The choriocarcinoma syndrome is a rare and serious complication of the choriocarcinoma tumor, whose outcome relies on its early recognition.
Case Report
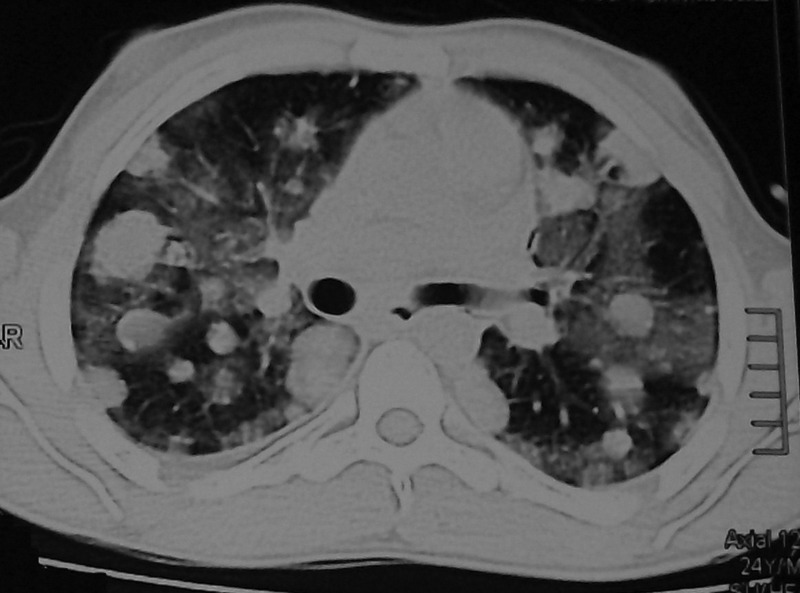
A 24-year-old male, with no medical history, noticed a gradual increase in the size of his left testicle over a period of six months. He consulted a physician because he had headaches, vomiting, fatigue, and mild dyspnea. On physical examination, he was found to be normotensive, with oxygen saturation of 99%. His relevant laboratory data were: Hematocrit 35.8%, LDH 2,345 IU/l (NV 210-420 IU/l), alfa-FP 76.7 IU/l (NV <11 IU/l), HCG >200,000 IU/l (NV <4 IU/l). Chest X-ray evidenced multiple bilateral nodules of well-defined, regular borders (Figure 1). The brain computed-tomography (CT) showed a lesion in the left occipital region with peripheral edema and midline displacement. He was diagnosed with testicular cancer and an orchiectomy was performed. Immediately afterwards, he was treated with combined chemotherapy with bleomycin, etoposide, and cisplatin. Three days later, he presented with a cough, hemoptysis, a rapidly progressive dyspnea and respiratory failure. New laboratory results showed his hematocrit had decreased to 24%. A chest CT showed zones of ground-glass opacity, mainly in the areas surrounding each pulmonary nodule (Figure 2). Bronchoscopy could not be performed because of the patient's breathing difficulty. He continued the chemotherapy treatment and showed clinical and blood-gas improvement during the following 72 hours. Finally, the case was referred to the oncology service. Afterwards, there were signs of improvement in the chest CT, along with a decrease in human chorionic gonadotropin (HCG) values.
Figure 1.
Chest X-ray showed evidence of multiple bilateral nodules of well-defined, regular borders
Figure 2.
A chest CT showed zones of ground-glass opacity, mainly in the areas surrounding each pulmonary nodule
Discussion
Testicular tumors derived from germ cells are the most common solid tumors in men between 15 and 35 years of age. Choriocarcinoma is the most aggressive variant of this group of neoplasias and is characterized serologically by the production of large amounts of HCG.
Logothetis first described the choriocarcinoma syndrome in 1984. The distinctive feature of this syndrome is bleeding at the metastatic site or sites.1–4 When the lungs are affected, the clinical case is similar to that of a diffuse alveolar hemorrhage. Even though this syndrome was first observed in patients diagnosed with choriocarcinoma and large tumor burden, cases with histological variants of seminoma have also been reported.2–6 Nevertheless, such cases showed high circulating HCG levels, which suggested the presence of choriocarcinoma component in such neoplasias. Besides testicular tumors, this syndrome has been described in germ-cell tumors associated with a trophoblastic and extratesticular disease.6–7
Although the pathogenesis of the syndrome is unknown, the damage may be triggered by chemotherapy, as the symptoms usually develop a few hours after the initiation of treatment.7 Tumor invasion of small vessels was said to be the cause of bleeding.8 The prognosis of this syndrome is very poor, particularly in patients with HCG values above 50,000 IU/l.6
The diagnosis of the syndrome is initially based on clinical suspicion. The chest radiography and CT imaging will subsequently show nodular images with irregular borders resulting from the presence of surrounding alveolar hemorrhage. The differential diagnosis should be performed with chemotherapy toxicity (e.g., bleomycin) and infections.4
Since the severity of the bleeding may threaten the patient's life, the main goals of the treatment are to ensure airway permeability and to achieve hemodynamic stability. At present, no specific therapy can be prescribed. Because of the shortness of breath, we were not able to conduct a bronchoscopy so as to confirm bleeding and at the same time discard any infections.
We think that this syndrome should be borne in mind among the physicians who monitor and treat patients for germ-cell tumors, avoiding a diagnostic delay. We hope that this case report contributes to the awareness of this complication, and therefore enables the prompt implementation of the appropriate supportive measures that could have a significant impact on patient survival.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Written consent to publish was obtained from the patient or next of kin
Guarantor
Jaime Segovia
Contributorship
All authors reviewed the literature and the manuscript
Acknowledgements
None
Reviewer
Simon Taggart
References
- 1.Logothetis CJ. Choriocarcinoma síndrome. Cancer Bull 1984;36:118–20 [Google Scholar]
- 2.Kawai K, Takaoka E, Naoi M, et al. A case of metastatic testicular cancer complicated by tumour lysis syndrome and choriocarcinoma syndrome. Jpn J Clin Oncol 2006;36:665–7 [DOI] [PubMed] [Google Scholar]
- 3.Lal A, Singhal M, Kumar S, Bag S, Singh SK, Khandelwal N. Bilateral renal and jejunal metastasis of choriocarcinoma presenting as spontaneous renal hemorrhage. Cancer Imaging 2009;9:56–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benditt JO, Farber HW, Wright J, Karnad AB. Pulmonary hemorrhage with diffuse alveolar infiltrates in men with high-volume choriocarcinoma. Ann Intern Med 1988;109:674–5 [DOI] [PubMed] [Google Scholar]
- 5.Venkatram S, Muppuri S, Niazi M, Fuentes GD. A 24-year-old pregnant patient with diffuse alveolar hemorrhage. Chest 2010;138:220–3 [DOI] [PubMed] [Google Scholar]
- 6.Durieu I, Berger N, Loire R, Gamondes JP, Guillaud PH, Cordier JF. Contralateral haemorrhagic pulmonary metastases (‘choriocarcinoma syndrome’) after pneumonectomy for primary pulmonary choriocarcinoma. Thorax 1994;49:523–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kandori S, Kawai K, Fukuhara Y, et al. A case of metastatic testicular cancer complicated by pulmonary hemorrhage due to choriocarcinoma syndrome. Int J Clin Oncol 2010;15:611–4 [DOI] [PubMed] [Google Scholar]
- 8.Shintaku M, Hwang MH, Amitani R. Primary choriocarcinoma of the lung manifesting as diffuse alveolar hemorrhage. Arch Pathol Lab Med 2006;130:540–3 [DOI] [PubMed] [Google Scholar]