Abstract
Purpose:
Biceps tenotomy and tenodesis are effective treatment options for biceps pathology, but outcomes of revision surgery are not known. This study examines the clinical outcomes of patients who have undergone a revision biceps tenodesis.
Materials and Methods:
A retrospective review of all patients since 2004 (N = 21) who had undergone a revision biceps tenodesis with greater than 6-month follow-up was completed. A follow-up survey was carried out, and the visual analog scale (VAS), Single Assessment Numeric Evaluation (SANE), Simple Shoulder Test (SST), American Shoulder and Elbow Surgeons (ASES), and University of California – Los Angeles (UCLA) scores were obtained, along with SF-12 Mental (MCS-12) and Physical Component Summaries (PCS-12).
Results:
Indications for revision surgery were continued pain (14) and ruptured biceps (7). Complete follow-up examinations were performed in 15 of 21 patients (71.4%). Average follow-up was 33.4 ± 23.5 months. The mean postoperative scores were 1.9 out of 10, VAS; 79 out of 100, SANE; 10.2 out of 12, SST; 83 out of 100, ASES; 29 out of 35, UCLA; 44, PCS- 12; and 47.1, MCS- 12. Five patients were considered failures with a UCLA score below 27. Seventeen of twenty-one patient underwent concomitant procedures. Complete preoperative and postoperative data were collected for 14 patients. All scores demonstrated highly significant improvement from preoperative levels (P < 0.005), except for the MCS-12. There was no statistically significant difference in the outcomes of revision due to rupture and revision due to persistent pain.
Conclusions:
The results suggest that revision subpectoral biceps tenodesis provides significant pain relief and improvement in functional outcomes at a mean follow-up of 33.4 months.
Level of Evidence:
Case Series, Level 4.
Keywords: Biceps tendinitis, biceps tenodesis, clinical outcomes, revision surgery, subpectoral
INTRODUCTION
The long head of the biceps (LHB) tendon has long been recognized as a source of significant pain in the shoulder. Identification of LHB pathology may be difficult to diagnose as it is often accompanied by other shoulder pathologies such as impingement, rotator cuff tears, labral tears, and glenohumeral arthritis.[1–6] Current surgical techniques used to address bicipital tendinitis, tear, or subluxation after conservative management has failed include biceps tenotomy and various biceps tenodesis procedures.[7–9] Overall, excellent clinical outcomes have been reported with both tenodesis and tenotomy, although a small percentage of patients have persistent or recurrent bicipital problems.[4,8,10–18] The literature remains sparse on the surgical outcomes of revision procedures for this difficult patient population. The purpose of this article is to report on clinical outcomes after revision biceps tenodesis. We hypothesize that patients undergoing revision biceps tenodesis will have significant improvement in subjective clinical outcome measures from pre-operative levels.
MATERIALS AND METHODS
A retrospective record review was conducted to identify patients who had undergone a revision biceps tenodesis since 2004 by the senior author (AAR). Patients were excluded if they had surgery less than 6 months ago. The study pproved by the Rush University Institutional Review Board. A total of 21 patients were identified, of whom all had undergone open subpectoral biceps tenodesis. Twenty (95%) patients had previously undergone biceps tenodesis, and 1 (5%) patient had undergone a previous biceps tenotomy. Of the 20 patients who underwent previous tenodesis, 12 underwent a proximal (suprapectoral) biceps tenodesis (60%) and 8 underwent an open subpectoral tenodesis (40%). Operative reports from the index biceps procedure were reviewed if available. All eight index subpectoral tenodesis procedures were performed at our institution, and seven of these were performed using the interference screw technique described later. In the other subpectoral tenodesis, the tendon was inserted into a drill hole in the humerus and locking tendon stitches were tied over a bone bridge distally. The 12 proximal tenodesis procedures were performed at outside hospitals, and no operative reports from that procedure were available. Based on clinic notes and operative reports from the revision surgery, it can be determined that seven were open, three were arthroscopic, and two remained unclear. Complete data about these index fixation methods are lacking, but include tenodesis screws and absorbable suture anchors. Eight (38%) patients had filed worker's compensation claims at the time of surgery. Five (23.8%) patients were completely lost to follow-up and one patient refused participation [Figure 1].
Figure 1.
