Abstract
OBJECTIVES
To qualitatively explore differences in Leventhal's common sense model (CSM) constructs between youth with type 1 diabetes (T1D) and sickle cell disease (SCD) and between different age groups and level of disease control.
METHODS
Two structured individual interviews were conducted in 24 youth with T1D (n=12) or SCD (n=12). Patients were between 8 and 21 years of age, had either good or poor disease control, and were seen at an outpatient children's hospital medical clinic.
RESULTS
Youth conceptualize their chronic disease in terms of identity, cause, timeline, control, and consequences: both cognitive and emotional dimensions are apparent. There was considerable contrast between discussions of youth with well- and poorly controlled T1D but little contrast between youth with well- and poorly controlled SCD. Surprisingly, youth with well-controlled T1D mentioned emotions most frequently. No youth with poorly controlled T1D described disease acceptance, but the majority of youth with well-controlled T1D did. Adolescents and young adults with good T1D control appear to understand disease cause, have better illness coherence, and habitually link discussion of symptoms and negative emotions with solutions. Youth with poorly controlled T1D appeared more likely to connect symptoms with negative consequences. Consequences included 1) disease symptoms, 2) the need to perform self-care activities, 3) physical outcomes, 4) health-system activities, 5) emotions, and 6) life impact. Interestingly, sickling crisis was mentioned more frequently by youth with good SCD control than by those with poor SCD control. Youth with SCD are distressed by others' judgmental perceptions and by feeling different from others.
CONCLUSIONS
In contrast to previous CSM work, youth with well-controlled T1D in this study discussed emotions more frequently than did those with poor control. Disease perceptions were similar between youth with well- and poorly controlled SCD. Results indicate there are noteworthy cognitive and emotional differences between youth with different types of disease and levels of disease control.
INDEX TERMS: adolescent, anemia, child, diabetes mellitus, health behavior, sickle cell disease
INTRODUCTION
Leventhal's common sense model (CSM) is used to understand people's responses to illness.1 The model proposes that illness perceptions directly influence coping strategies, which in turn influence outcomes.2 Illness perceptions are lay interpretations of information and personal experiences the patient has acquired.3,4 They are posited to include 5 main cognitive domains: 1) identity (label and symptoms), 2) timeline, 3) consequences, 4) cause, and 5) perceived controllability or curability,2,5,6 plus 1 noncognitive domain: emotional perceptions.7 The model posits parallel-processing of cognitions and emotions.2 Research indicates youth do conceptualize disease dimensions similarly to adults, but these conceptualizations vary in sophistication and number.8,9
We chose type 1 diabetes (T1D) and sickle cell disease (SCD) because we expected to see a contrast in CSM constructs due to the difference in the relationship between therapy adherence and results. While poor therapy adherence can negatively impact the disease outcome for patients with either of these diseases, good adherence is highly likely to improve diabetes outcomes but not very likely to improve sickle cell outcomes. An estimated 15,000 youth below 20 years of age are diagnosed with T1D annually:10 its incidence increased 5.5% in the United States between 1990 and 1999.11 An estimated 50,000 persons in the United States have SCD.12 Most youth with T1D receiving appropriate treatment can control their disease, lead well-adjusted lives, and engage in most types of physical activity. In contrast, there are few effective treatments for those with SCD.13 Youth with SCD are typically restricted from strenuous activities and find it difficult to plan activities because pain episodes are unpredictable.14
