Abstract
Background
Coronary artery fistula (CAF) is a rare anomaly. Transcatheter CAF closure has been introduced using various materials, but only few data are available on the Guglielmi detachable coil (GDC). The advantage of using GDC for transcatheter CAF closure is more controllable, therefore much safer when compared to other coils. This report is about our experience in transcatheter closure of CAF using fibered GDC in our hospital.
Methods & Results
From 2002 to 2007, there were 10 patients with CAFs (age range: 28 to 56 year-old, 7 males) who underwent transcatheter CAF closure. There were a total of 19 CAFs which originated from right coronary (n = 5), left circumflex (n = 3), left anterior descending artery (n = 10) and left main trunk (n = 1). Median number of coil deployment for each fistula was 3 (range: 1 to 6). The pulmonary artery was the most common site of the distal communication of CAFs (n = 14), followed by right atrium (n = 3), left atrium (n = 1) and left ventricle (n = 1). Immediate coronary angiography after GDC deployment revealed no residual shunt in 12 (63.2%) CAFs, significant reduction of the flow in 5 (26.3%), while 2 (10.5%) could not be closed due to small size. Nine (90%) patients underwent a repeated angiography within 3 to 8 months. Among 12 CAFs that were occluded immediately post-deployment, there were 2 CAFs with insignificant residual flow. Among 6 CAFs with significantly decreased flow immediately post-deployment, 2 were occluded totally in the follow-up angiography. In total, 12 (70.5%) CAFs were occluded completely and 5 (29.5%) CAFs still had insignificant residual flow, which did not need any additional coil deployment. During a mean follow up of 4.3 ± 0.7 year, all patients remained symptom and complication free.
Conclusions
The fibered GDC is a safe and effective method for percutaneous closure of the CAFs.
Keywords: Coronary artery fistula, Transcatheter closure, Guglielmi detachable coil
1. Introduction
Coronary artery fistula (CAF) is a rare anomaly. It consists of abnormal communication between coronary artery and one of the cardiac chambers or vessels adjacent to the heart. CAFs were present in 0.002% of the general population and were visualized in nearly 0.25% of patients undergoing catheterization.[1]–[3] Their clinical importance was usually seen in the period of adulthood, due to an increased risk of complications, including heart failure, myocardial ischemia, infective endocarditis, arrhythmias, and rupture.[4]–[6]
Surgery and direct epicardial ligation were traditionally viewed as the main therapeutic methods for the closure of CAFs.[7] Surgical correction is safe and effective, with good results.[8]–[13] However, treatment of asymptomatic adult patients with non-significant shunting was still a matter of debate. Transcatheter closure of CAFs is a non-surgical treatment option. Since its introduction in early 1980s,[14] transcatheter closure of CAF is now widely available and has been recognized for nearly a decade as an effective and safe approach and provides good outcome. There are a variety of devices being used for the closure including coils, vascular plug, covered stent, and detachable balloon.[15]–[26] The Guglielmi detachable coil (GDC) (Boston Scientific/Target Therapeutics, Boston, Mass, USA) is a platinum coil commonly used in intracranial occlusion of brain aneurysm.[27],[28] Only few data are available on the use of GDC for CAF closure.[29] Fibered GDC has robust thrombogenic properties and therefore presents a better alternative for closing the fistula. GDC provides an additional advantage over the other coils due to the ability to reposition or even remove the coil when it was not in proper position, which would minimize the risk of coil migration. This study reported our experience of using these coils in the treatment of CAF and the mid-term follow-up.
2. Methods
2.1. Patient population
Consecutive patients diagnosed with CAF who underwent transcatheter closure using fibered GDC were included in this study. Patient baseline characteristics, hemodynamic and angiographic data, and clinical status were collected from the patient's medical records. All patients were diagnosed incidentally to have CAF during coronary angiogram. Informed and written consent were obtained from all patients. Clopidogrel 75 mg (O.D.) was given for 3 days prior to procedure and was continued for at least one month. Aspirin 160 mg (O.D.) was given for at least 6 months after the procedure. During the procedure, heparin was given intravenously at 100 units per kilogram bodyweight. CK-MB and troponin T were not obtained routinely unless myocardial injury was suspected.