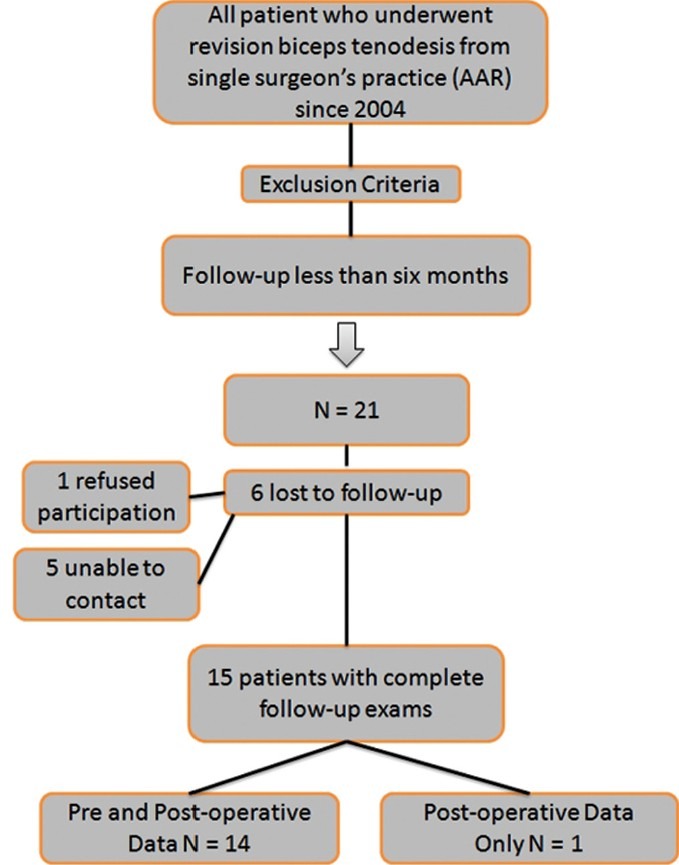
Flow of patients through the study
Previously, 8 (38.1%) patients had a rotator cuff repair, 17 (81.0%) had a subacromial decompression (SAD), 5 (23.8%) had distal clavicle resections, 4 (19.0%) had superior labral anterior-to-posterior (SLAP) repairs, 3 (14.1%) had labral repairs, and 3 (14.1%) had capsular releases. Concurrently, with the revision biceps procedure, a total of 12 (57.1%) had a subacromial decompression, 9 (42.9%) had distal clavicle resections, 3 (14.1%) had rotator cuff repairs, 4 (19.0%) had capsular releases, and 1 patient had a latissimus dorsi transfer. There were 4 (19.0%) patients who received only a revision biceps procedure.
Diagnostic criteria
A diagnosis of persistent symptomatic biceps pathology was made using a combination of history, physical examination findings, and advanced imaging. These patients complained of pain radiating down the anterior aspect of the humerus, and demonstrated tenderness to palpation in the intertubercular groove or subpectoral triangle. Positive Speed's, Yergason's, or O’Brien's testing supported the diagnosis. A diagnosis of biceps tendon rupture was made based on a clinical history of a “popping” sensation, cramping, and weakness with elbow flexion, evaluation for gross deformity of the biceps muscle (Popeye deformity), pain in the anterior aspect of the humerus, and possible findings of biceps tendon rupture on advanced imaging techniques such as magnetic resonance imaging (MRI).
Operative treatment
Operative intervention was undertaken when the clinical presentation and physical examination supported the biceps tendon as a source of persistent pain or disability. All patients failed prior conservative management, including physical therapy, injections, and activity modification. For revision biceps tenodesis, a mini-open subpectoral approach was performed, as has previously been described.[1] Concomitant procedures were performed prior to the biceps tenodesis. The LHB tendon was mobilized arthroscopically, and retrieved through the axillary incision at the inferior border of the pectoralis major tendon. A Fiber Loop Suture (Arthrex, Naples, FL, USA) with No. 2 non-absorbable suture was placed beginning at the musculotendinous junction and continued proximally for 15 mm. The remainder of the LHB was excised. It was not sent for histologic analysis. The humerus was prepared with an 8-mm cannulated reamer over a guide wire inserted into the bicipital groove of the proximal humerus. Care was taken to ream only the anterior cortex of the humerus. One suture limb was then passed through an interference screw (8 × 12 mm polyetheretherketone tenodesis screw; Bio-Tenodesis, Arthrex, Naples, FL, USA), and the tendon was placed within the reamed tunnel. The screw was then advanced until it was flush with bone, and the two suture limbs were tied for secondary fixation.