Therapy adherence often declines in youth with either T1D7-19 or SCD15 as they move from childhood into adolescence and begin to assume responsibility for self-care. Because optimal self-care has the potential to reduce long-term complications from both diseases,13 a better understanding of how disease perceptions influence self-care in youth with chronic illnesses such as T1D and SCD as they begin to assume responsibility for maintaining and promoting their own health is important. This understanding will better enable us to develop appropriate assessment tools and intervention strategies to reduce the risk of complications from long-term disease.
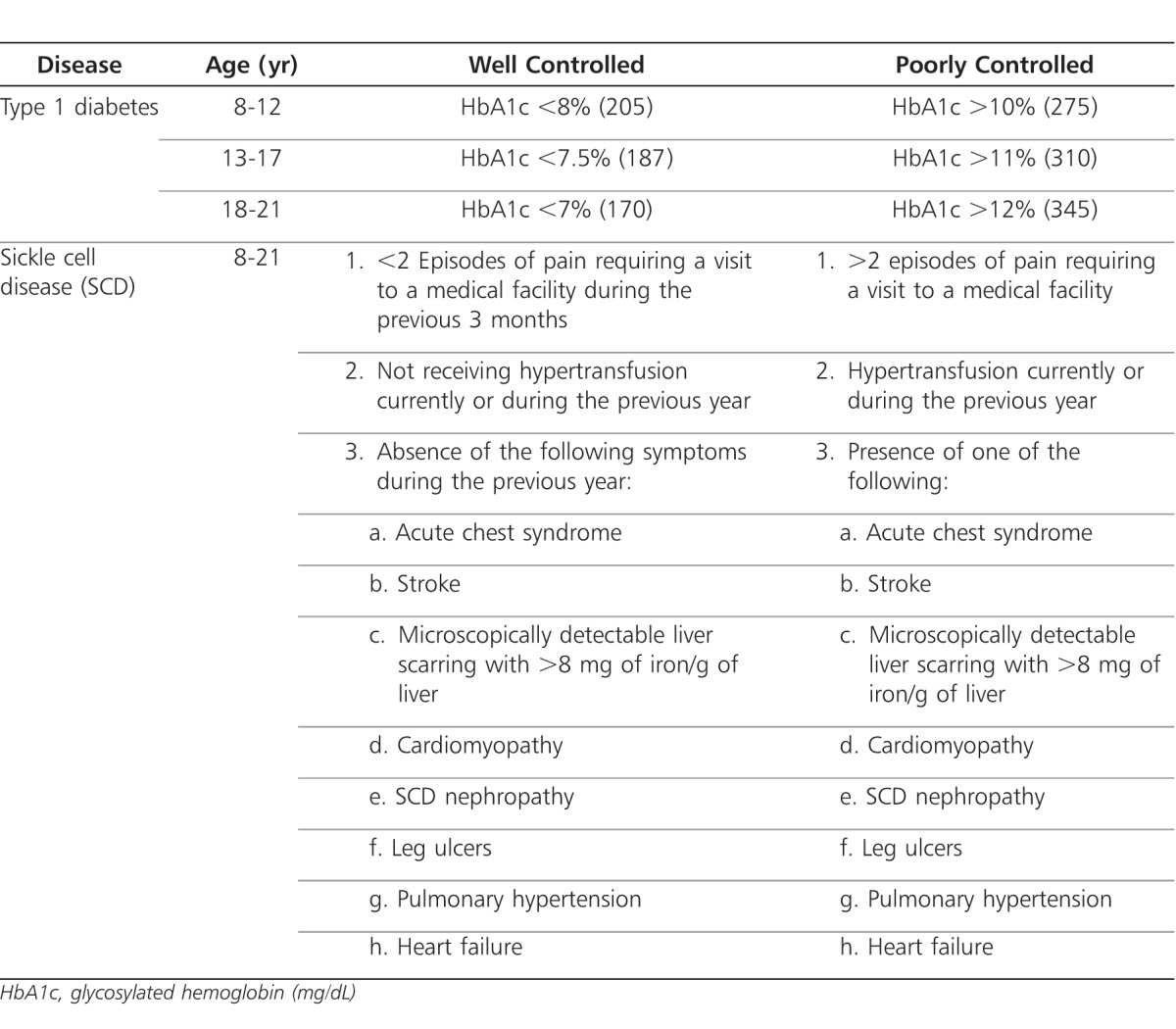
The study objectives were to qualitatively explore differences in CSM constructs between youth with T1D or SCD, different age groups, and level of a priori determined disease control. Level of disease control was based on glycosylated hemoglobin (HbA1c) in youth with T1D and symptoms and required treatments in youth with SCD (Table 1).
Table 1.
Classification of Level of Disease Control
MATERIALS AND METHODS
Data Collection
Two semistructured interviews were conducted with each of the 24 youth. The institutional review boards at the University of Georgia and the southern state hospital from which participants were recruited approved the study. Youth below 18 years of age signed assents; their parents and youth 18 years of age and older signed consents. Subjects were invited to participate during a regularly scheduled office visit. Parents were not present during the interviews, which were conducted in a private room.
Pre-scripted interview guides were based on those used in a previous CSM-based study among youth between 8 and 14 years of age.8 Interviews were conducted by research nurses and resident physicians, who were instructed to read the questionnaire verbatim and were provided with follow-up and probe questions. The first interview focused on illness representations, while the second interview addressed daily activities, symptoms, coping, and self-care activities. Interviews were tape-recorded and transcribed verbatim.
Participants
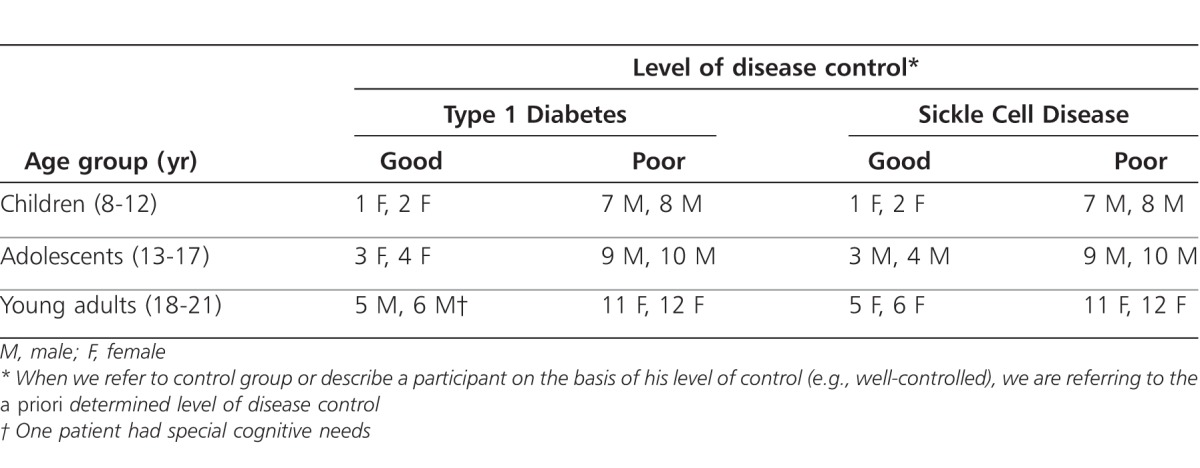
Patients who had been diagnosed with T1D or SCD at least 6 months earlier were recruited from a hospital-based pediatric endocrine clinic. All participants spoke English and were recruited without regard for sex. Two patients with well-controlled and 2 with poorly controlled disease were recruited for each of 3 age groups for both diseases. Participants were divided into 1 of 3 age groups: children (8 to 12 years), adolescents (13 to 17 years), and young adults (YAs; 18 to 21 years). The participant categorization scheme (used to identify quotations in the article) is presented in Table 2, which provides information on age, sex, disease, and disease control. When we refer to the control group or describe a participant on the basis of his level of control (eg, well-controlled), we are referring to the a priori determined level of disease control.