2.2. Cardiac catheterization
The procedure was done to all patients in fasting state and mild sedation. Percutaneous access by the Seldinger technique was obtained from both the right femoral vein and artery. After collection and analysis of hemodynamic data, anatomy and dimensions of the coronary arteries, the CAFs were determined using selective coronary angiograms. Hand injection of contrast facilitated catheter positioning in the distal CAF. Determination of the orificium of the CAF was done by multiple views. Terminology of the CAF was used according to the Dutch Registry i.e., its origin, pathway and termination.[30]
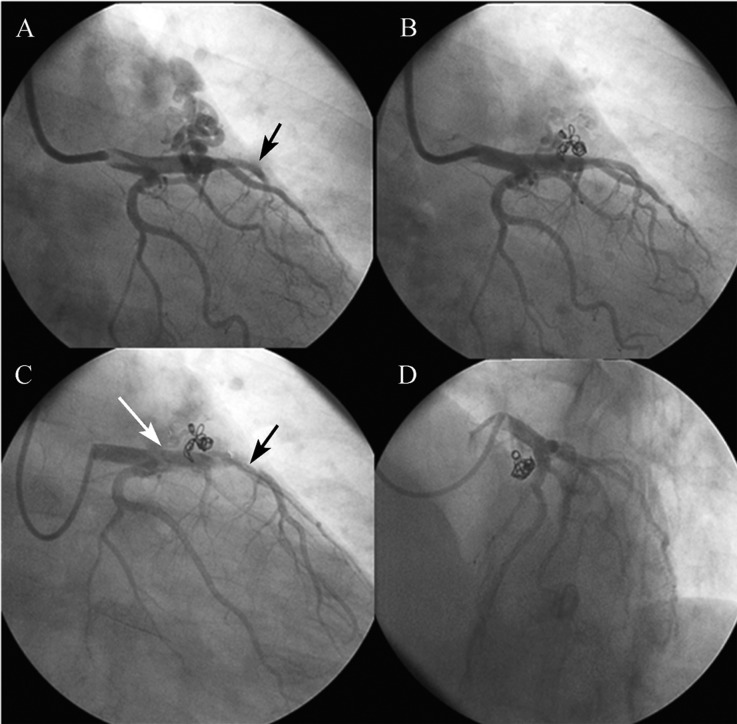
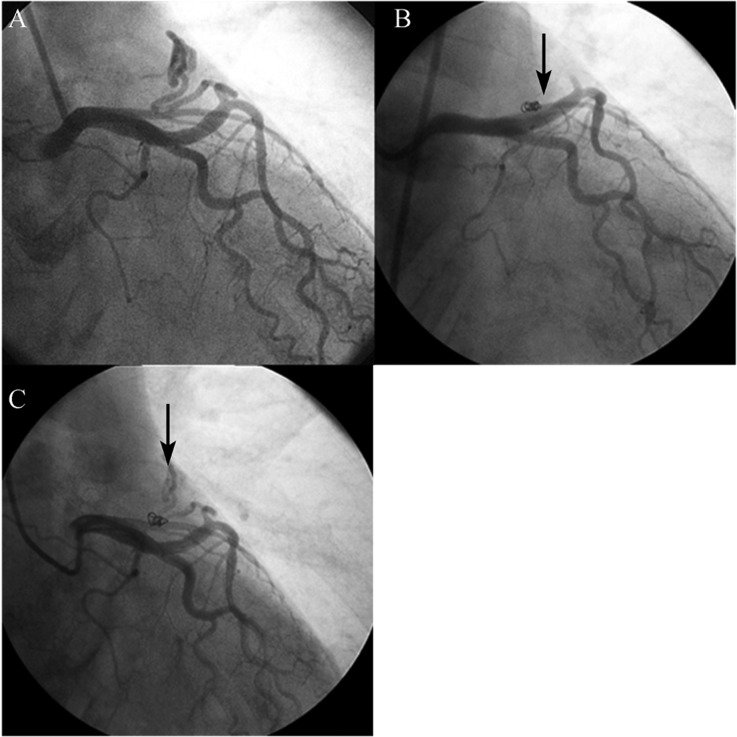
We used fibered GDC as the occlusive device. A 2.0 F microcatheter, either Progreat 2.0 (Terumo, Tokyo, Japan) or Excesior 1018 (Boston Scientific, Natick, MA, USA) that could accommodate 0.014 inch wires or GDC was used. After determining the orificium of CAF, the microcatheter was then introduced through guiding catheter over 0.014 inch hydrophilic coronary guidewire (Radiofocus, Guidewire M, Terumo, Tokyo, Japan) until it was selectively positioned within the CAF. The tip of the microcatheter was placed at least 1 to 2 cm away from its orificium of the CAF to avoid embolization of the coil into the distal coronary artery. The GDC coil was deployed into the fistula through the microcatheter. After the coil was considered in a proper position within the fistula (Figure 1 and 2), then it was detached. If the blood flow within the fistula remained high, an additional coil was inserted. Repeat angiography was performed after removal of the microcatheter. The patient was discharged on the second day after the procedure. Repeat angiography was scheduled to be performed in 3 to 6 months following the procedure in order to evaluate the flow within the fistula. Clinical follow-up was performed by regular visits on a yearly basis.
Figure 1. Transcatheter closure of LAD fistula using Guglielmi detachable coil in a patient with no symptoms. (A): Before coiling; (B): After 2 GDCs deployment, there was still insignificant flow in the fistula; (C): Four months after coiling. The flow from another fistula (from LCX, white arrow) was seen, but the fistula originated from LAD was totally occluded. The distal LAD became larger (black arrow) due to lack of stealing phenomenon. (D): LAO cranial position, the fistula originated from LAD was clearly seen and was totally occluded. GDCs: Guglielmi detachable coil; LCX: left circumflex; LAD: left anterior descending; LAO: left anterior oblique.