Postoperative management
Postoperatively, the patient was placed in a sling. The length of immobilization and rehabilitation was dictated by concomitant procedures. For an isolated biceps tenodesis, the sling was discontinued at 4 weeks, with the goal of progressing to full active glenohumeral motion and full passive range of motion of the elbow during this time. Gentle active-assisted elbow range of motion without resistance was also allowed. Active elbow flexion and supination was restricted until 6 weeks postoperatively, then progressing to isometric exercises followed by elastic bands and handheld weights. Depending on their occupation, patients might return to light work within 3–4 weeks, with release to unrestricted activity at 3–4 months.
Outcome assessment
All patients completed a follow-up survey, and were evaluated with the Single Assessment Numeric Evaluation (SANE) score,[19] the Simple Shoulder Test (SST),[20] the American Shoulder and Elbow Surgeons (ASES) score,[21] and the University of California – Los Angeles (UCLA) score.[13,15] The self-reported portion of the ASES score was utilized. Pain scores were recorded using the visual analog scale (VAS). The SF-12 physical component summary (PCS-12) and mental component summary (MCS-12) were also administered. All outcome data were collected at least 6 months postoperatively.
Statistical analysis
All data were collected and analyzed in Microsoft Excel. Descriptive statistics were reported using means and standard deviation where appropriate. A two-tailed paired sample t test was used to compare pre- and postoperative outcome measures. A two-tailed unpaired sample t test was conducted to evaluate whether patients who underwent revision due to biceps rupture differed in clinical outcomes from those who underwent revision due to tendinitis. A Fisher exact test was used to determine if the reason for revision was associated with the type of index biceps tenodesis procedure (subpectoral vs. proximal). The alpha level for all statistics was set at 0.05.
RESULTS
Between January 2004 and March 2011, a total of 21 patients underwent a revision biceps tenodesis. The mean age at the time surgery was 46.5 years (range 23.1–64.9 years). Complete follow-up surveys were obtained by phone interview or mail in 15 of 21 (71.4%) patients. There were a total of 17 men and 4 women. Primary indications for a revision biceps tenodesis were pain due to persistent biceps pathology in 14 (66.6%) patients and biceps rupture in 7 (33.3%) patients. Five out of the seven patients who sustained biceps rupture had undergone a previous subpectoral tenodesis. In these cases, the tenodesis screw was intact. In four of the cases, the tendon re-ruptured at the tenodesis site and retracted distally. In the other case, the Fiberwire suture backed out of the tenodesis screw. The remaining two patients who underwent previous subpectoral tenodesis were revised for persistent pain.
In patients who were revised for persistent pain, hardware and suture from the initial procedure was removed if it was encountered during the procedure. Inflammation and synovitis surrounding the LHB tendon was noted in some patients who underwent previous proximal tenodesis. The one patient who underwent revision tenodesis after tenotomy presented with persistent biceps pain and was found to have autotenodesis of the LHB tendon within the intertubercular groove with an inflamed tendon appearance. Average time from index biceps procedure to revision surgery was 19.6 months (range 3.4–82.4 months). Both preoperative and postoperative scores were available for 14 (66.7%) patients.
The mean follow-up was 33.4 months (range 8.1–73.8 months). The mean postoperative scores were 79 out of 100 (range 25–100), SANE; 10.2 out of 12 (range 3–12), SST; 83 out of 100 (range 45–100), ASES; 44 (range 23–54), PCS-12; 47.1 (range 37–58), MCS-12; 1.9 out of 10 (range 0–6), VAS; and 29 out of 35 (range 22–35), UCLA. Postoperative UCLA scores are reported in Figure 2.
Figure 2.
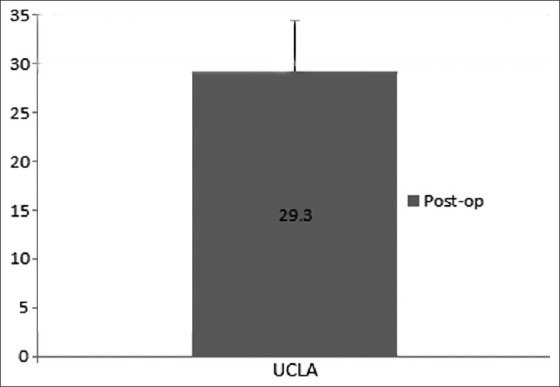
Postoperative clinical outcome: University of California – Los Angeles (UCLA) score at a mean follow-up of 33 months
Seven out of 15 patients reported no pain (46.7%); the mean pain score for the remaining 8 patients was 3.5 (range 2–6) out of 10. Five patients were considered failures, with a UCLA score below 27 (33.3%). Three of those five had active worker's compensation claims at the time of surgery. Only one patient reported that they were not satisfied with the outcomes of their surgery (6.7%). No complications were reported.