Table 2.
Participants by Diagnosis, Age Group, Sex, and Disease Control Level
T1D control was determined using current HbA1c value, which varied with age according to current American Type-1 Diabetes Association guidelines.16 Although we know that optimal self-care can improve HbA1c concentrations in children and adolescents,17,18 it can also be influenced by other factors, such as parental care19 or the metabolic changes of puberty.20 HbA1c may even have bidirectional aspects with self-care.21 To maximize self-care differences between the youth we selected participants with values near A1c scale extremes (Table 1). Level of SCD control was determined by reviewing charts to assess pain episodes requiring a medical facility visit during the previous 3 months, requiring a blood transfusion during the previous year, and presence/absence of specific symptoms (Table 1).
Analysis
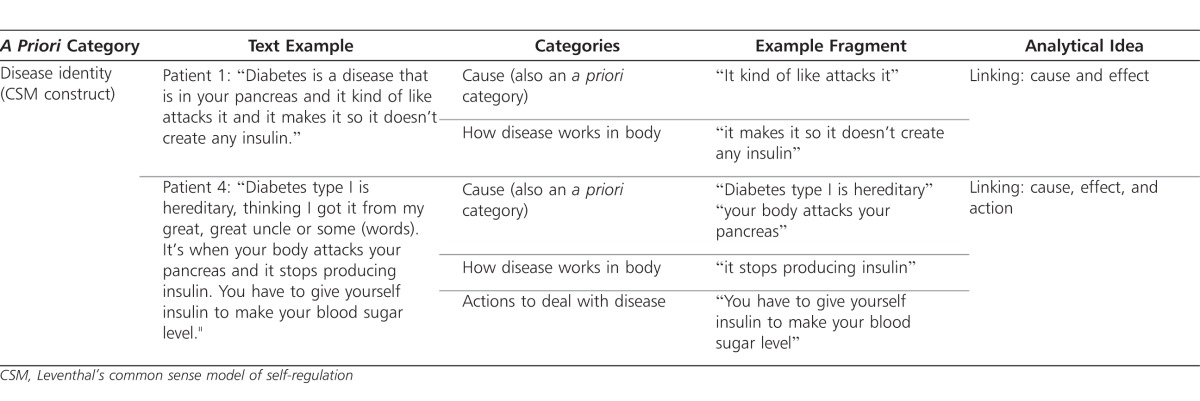
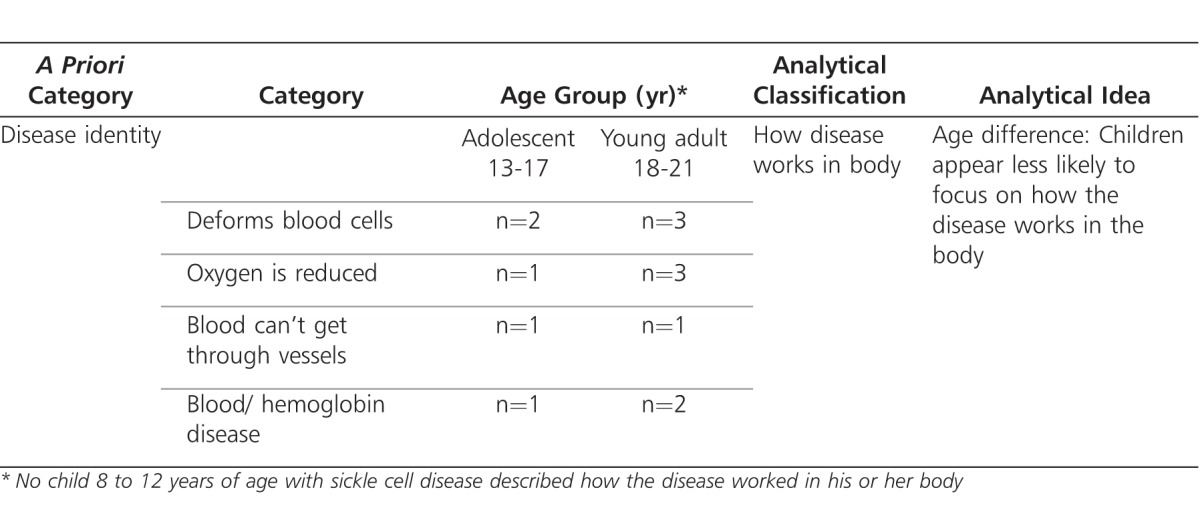
Transcripts were analyzed using a framework approach22 by the principal author using NVivo 8 (QSR International, Doncaster, Victoria, Australia) qualitative software, focusing on the CSM domains. Several theory-based coding categories were determined a priori (e.g., disease identity, symptoms, cause, timeline, control, and consequences) (Table 3). New categories and analytical ideas were developed after iterative readings, discussion, and feedback from the second author, who helped provide a broader perspective. Categories and themes were compared by disease, age group, and disease control level (Table 4). Quoted passages were edited into more readable form by eliminating embedded off-topic phrases or words.
Table 3.
Example of Coding Development: Type 1 Diabetes
Table 4.
Example of Comparative Analysis: Sickle Cell Disease and Age Group
RESULTS
Quotations presented in the article are identified by disease (T1D or SCD) and participant number, as assigned in Table 2. Twelve youth each with T1D or SCD were interviewed. Males were more likely to have poor disease control. One well-controlled YA with T1D, patient 6, had special cognitive needs but could speak and communicate well.
Identity and Cause
All youth with SCD knew it was inherited. There was considerably more response variation among youth with T1D; several offered more than 1 potential cause (Table 5). With the exception of the special needs subject (patient 6), only youth with poorly controlled T1D thought poor diet could cause T1D or did not know its cause. Youth with well-controlled T1D nominated more plausible and sophisticated causes.