Figure 2. Transcatheter closure of LAD fistula using Guglielmi detachable coil in a 54-year-old man with shortness of breath and positive treadmill test. (A): AV fistula from mid LAD to PA; (B): Just after 1 coil deployment, the flow was absent (black arrow); (C): Three months after coil deployment, an insignificant flow reappeared at the CAF (black arrow). AV: Arteriovenous; LAD: left anterior descending; PA: pulmonary artery.
2.3. Statistical analysis
The statistical analysis was performed using SPSS version 17 software (SPSS Inc, Chicago, Illinois). Continuous variables were expressed as the mean ± SD and categorical variables as proportions (%).
3. Results
This study consisted of 10 patients (age range: 28∼56 years, 70% male) with CAFs who underwent transcatheter closure during the periods of 2002 to 2007. There were 3 patients with symptoms of angina pectoris, 1 patient complained of shortness of breath, the rest were asymptomatic. Resting electrocardiogram (ECG) and echocardiogram of all patients were normal. All of the patients had a positive treadmill test, but no structural heart diseases were detected. Two cases were associated with significant coronary artery disease and underwent coronary stenting in addition to CAF closure. The baseline characteristics of the patients are presented in Table 1. The detailed fistula type, coils used and outcome in patients are listed in Table 2. After the procedure, all patients had no ECG changes or symptoms suggesting myocardial injury. Therefore, we did not perform echocardiogram or obtain CK-MB or troponin T level following the procedure.
Table 1. Patient characteristics.
| Patient | Sex | Age (years) | Sign | Symptoms | Associate lesion |
| EN | F | 52 | Nil | Nil | Nil |
| ZAE | M | 48 | Murmur | Angina | Significant LAD stenosis |
| SAM | M | 41 | Nil | Angina | Significant LAD stenosis |
| TON | M | 54 | Nil | SoB | Nil |
| PUD | M | 28 | Nil | Nil | Nil |
| HW | M | 51 | Nil | Nil | Nil |
| LUH | M | 49 | Nil | Nil | Nil |
| MAD | F | 35 | Nil | Angina | Insignificant LAD stenosis |
| SYA | M | 36 | Nil | Nil | Nil |
| RAB | F | 56 | Nil | Nil | Nil |
F: female; M: male; LAD: left anterior descending artery; SoB: shortness of breath.
