation of the parental attitudes and behaviors scale (PABS) Child and Family Behavior Therapy. 2008b;30:199–214. [Google Scholar]
- Piacentini J, Bergman LB, Chang S, Langley A, Peris T, Wood J, McCracken J. Controlled Comparison of Family Cognitive Behavioral Therapy and Psychoeducation/Relaxation-Training for Child OCD. Journal of the American Academy of Child and Adolescent Psychiatry. doi: 10.1016/j.jaac.2011.08.003. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piacentini J, Bergman RL, Jacobs C, McCracken J, Kretchman J. Cognitive--behaviour therapy for childhood obsessive compulsive disorder: Efficacy and predictors of treatment response. Journal of Anxiety Disorders. 2002;16:207–219. doi: 10.1016/s0887-6185(02)00096-8. [DOI] [PubMed] [Google Scholar]
- Piacentini J, Bergman RL, Keller M, McCracken J. Functional impairment in children and adolescents with obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology. 2003;13:S61–S69. doi: 10.1089/104454603322126359. [DOI] [PubMed] [Google Scholar]
- Piacentini J, Peris TS, Bergman RL, Chang S, Jaffer M. The Child Obsessive-Compulsive Impact Scale-Revised (COIS-R): Development and psychometric properties. Journal of Clinical Child and Adolescent Psychology. 2007;36:645–653. doi: 10.1080/15374410701662790. [DOI] [PubMed] [Google Scholar]
- Piacentini J, Peris T, March J, Franklin M. Cognitive-behavioral therapy for youngsters with obsessive-compulsive disorder. In: Kendall P, editor. Child and adolescent therapy: Cognitive-behavioral procedures. 4. NY: Guilford; in press. [Google Scholar]
- Renshaw KD, Steketee G, Chambless DL. Involving family members in the treatment of OCD. Cognitive Behavior Therapy. 2005;34:164–175. doi: 10.1080/16506070510043732. [DOI] [PubMed] [Google Scholar]
- Scahill L, Riddle MA, McSwiggan-Hardin MT, Ort SI, King RA, Goodman WK, et al. Children’s Yale Brown Obsessive Compulsive Scale: Reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- Silverman W, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV: Parent Version. San Antonio, TX: Graywing; 1996. [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Steketee G. Social support as a predictor of follow-up outcome following treatment for OCD. Journal of Behavioural Psychotherapy. 1993;21:81–95. [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ. Family accommodation in pediatric obsessive-compulsive disorder. Journal of Clinical Child &Adolescent Psychology. 2007;36:207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- Storch EA, Merlo LJ, Larson MJ, Marien WE, Geffken GR, Jacob ML, Goodman WK, Murphy TK. Clinical features associated with treatment-resistant pediatric obsessive-compulsive disorder. 2008 doi: 10.1016/j.comppsych.2007.06.009. [DOI] [PubMed] [Google Scholar]
- Sullivan AE, Miklowitz DJ. Family functioning among adolescents with bipolar disorder. Journal of family psychology. 2010;24:60–70. doi: 10.1037/a0018183. [DOI] [PubMed] [Google Scholar]
- Valleni-Basile LA, Garrison CZ, Jackson KL, Waller JL, McKeown RE, Addy CL. Family and psychosocial predictors of obsessive compulsive disorder in a community sample of young adolescents. Journal of Child and Family Studies. 1995;4:193–206. doi: 10.1097/00004583-199407000-00002. [DOI] [PubMed] [Google Scholar]
- Vandeleur CL, Jeanprêtre N, Perrez M, Schoebi D. Cohesion, Satisfaction With Family Bonds, and Emotional Well-Being in Families With Adolescents. Journal of Marriage and Family. 2009;71:1205–1219. [Google Scholar]
- Watson HJ, Rees CS. Meta-analysis of randomized, controlled treatment trials for pediatric obsessive-compulsive disorder. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2008;49:489–498. doi: 10.1111/j.1469-7610.2007.01875.x. [DOI] [PubMed] [Google Scholar]
- Wever C, Rey JM. Juvenile obsessive-compulsive disorder. The Australian and New Zealand journal of psychiatry. 1997;31:105–113. doi: 10.3109/00048679709073806. [DOI] [PubMed] [Google Scholar]
- Wood J, Piacentini J, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Version. Journal of Clinical Child Psychology. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]