Table 5.
Perceived Causes of Type 1 Diabetes in Children, Adolescents, and Young Adults With the Disease
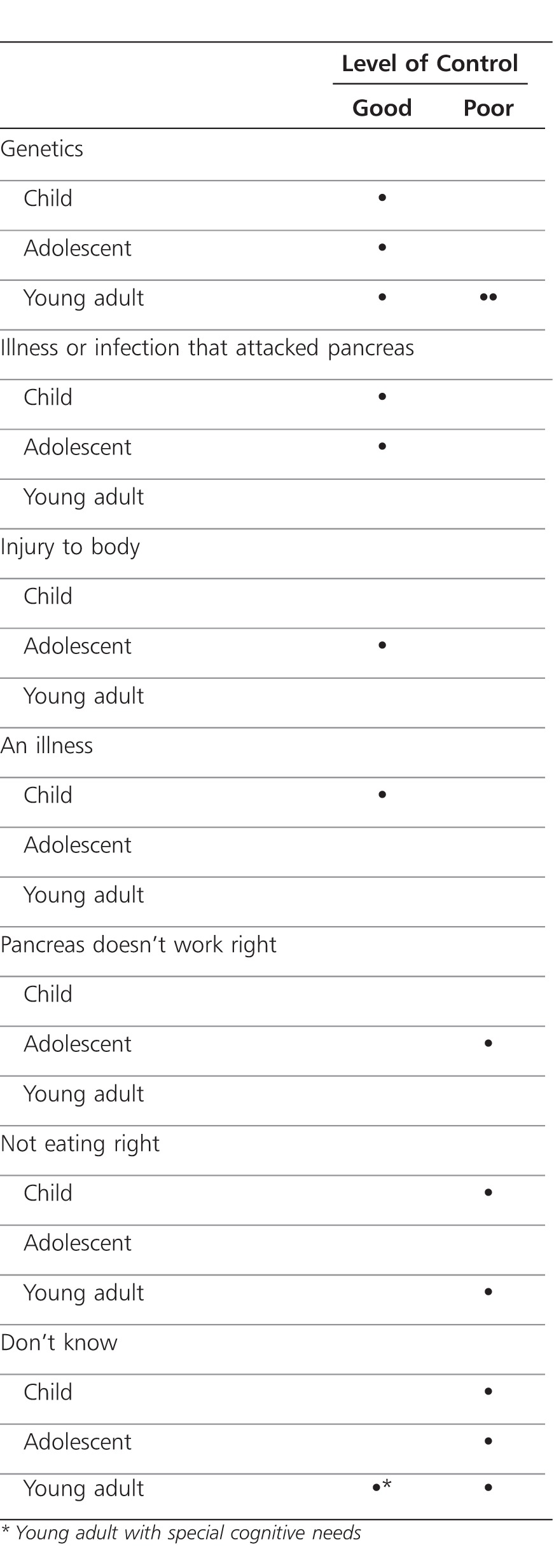
All of the children discussed cause in response to identity questions. Only children with SCD mentioned symptoms (pain). Children with T1D also discussed disease pathophysiology or disease duration. For identity, adolescents discussed disease cause, self-care actions, and pathophysiology. Youth with T1D contrasted it with type 2 diabetes. Only youth with SCD discussed symptoms, affected body parts, disease duration, and restrictions. Identity and cause discussion was more sophisticated among adolescents with better controlled disease, and the contrast was strongest among youth with T1D. For example, patient 4, who was an adolescent with well-controlled disease, noted that “T1D type 1 is hereditary … [text omitted] …. It's when your body attacks your pancreas and it stops producing insulin. You have to give yourself insulin to make your blood sugar level.” In contrast, patient 10, an adolescent with poorly controlled disease, reported that “diabetes type 1 is … ah, actually I really can't explain it.”
YAs were less verbal about disease identity than were adolescents. They discussed self-care activities and compared and contrasted their disease with similar diseases. In response to identity questions those with T1D did not mention symptoms or causality, but those with SCD did discuss the symptom of pain and its causes.
Symptoms
Type 1 Diabetes
Youth with well-controlled T1D identified and discussed a larger variety of symptoms (n=17) and discussed them more frequently than did youth with poorly controlled diabetes (n=8). Only a few youth with T1D said they thought about symptoms frequently. Adolescents and YAs with good T1D control were more likely than those with poor control to view symptoms as a cue to test blood sugar. Symptom prevention motivated some youth with good T1D control. An adolescent with poor control connected negative consequences with symptoms.
For example, patient 10, an adolescent with poorly controlled T1D, noted “Well, I think about them every day, because, I—I know that it affects me—like with my sports and stuff … .”
Sickle Cell Disease
All youth with SCD described pain and its causes, with little variation between groups. Several discussed the pain's intermittent and unpredictable nature and its interference in their lives. Interestingly, youth (n=5, 10 mentions) with good SCD control discussed sickling crisis more frequently than did youth (n=2, 4 mentions) with poor control.
Timeline
The vast majority of patients understood their condition as a lifelong one, although sometimes the hope for a cure was mentioned. A few may have conflated cure with disease improvement or needing fewer treatments.
Patient 3, an adolescent with good control of his disease, reported that “Sometime SCD disease, like, you can like grow out of it. You'll still have it, but you won't have as many outbreaks and such. And sometimes you have to live with it. But um … , I know there are cures for it now, and treatments that help you avoid outbreaks.”
Likewise, adolescent number 3, with good control of T1D, noted “there's a honeymoon stage where you don't have it, like—it could go up from, like 2 days to a month, but … I haven't gone through that yet,” and “I think it can—it can go away.”