Table 2. Details of fistula type, coils used and outcome in patients undergoing CAF closure.
| Patient | Fistula type | Fistula size (mm) | No. of coils used | Outcome |
| EN | LAD to PA | 3 | 2 | Totally occluded |
| ZAE | LAD to PA | 4 | 3 | Totally occluded |
| LAD to PA | 2 | 1 | Totally occluded | |
| SAM | LAD to PA | 4 | 3 | Insignificant flow |
| TON | LAD to PA | 3 | 1 | Totally occluded |
| PUD | RCA to PA | 3 | 2 | Totally occluded |
| RCA to RA | 2 | 1 | Totally occluded | |
| HW | LM to PA | 2 | 1 | Totally occluded |
| LAD to PA | 3 | 2 | Insignificant flow | |
| RCA to RA | 3 | 2 | Totally occluded | |
| LUH | LAD to PA | 4 | 3 | Totally occluded |
| LCX to LA | 1 | - | Cannot be closed due to small CAF | |
| MAD | LAD to PA | 3 | 1 | Insignificant flow |
| SYA | LAD to PA | 4 | 3 | Totally occluded |
| LCX to LV | 6 | 3 | Totally occluded | |
| RCA to RA | 3 | 2 | Insignificant flow | |
| RAB | LAD to PA | 3 | 2 | Insignificant flow |
| LCX to PA | 1 | - | Cannot be closed due to small CAF | |
| RCA to RA | 8 | 3 | Totally occluded |
CAF: coronary artery fistula; LAD: left anterior descending; LCX: left circumflex; RCA: right coronary artery; LM: left main; PA: pulmonary artery.
Nineteen CAFs were detected during the cardiac catheterization. They consisted of 16 unilateral, 1 bilateral and 3 multilateral communications. The proximal sites of communication were originated from left anterior descending artery (n = 10), right coronary artery (n = 5), left circumflex artery (n = 3) and left main trunk (n = 1). The pulmonary artery (n = 13) was the most common site of distal communication of the CAFs, followed by the right atrium (n = 3), left atrium (n = 1), and left ventricle (n = 1). The mean CAF size was 3.3 ± 1.6 mm (range: 1 to 8 mm). All patients underwent transcatheter closure using fibered GDC. All coil deployments were performed retrogradely (via the femoral artery). Median number of fibered GDCs was 3 (range: 1 to 6). The mean procedure time was 45 ± 19 min (range: 34 to 73 min). The mean fluoroscopy time was 12 ± 6 min (range: 8∼19 min). Coronary angiography immediately after GDC deployment revealed no residual shunt in 12 (63.2%) CAFs, in 5 (26.3%) had significant decrease in the flow, while in 2 (10.5%) CAFs could not be closed due to small sizes. Nine patients (90%) underwent repeat angiograms within 3 to 8 months (mean: 4.3 ± 0.9 months) after the CAF closure procedure. Among 12 CAFs that occluded immediately following the first procedure, there were 2 CAFs with an insignificant residual flow within the fistula (Figure 2). Among 6 CAFs that had significantly decreased flow immediately post-deployment, there were 2 CAFs occluded totally during the follow-up angiography. Therefore, the total number of CAFs completely occluded was 12 (70.5%) and the remaining 5 (29.5%) CAFs had an insignificant residual flow. No additional coils were added in the patients during repeat angiography follow-up. After a mean follow up of 4.3 ± 0.7 year, all patients remained symptom and complication free.