Perceived Controllability
Controllability was mentioned by 5 youth with T1D and only 1 with SCD. Sophistication regarding controllability perceptions was high (e.g., a child with poorly controlled T1D differentiated between checking blood sugar and keeping it under control). Rebellion against adult control was also evident, as follows: Child number 1, with well-controlled T1D, said “it doesn't mean that you're not taking control of your T1D whenever you're slacking off for just 1 day. It matters but it doesn't matter as much as if you were to do it every month. Have to make sure that (word) on task, but not, you don't have to say that it's going to kill you because you did it for 1 day.”
Acceptance of responsibility for blood sugar controllability differed between adolescents with good and poor T1D control. For example, one adolescent with poor control (patient 1) relied on his parents and doctor to help him keep blood sugar concentrations under control. In contrast, notice the responsibility and problem-solving orientation in adolescent number 3 with well controlled T1D: “I haven't figured out why [my blood sugar went out of control] … [text omitted] …. I have to make sure my blood sugar is under control. I have to check it. I have to take my insulin when I'm supposed to.”
Consequences
Major categories of impact for youth, excluding symptoms, were 1) life impact, 2) physical outcomes, 3) self-care, 4) emotions, and 5) health-system activities (Table 6). Adolescents provided more detailed discussion than did either children or YAs. Youth with both T1D and SCD from all age and control categories noted that their disease interfered with their activities and lifestyle, the most frequently mentioned impact. Patient 6, with well-controlled SCD, reported “I feel bad, cause I'm kind of trapped, can't do anything … at all.”
Table 6.
Items Children, Adolescents, and Young Adults Saw as a Consequence of their Disease (Excluding Symptoms)
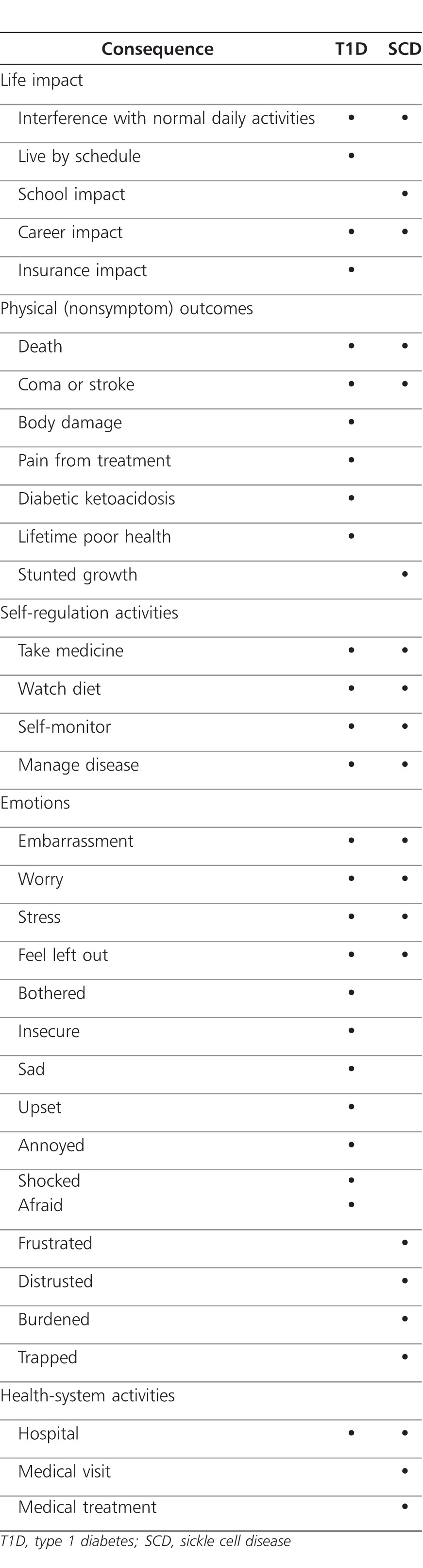
About half of the youth with T1D denied significant day-to-day T1D impact, while only 2 youth with SCD denied significant impact. Denial could not be taken at face value, though. For example, patient 1, a child with well-controlled T1D, noted “[T1D] doesn't really affect it [daily life] that much. I just kind of try to hide it. So I won't be embarrassed or anything.”
Youth in both disease groups admitted they occasionally forgot medication when socializing, despite having friends who were described as supportive and helpful. Most youth with T1D tried to keep up with friends even when they were not feeling well, while most youth with SCD did not. Children with T1D complained about taking time out from social activities to check/adjust insulin. Youth with SCD frequently discussed the negative impact of numerous health-system visits and symptoms on school/work attendance. Two youth with T1D said blood sugar problems impaired concentration at school, but not school attendance. Only youth with T1D mentioned disease impact on career choice and insurability or the importance of scheduling.
All youth described their disease as serious or very serious, with death most frequently mentioned as the worst that could happen, followed by coma (T1D) and hospitalization. Youth with T1D identified a larger number of physical consequences than did youth with SCD.
Self-care activities were also seen as a consequence by all youth, with specific activities varying by disease and age. Most youth with SCD mentioned rest, avoiding overexertion, maintaining hydration, and taking medicine as disease consequences. Youth with T1D mentioned medicine and diet, adolescents and YAs included checking blood sugars. One adolescent with poor T1D control mentioned reducing the number of shots as a positive outcome.