4. Discussion
The first case of transcatheter embolization therapy was performed in 1960 by Luessenhop et al.[31] They reported a 47-year-old woman with cerebral arteriovenous malformation and was treated by injecting spherical plastic emboli into the carotid artery. Since then, numerous devices and materials have been used to occlude vascular structure in various clinical settings.[32] Reidy at al.[14] reported the first successful transcatheter closure of congenital CAF in 1983. Subsequently, many authors have demonstrated the feasibility of transcatheter occlusion of CAF using different devices and materials.[15]–[26] However, all of the reports were limited in patient numbers and follow-up data. The largest series was reported by Armsby at al.[15] on 35 cases over twelve years with transcatheter closures of CAF using coils in 28 patients, umbrella devices in 6 patients and the Grifka vascular occlusion device in 1 patient. Post-deployment angiograms demonstrated complete occlusion in 19 cases, traces in 11 cases, and small residual flow in 5 cases. Follow-up echocardiograms (median: 2.8 years) in 27 patients showed no flow in 22 and small residual flow in 5. Of the 6 patients without imaging follow-up, immediate post-deployment angiograms showed complete occlusion in 5 patients and small residual flow in 1 patient. Thus, complete occlusion was accomplished in 27 (82%) patients. Early complications included transient ST-T wave changes in 5 patients, transient arrhythmias in 4 patients and single instances of distal coronary artery spasm, fistula dissection and unretrieved coil embolization. There were neither deaths nor long-term morbidity. Perry at al.[33] reported transcatheter CAF closure on nine patients. There were three CAFs from the LCX artery to the coronary sinus, three from the LAD to the right ventricular apex, two from the RCA to the superior vena cava/right atrial junction and one CAF from the LCX to the pulmonary artery. The CAFs was closed with Gianturco coils in six patients, a double-umbrella device in two and a combination of an umbrella and coils in one patient. All CAFs were completely occluded. Complications consisted of migration of two coils, one of which was retrieved, and a transient junctional tachycardia in one patient. In three patients with multiple CAFs, transcatheter occlusion was not attempted.[33]
To the best of our knowledge, there has been only one report of transcatheter closure of CAF using GDCs by Tacoy et al.[29] In their report of a 35-year-old man complained of chest pain who had severe tortuous fistula arising from distal LCX, the CAF was completely closed by multiple insertion of GDCs. The GDC system consists of a soft platinum coil soldered to a stainless steel delivery wire. When the GDC is in proper position within CAF, a 1 mA current is applied to the delivery wire. The electric current dissolved the stainless steel delivery wire proximal to the platinum coil by means of electrolysis. Therefore, using this device would avoid coil migration and embolization.[34],[35] Large clinical trials showed the safety and efficacy of GDCs in endovascular treatment.[36] In our case, we used GDCs not only because it is easy to perform, but due to the controllable coil manipulation which could prevent coil embolization and minimize complications.
Transcatheter closure of CAF is relatively safe, but death has been reported.[37] Armsby et al.[15] reported a very low rate of complications. Among 35 cases, there were 5 patients with early complications including transient ST-T wave changes, 4 patients developed transient arrhythmias, 1 patient had a distal coronary artery spasm, 1 patient developed fistula dissection and 1 patient experienced unretrieved coil embolization. There were neither deaths nor long-term morbidity in their study.[15] In our case series, all patients were free from symptoms and complications during follow-up.
The most important factor in this procedure is to choose the coil size, which exceeded the diameter of the CAFs by at least 30%, in order to prevent coil repositioning or migration. The limitation of this coil is its relatively more expensive when compared to other coils. In our series, we did not have a case of giant fistula, which has been reported in other studies.[38],[39] However, if such a case was encountered, a number of coils may be required, or we might use another closure device, such as a vascular plug (Aga Medical Corp., Minneapolis, USA). This device should be used for large CAFs and its orificium should be at close proximity to the ostium of the coronary artery, because of the stiffness of its delivery cable. The tip of the guiding catheter for delivering the vascular plug should be placed around 0.5 to 1 cm from the orificium at the proximal of the fistula. If the orificium of the fistula is quite far from the ostium of the coronary artery, the delivery cable could result in injury of the coronary artery. The delivery catheter should also engage 1 to 2 cm within proximal of the fistula. The stiffness of the cable could also cause difficulty to manipulate.
In conclusion, transcatheter coil embolization using fibered GDC coil in selected patient with CAF is safe and effective.
4.1. Study limitations
This study is a case series of transcatheter closure of CAF and is done retrospectively. Therefore, it will not represent the non-surgical treatment of all CAF cases and not included those having a large CAF. A prospective and multicenter study or registry on transcatheter closure of CAF using this device may be needed.
References
- 1.Fernandes ED, Kadivar H, Hallman GL, et al. Congenital malformations of the coronary arteries: the Texas Heart Institute experience. Ann Thorac Surg. 1992;54:732–740. doi: 10.1016/0003-4975(92)91019-6. [DOI] [PubMed] [Google Scholar]
- 2.Olearchyk AS, Runk DM, Alavi M, et al. Congenital bilateral coronary-to-pulmonary artery fistulas. Ann Thorac Surg. 1997;64:233–235. doi: 10.1016/s0003-4975(97)00347-0. [DOI] [PubMed] [Google Scholar]
- 3.Urrutia SC, Falaschi G, Ott DA, et al. Surgical management of 56 patients with congenital coronary artery fistulas. Ann Thorac Surg. 1983;35:300–307. doi: 10.1016/s0003-4975(10)61563-9. [DOI] [PubMed] [Google Scholar]
- 4.Vizzardi E, D'Aloia A, Zanini G, et al. Coronary artery fistula: diagnostic role of transthoracic and transesophageal echocardiography. Minerva Cardioangiol. 2008;56:361–364. [PubMed] [Google Scholar]
- 5.Umezu K, Hanayama N, Toyama A, et al. Successful repair for a giant coronary artery aneurysm with coronary arteriovenous fistula complicated by both right- and left-sided infective endocarditis. Gen Thorac Cardiovasc Surg. 2009;57:544–546. doi: 10.1007/s11748-009-0430-4. [DOI] [PubMed] [Google Scholar]
- 6.Vitarelli A, De Curtis G, Conde Y, et al. Assessment of congenital coronary artery fistulas by transesophageal color Doppler echocardiography. Am J Med. 2002;113:127–133. doi: 10.1016/s0002-9343(02)01157-9. [DOI] [PubMed] [Google Scholar]
- 7.Mavroudis C, Backer CL, Rocchini AP, et al. Coronary artery fistulas in infants and children: a surgical review and discussion of coil embolization. Ann Thorac Surg. 1997;63:1235–1242. doi: 10.1016/s0003-4975(97)00251-8. [DOI] [PubMed] [Google Scholar]
- 8.Balanescu S, Sangiorgi G, Castelvecchio S, et al. Coronary artery fistulas: clinical consequences and methods of closure. A literature review. Ital Heart J. 2001;2:669–676. [PubMed] [Google Scholar]
- 9.Wang S, Wu Q, Hu S, et al. Surgical treatment of 52 patients with congenital coronary artery fistulas. Chin Med J (Engl) 2001;114:752–755. [PubMed] [Google Scholar]
- 10.Rittenhouse EA, Doty DB, Ehrenhaft JL. Congenital coronary artery- cardiac chamber fistula. Review of operative management. Ann Thorac Surg. 1975;20:468–485. doi: 10.1016/s0003-4975(10)64245-2. [DOI] [PubMed] [Google Scholar]
- 11.Mawatari T, Koshino T, Morishita K, et al. Successful surgical treatment of giant coronary artery aneurysm with fistula. Ann Thorac Surg. 2000;70:1394–1397. doi: 10.1016/s0003-4975(00)01762-8. [DOI] [PubMed] [Google Scholar]
- 12.Lowe JE, Oldham HN., Jr Sabiston DC, Jr. Surgical management of congenital coronary artery fistulas. Ann Surg. 1981;194:373–380. doi: 10.1097/00000658-198110000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kamiya H, Yasuda T, Nagamine H, et al. Surgical treatment of congenital coronary artery fistulas: 27 years' experience and a review of the literature. J Card Surg. 2002;17:173–177. doi: 10.1111/j.1540-8191.2002.tb01195.x. [DOI] [PubMed] [Google Scholar]