Emotions
Emotions were also a frequently described consequence as well as being discussed in other contexts. Youth with well-controlled diabetes mentioned emotions markedly more often than those in the other 3 groups. Youth noted that significant others felt worried and anxious about them, and some youth described a need for encouragement. Social emotions included feeling left out or embarrassed and negative feelings resulting from others' lack of understanding or impatience. For example, patient 5, a YA with well-controlled SCD, reported “most of them think that your sickle cell pain is just like a regular stomachache and it's not. [text omitted] trying to go out and do your daily things and you can't do it, and people don't understand that there is a seriousness there, and there are complications with sickle cell, but they don't understand. And people looking at it—looking at you like, you don't look like you in pain, because they don't see no … blood, they don't see nothing.”
The most prominent nonsocial emotion was worry, discussed most frequently by children and adolescents with well-controlled T1D (about symptoms or blood sugar). Worry was discussed less frequently by youth with both well- and poorly controlled SCD (about pain, getting sick, getting to a healthcare visit). Youth with T1D who discussed worry also described methods for dealing with it: understanding, checking sugars, preventive steps, and avoiding dwelling on symptoms. Two youth with poorly controlled SCD advised having a good attitude and going on with life. Only 1 youth with poorly controlled T1D mentioned worry, advising against it.
Additional nonsocial emotions were annoyance/frustration, general emotional distress (e.g., “feel bad,” “bothered”), fear, sadness, and shock. Annoyance/frustration was most frequently related to the self-care routines of youth with well-controlled T1D. Youth expressing general emotional distress most often had poor disease control (both T1D and SCD) and did not link the emotion with any positive coping strategy. The distress of youth with SCD was primarily related to feeling different from others. This was evident in child 8, with poorly controlled SCD, who said “[I] want to be a normal little person.”
Acceptance and understanding were expressed by 4 youth with well-controlled T1D and 2 with poorly controlled SCD and were generally described as a response to a negative situation. No youth with poor T1D control discussed acceptance.
Two adolescents with good T1D control attributed grumpiness, irritability, and anger to blood sugar problems, and several youth noted their belief that stress and worry could worsen disease.
An adolescent with well-controlled SCD (patient 3) noted “If you think about the symptoms a lot, you could start to stress yourself out and make yourself sick, so I don't really think about it unless I'm sick.”
DISCUSSION
Illness representations as a modifier of medication adherence have received little attention in pediatrics and may represent a novel way in which to understand and improve patient adherence and therefore disease outcomes. Adherence support is an increasingly important role for pharmacists.23,24 If pharmacists understand the underpinnings of nonadherence it will improve their ability to interact with pediatric patients with the goal of identifying and modifying maladaptive thinking.
Within the CSM framework identity has most often been operationalized as a list of symptoms related to the illness.7 Results from this study indicate that disease identity incorporates multiple CSM constructs and changes with age and/or experience. There may be a natural progression as disease knowledge increases and becomes more integrated, moving from cause through pathophysiology, differentiation from similar diseases, and self-care. Additionally, the most salient disease features appear to contribute to disease identity. Mental representations have been described as “a collection of salient features weighted in terms of their importance … .”25 For both groups, younger children are very interested in what causes the disease. Results from this study indicate that causal discussion with children between 8 and 12 years of age should remain at a simple level, but they also indicate that it is important to correct any causal misperceptions they may have at this time as they are building mental representations of the disease. Caregivers should consider increasing the sophistication of causal discussions during the adolescent years. Teens appear open to somewhat-technical discussions concerning mechanism of action and how self-care influences the disease. It is important to discuss these topics during childhood and adolescence because YAs (aged 18 years and above) look to be less interested in the topic. For youth with T1D, blood sugar concentration and self-care appear highly salient; for youth SCD symptoms and restrictions are of paramount interest. This indicates that a list of symptoms related to the illness would be appropriate for assessing youth with SCD, but a list of symptoms related to blood sugar concentrations might be more appropriate for youth with T1D.
There appeared to be greater differences between youth with well- and poorly controlled T1D than those with well- and poorly controlled SCD in regard to the symptoms mentioned. Youth in this study with well-controlled T1D discussed more symptoms more frequently than did youth with poorly controlled T1D, and in a greater variety of contexts. This is in contrast to previous literature that suggests that dwelling on symptoms may be associated with poor HbA1c control.26,27 Previous measures may have had problems, however (e.g., a generic list of symptoms that did not include diabetes symptoms such as shakiness, thirst, and increased urine). Another problem may have been that older measures had patients' rate symptom intensity, which could indicate somatization rather than identifying the symptom with the disease.7
This does raise the intriguing idea that a key difference between youth with well- and poorly controlled T1D, as defined by HbA1c control, may not be symptom focus but rather the meanings and actions they habitually connect to them. Youth with good T1D control included in this study appeared to link proactive thinking and coping strategies with symptoms, while those with poor control linked negative consequences. Youth with well-controlled T1D also discussed emotions much more extensively than did those with poorly controlled disease, often in conjunction with blood sugar testing. Emotions may be stimulated because the youth are performing self-care actions, but many also talked about accepting and dealing with these emotions. Youth with poor T1D control may avoid negative emotions they cannot or do not wish to deal with by avoiding self-care behaviors. Greater self-efficacy may be useful in reducing worry and fear about ‘highs' and ‘lows' resulting from insulin administration. Confidence in their ability to control blood sugar may help youth maintain emotional control. Cognitive-behavioral interventions may be particularly appropriate for use in conjunction with a CSM-based assessment. Both posit that the meaning attached to events influences emotional responses and behavioral choices.28,29 Pharmacists might consider acknowledging symptoms and emotions while modeling and linking appropriate action steps. A thorough discussion of symptom meaning, appropriate steps, and action rehearsals has the potential to help forge and strengthen appropriate action links. For example, many youths associate particular symptoms with blood sugar concentration changes. The pharmacist could identify the symptoms a youth associates with high or low blood sugars and discuss potential alternative symptom causes. A demonstration day or days could be planned to help patients see that their blood sugar changes even when they do not experience ‘symptoms' and that it does not always change when they do experience ‘symptoms.' Interventions for youth who see insulin use as a reminder of their disease could focus on recognizing and dealing with negative emotions and thinking, as well as shifting their view of insulin from disease reminder to tool for control.