- 14.Reidy JF, Sowton E, Ross DN. Transcatheter occlusion of coronary to bronchial anastomosis by detachable balloon combined with coronary angioplasty at same procedure. Br Heart J. 1983;49:284–287. doi: 10.1136/hrt.49.3.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armsby LR, Keane JF, Sherwood MC, et al. Management of coronary artery fistulae. Patient selection and results of transcatheter closure. J Am Coll Cardiol. 2002;39:1026–1032. doi: 10.1016/s0735-1097(02)01742-4. [DOI] [PubMed] [Google Scholar]
- 16.Sim JY, Alejos JC, Moore JW. Techniques and applications of transcatheter embolization procedures in pediatric cardiology. J Interv Cardiol. 2003;16:425–448. doi: 10.1046/j.1540-8183.2003.01009.x. [DOI] [PubMed] [Google Scholar]
- 17.Kamineni R, Butman SM, Rockow JP, et al. An unusual case of an accessory coronary artery to pulmonary artery fistula: successful closure with transcatheter coil embolization. J Interv Cardiol. 2004;17:59–63. doi: 10.1111/j.1540-8183.2004.01711.x. [DOI] [PubMed] [Google Scholar]
- 18.Trehan VK, Arora R, Mukhopadhyay S, et al. Percutaneous closure of coronary pulmonary arterial fistula using catheterization laboratory trash. Catheter Cardiovasc Interv. 2003;59:49–51. doi: 10.1002/ccd.10469. [DOI] [PubMed] [Google Scholar]
- 19.Justo RN, Slaughter RE, Whight CM, et al. Transcatheter embolisation of coronary artery fistulae. Heart Lung Circ. 2001;10:53–57. doi: 10.1046/j.1444-2892.2001.00081.x. [DOI] [PubMed] [Google Scholar]
- 20.Bonello L, Com O, Gaubert JY, et al. Covered stent for closure of symptomatic plexus-like coronary fistula. Int J Cardiol. 2006;109:408–410. doi: 10.1016/j.ijcard.2005.05.041. [DOI] [PubMed] [Google Scholar]
- 21.Thomson L, Webster M, Wilson N. Transcatheter closure of a large coronary artery fistula with the Amplatzer duct occluder. Catheter Cardiovasc Interv. 1999;48:188–190. doi: 10.1002/(sici)1522-726x(199910)48:2<188::aid-ccd13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 22.Behera SK, Danon S, Levi DS, et al. Transcatheter closure of coronary artery fistulae using the Amplatzer duct occluder. Catheter Cardiovasc Interv. 2006;68:242–248. doi: 10.1002/ccd.20811. [DOI] [PubMed] [Google Scholar]
- 23.Subramanyan R, Agrawal A, Abhyankar A. Transcatheter closure of a large coronary artery fistula with Amplatzer duct occluder: a new approach. Indian Heart J. 2001;53:493–495. [PubMed] [Google Scholar]
- 24.Ozasa H, Kamiya I, Haneda N. Successful percutaneous closure of a coronary artery fistula with a detachable balloon. Acta Paediatr Jpn. 1996;38:160–163. doi: 10.1111/j.1442-200x.1996.tb03461.x. [DOI] [PubMed] [Google Scholar]
- 25.Hartog JM, van den Brand M, Pieterman H, et al. Closure of a coronary cameral fistula following endomyocardial biopsies in a cardiac transplant patient with a detachable balloon. Cathet Cardiovasc Diagn. 1993;30:156–159. doi: 10.1002/ccd.1810300215. [DOI] [PubMed] [Google Scholar]
- 26.Krabill KA, Hunter DW. Transcatheter closure of congenital coronary arterial fistula with a detachable balloon. Pediatr Cardiol. 1993;14:176–178. doi: 10.1007/BF00795650. [DOI] [PubMed] [Google Scholar]