Youth with well-controlled T1D included in this study appeared to have a better understanding of their disease pathophysiology than did youth with poor control. A similar association between control level and pathophysiology knowledge was not seen for youth with SCD. Current illness coherence measures seek to determine if the disease makes sense to the subject (eg, “My illness is a mystery to me”) but do not assess pathophysiology knowledge. Future research should assess whether illness coherence is associated with actual disease pathophysiology knowledge and understanding and should investigate the nature of that association. Illness coherence may indicate that youth understand more than basic knowledge of how the disease is caused and what the symptoms are or could include knowledge of what symptoms do or do not mean and how their actions and treatments can influence the course of the disease. Again, it may be that understanding and making the connections is a key factor. If they are not associated, separate disease-specific knowledge questions and/or cause-and-effect questions may be useful. Either way, increased focus on illness coherence and disease knowledge for youth with poorly controlled T1D may be helpful in combination with strategies for dealing with symptoms and emotions. Some youth believed that having to perform fewer self-care behaviors indicated disease improvement. This type of magical thinking may result in poor treatment adherence and long-term outcomes, as well as disappointment if the expected ‘improvement' is never achieved. Clinicians may want to ensure that youth with chronic disease realize that having to perform fewer self-care behaviors is not always a sign of disease improvement and that regular checks even when asymptomatic are important.
In this study, youth with SCD with poorly controlled disease actually discussed sickling crisis less frequently than did youth with better controlled disease, and they appeared to discuss negative emotions somewhat less frequently than did youth with T1D. This may be adaptive, since the disease is not easily controlled. Youth with SCD would likely benefit from discussion about the negative emotions and difficulties they face in dealing with society and interacting with others.
Caregivers and parents spend a great deal of time discussing the negative long-term consequences of not managing diabetes or sickle cell disease as a type of fear motivator to encourage better compliance. The absence of significant discussion on this aspect of the disease indicates that using scare tactics to improve self-care behaviors has limited effectiveness. Future studies should address this common counseling strategy directly. The further a practitioner gets from understanding his patient's perspective (particularly with children/adolescents), the less likely the practitioner will be to be able to positively influence a patient's behavior.
A limitation of this study is that we could not examine sex differences. Sex differences may be conflated with differences associated with level of disease control. As discussed in the “Participants” section above, HbA1c can be influenced by many factors. To maximize self-care differences between the youth we selected participants with values near HbA1c scale extremes. All of the participants were recruited from the same site, which limits transferability. Data about refusers were not recorded. The sample size was small; future studies with more participants could yield even richer data.
CONCLUSIONS
Overall, the CSM appears most useful for assessing relevant disease perceptions and developing interventions for youth with diseases that have effective therapies requiring active self-care. Although children do not seem ready to make sophisticated connections, ensuring that they and their families receive and understand accurate causality information appears important. It may also be useful to discuss positive connections between symptoms, adaptive self-care activities, and outcomes to help assist them in developing these links right from the start.
Adolescence may be the key time to focus discussions on symptoms, self-care, and outcomes, however, as this age group seems most interested in this type of discussion. This could be particularly important among youth with poor disease control. Future work needs to determine if there is a significant association between these types of mental links and HbA1c control and if they are causal. If this association is sustained, interventions that provide opportunities for youth to rehearse symptom-action links and potentially problematic social situations may be of benefit.
It also appears likely that socio-emotional discussion with children and adolescents with both SCD and T1D would be profitable. Youth with SCD may benefit from help with the negative emotions that seem to arise from dealing with judgmental others and multiple restrictions on activities. Youth with poorly controlled T1D may benefit from help with emotionally accepting their disease and taking responsibility for it. Youth with both well- and poorly controlled diabetes could potentially benefit from learning how to handle negative emotions associated with self-care activities as well as negative social situations.
ABBREVIATIONS
- CSM
Leventhal's common sense model
- HbA1c
glycosylated hemoglobin A1c
- SCD
sickle cell disease
- T1D
type 1 diabetes
- YA
young adult
Footnotes
DISCLOSURE Other than funds provided by the University of Georgia, the authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria.
REFERENCES
- 1.French DP, Weinman J. Current issues and new directions in psychology and health: “Assessing illness perceptions: beyond the IPQ.”. Psychol Health. 2008;;23(1):5–9. doi: 10.1080/08870440701616714. [DOI] [PubMed] [Google Scholar]
- 2.Brownlee S, Leventhal H, Leventhal EA. Chapter twelve. Regulation, self-regulation, and construction of the self in the maintenance of physical health. In: Boekarts M, Pintrich PR, Zeidner M, editors. Handbook of Self-Regulation. San Diego, CA: Academic Press;; 2000. pp. 369–416. [Google Scholar]
- 3.Leventhal H, Meyer D, Nerenz D. The common sense model of illness danger. In: Rachman S, editor. Medical Psychology. Vol 2. New York, NY: Pergamon;; 1980. pp. 7–30. [Google Scholar]
- 4.Leventhal H, Nerenz DR, Steele DJ. Illness representations and coping with health threats. In: Baum A, SE Taylor, Singer JE, editors. Handbook of Psychology and Health: Social Psychological Aspects of Health. Vol 4. Hillsdale, NJ: Erlbaum;; 1984. pp. 219–252. [Google Scholar]
- 5.Lau RR, Bernard TM, Hartman KA. Further explorations of common-sense representations of common illnesses. Health Psychol. 1989;;8(2):195–219. doi: 10.1037//0278-6133.8.2.195. [DOI] [PubMed] [Google Scholar]
- 6.Hagger MS, Orbell S. A confirmatory factor analysis of the revised Illness Perception Questionnaire (IPQ-R) in a cervical screening context. Psychol Health. 2005;;20(2):161–173. [Google Scholar]
- 7.Moss-Morris R, Weinman J, Petrie KJ, et al. The revised Illness Perception Questionnaire (IPQ-R) Psychol Health. 2002;;17(1):1–16. [Google Scholar]
- 8.Paterson J, Moss-Morris R, Butler SJ. The effect of illness experience and demographic factors on children's illness representations. Psychol Health. 1999;;14(1):117–129. [Google Scholar]
- 9.Goldman SL, Whitney-Saltiel D, Granter J, Rodin J. Children's representations of “everyday” aspects of health and illness. J Pediatr Psychol. 1991;;16(6):747–766. doi: 10.1093/jpepsy/16.6.747. [DOI] [PubMed] [Google Scholar]
- 10.National Diabetes Statistics. National Diabetes Statistics. Fact Sheet. 2007. http://diabetes.niddk.nih.gov/DM/PUBS/statistics/#allages. Accessed May 7, 2009.
- 11.Diamond Project Group. Incidence and trends of childhood type 1 diabetes worldwide 1990–1999. Diabet Med. 2006;;23(8):857–866. doi: 10.1111/j.1464-5491.2006.01925.x. [DOI] [PubMed] [Google Scholar]
- 12.Ashley-Koch A, Yang Q, Olney RS. Sickle hemoglobin (HbS) allele and sickle cell disease: a HuGE review. Am J Epidemiol. 2000;;151(9):839–845. doi: 10.1093/oxfordjournals.aje.a010288. [DOI] [PubMed] [Google Scholar]
- 13.Hankins J, Aygun B. Pharmacotherapy in sickle cell disease—state of the art and future prospects. Br J Haematol. 2009;;145(3):296–308. doi: 10.1111/j.1365-2141.2009.07602.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kinney TR, Ware RE. The adolescent with sickle cell anemia. Hematol Oncol Clin North Am. 1996;;10(6):1255–1264. doi: 10.1016/s0889-8588(05)70398-1. [DOI] [PubMed] [Google Scholar]
- 15.Hilker KA, Jordan SS, Jensen S, et al. Development of a screening instrument of adherence in pediatric sickle cell disease. Child Health Care. 2006;;35(3):235–246. [Google Scholar]
- 16.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2008;;31((suppl 1)):S12–S54. doi: 10.2337/dc08-S012. [DOI] [PubMed] [Google Scholar]
- 17.DCCT Research Group. Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr. 1994;;125(2):177–188. doi: 10.1016/s0022-3476(94)70190-3. [DOI] [PubMed] [Google Scholar]
- 18.Helgeson VS, Snyder PR, Seltman H, et al. Brief report: trajectories of glycemic control over early to middle adolescence. J Pediatr Psychol. 2010;;35(10):1161–1167. doi: 10.1093/jpepsy/jsq011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kichler JC, Kaugars AS, Ellis J, Alemzadeh R. Exploring self-management characteristics in youths with type 1 diabetes mellitus: does membership in a glycemic control category matter? Pediatr Diabetes. 2010;;11(8):536–543. doi: 10.1111/j.1399-5448.2010.00638.x. [DOI] [PubMed] [Google Scholar]
- 20.Hamilton J, Daneman D. Deteriorating diabetes control during adolescence: physiological or psychosocial? J Pediatr Endocrinol Metab. 2002;;15:115–126. doi: 10.1515/jpem.2002.15.2.115. [DOI] [PubMed] [Google Scholar]
- 21.Du Pasquier-Fediaevsky L, Chwalow AJ, Tubiana-Rufi N. Is the relationship between adherence behaviours and glycaemic control bi-directional at adolescence? A longitudinal cohort study. Diabet Med. 2005;;22(4):427–433. doi: 10.1111/j.1464-5491.2005.01429.x. [DOI] [PubMed] [Google Scholar]
- 22.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;;320(7227):114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Armour C, Bosnic-Anticevich S, Brillant M, et al. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax. 2007;;62(6):496–502. doi: 10.1136/thx.2006.064709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clifford S, Barber N, Elliott R, et al. Patient-centred advice is effective in improving adherence to medicines. Pharm World Sci. 2006;;28(3):165–170. doi: 10.1007/s11096-006-9026-6. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan S, Kaplan R. Cognition and Environment: Functioning in an Uncertain World. Ann Arbor, MI: Ulrich's;; 1983. [Google Scholar]
- 26.Griva K, Myers LB, Newman S. Illness perceptions and self efficacy beliefs in adolescents and young adults with insulin dependent diabetes mellitus. Psychol Health. 2000;;15(6):733–750. [Google Scholar]
- 27.Hagger MS, Orbell S. A meta-analytic review of the common sense model of illness representations. Psychol Health. 2003;;18(2):141–184. [Google Scholar]
- 28.Neenan M, Dryden W. Cognitive Therapy. 100 Key Points and Techniques. New York, NY: Brunner-Routledge, Taylor & Francis Group; 2004. [Google Scholar]
- 29.Hains AA, Berlin KS, Davies WH, et al. Attributions of adolescents with type 1 diabetes in social situations—relationship with expected adherence, diabetes stress, and metabolic control. Diabetes Care. 2006;;29(4):818–822. doi: 10.2337/diacare.29.04.06.dc05-1828. [DOI] [PubMed] [Google Scholar]