- 27.Vinuela F, Duckwiler G, Mawad M. Guglielmi detachable coil embolization of acute intracranial aneurysm: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg. 1997;86:475–482. doi: 10.3171/jns.1997.86.3.0475. [DOI] [PubMed] [Google Scholar]
- 28.Friedman JA, Nichols DA, Meyer FB, et al. Guglielmi detachable coil treatment of ruptured saccular cerebral aneurysms: retrospective review of a 10-year single-center experience. AJNR Am J Neuroradiol. 2003;24:526–533. [PMC free article] [PubMed] [Google Scholar]
- 29.Tacoy G, Ebinc H, Onal B, et al. Congenitally severe tortuous circumflex artery fistula draining into the coronary sinus: Transcatheter closure with Guglielmi detachable coils via different delivery system. J Cardiol. 2009;54:317–321. doi: 10.1016/j.jjcc.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 30.Said SA, van der Werf T. Dutch survey of coronary artery fistulas in adults: congenital solitary fistulas. Int J Cardiol. 2006;106:323–332. doi: 10.1016/j.ijcard.2005.01.047. [DOI] [PubMed] [Google Scholar]
- 31.Luessenhop AJ, Spence WT. Artificial embolization of cerebral arteries. Report of use in a case of arteriovenous malformation. J Am Med Assoc. 1960;172:1153–1155. doi: 10.1001/jama.1960.63020110001009. [DOI] [PubMed] [Google Scholar]
- 32.Drooz AT, Lewis CA, Allen TE, et al. Quality improvement guidelines for percutaneous transcatheter embolization. SCVIR Standards of Practice Committee. Society of Cardiovascular & Interventional Radiology. J Vasc Interv Radiol. 1997;8:889–895. doi: 10.1016/s1051-0443(97)70679-1. [DOI] [PubMed] [Google Scholar]
- 33.Perry SB, Rome J, Keane JF, et al. Transcatheter closure of coronary artery fistulas. J Am Coll Cardiol. 1992;20:205–209. doi: 10.1016/0735-1097(92)90160-o. [DOI] [PubMed] [Google Scholar]
- 34.Sato Y, Ogino H, Hara M, et al. Embolization of collateral vessels using mechanically detachable coils in young children with congenital heart disease. Cardiovasc Intervent Radiol. 2003;26:528–533. doi: 10.1007/s00270-003-2723-9. [DOI] [PubMed] [Google Scholar]
- 35.Naber CK, Doerfler A, Churzidze S, et al. Percutaneous coil embolization of a large, congenital coronary-pulmonary fistula using hydrophilic-coated detachable platinum coils. Herz. 2004;29:218–219. doi: 10.1007/s00059-004-2566-4. [DOI] [PubMed] [Google Scholar]
- 36.Eskridge JM, Song JK. Endovascular embolization of 150 basilar tip aneurysms with Guglielmi detachable coils: results of the Food and Drug Administration multicenter clinical trial. J Neurosurg. 1998;89:81–86. doi: 10.3171/jns.1998.89.1.0081. [DOI] [PubMed] [Google Scholar]
- 37.Dorros G, Thota V, Ramireddy K, et al. Catheter-based techniques for closure of coronary fistulae. Catheter Cardiovasc Interv. 1999;46:143–150. doi: 10.1002/(SICI)1522-726X(199902)46:2<143::AID-CCD6>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 38.Olivotti L, Moshiri S, Santoro G, et al. Percutaneous closure of a giant coronary arteriovenous fistula using free embolization coils in an adult patient. J Cardiovasc Med (Hagerstown) 2008;9:733–736. doi: 10.2459/JCM.0b013e3282f2d90d. [DOI] [PubMed] [Google Scholar]
- 39.Zhou T, Shen XQ, Fang ZF, et al. Transcatheter closure of a giant coronary artery fistula with patent duct occluder. Chin Med J (Engl) 2006;119:779–781. [PubMed] [Google Scholar]