Fourteen patients had both preoperative and postoperative data collected. Preoperative data included SANE, SST, ASES, SF-12, and VAS scores. In this group, a paired sample t test was used to compare preoperative and postoperative outcome measures. All clinical outcome measures demonstrated statistically highly significant improvement (P ≤ 0.005) when compared with preoperative scores, except for the MCS-12 score. The preoperative and postoperative scores are presented in Figure 3.
Figure 3.
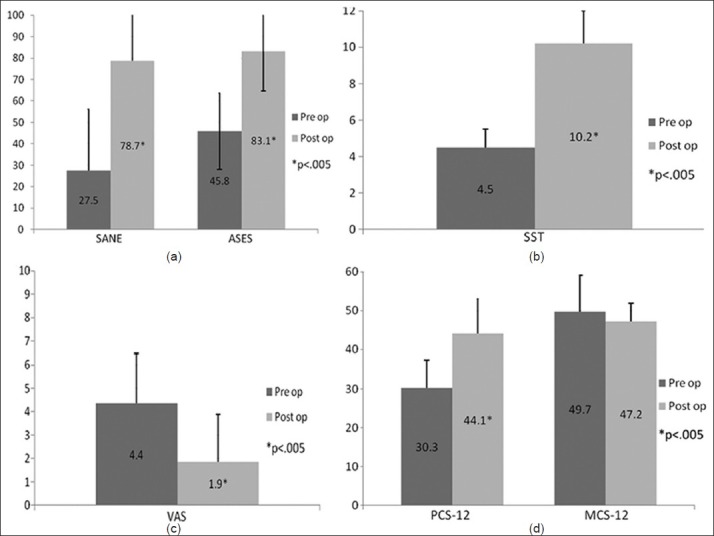
(a) Pre- and postoperative Single Assessment Numeric Evaluation (SANE) and American Shoulder and Elbow Surgeons (ASES) score comparison. (b) Pre- and postoperative Simple Shoulder Test (SST) score comparison. (c) Pre- and postoperative visual analog score (VAS) comparison. (d) Pre- and postoperative SF-12 physical composite score (PCS-12) and mental composite score (MCS-12) score comparison
Seven patients underwent revision due to biceps rupture. A two-tailed unpaired sample t test was performed to evaluate whether these patients differed in their clinical outcomes from those who underwent revision due to biceps tendonitis. The time between the initial biceps procedure and subsequent revision surgery (time to revision) was significantly shorter in patients who underwent revision due to biceps rupture (5.5 months ± 2.8) than those who underwent revision due to biceps tendonitis (18.1 months ± 12.3) [Figure 4]. Otherwise, there was no significant difference in any outcome scores. There was no significant association between initial type of biceps tenodesis (subpectoral vs. proximal) and cause for revision surgery.
Figure 4.
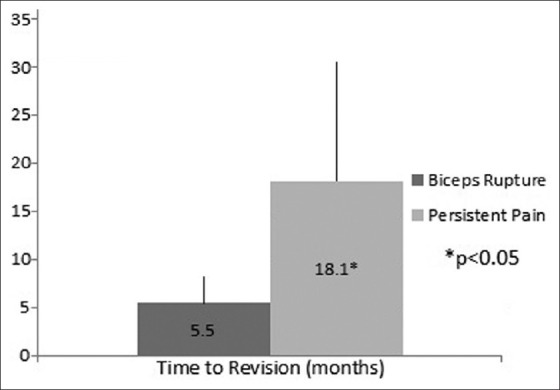
Time to revision in patients who underwent revision due to biceps rupture compared to those who underwent revision due to persistent biceps pain
DISCUSSION
This case series represents one surgeon's experience with revision open subpectoral biceps tenodesis for persistent or recurrent bicipital symptoms following biceps tenotomy or tenodesis. It demonstrates that significant improvement in clinical outcomes can be obtained in this challenging patient population. We demonstrate subjective improvement in all outcome scores, except for the SF-12 mental component score. Additionally, we note that the outcome scores for patients who underwent revision due to biceps rupture or prior tenotomy did not significantly differ from those who underwent revision due to biceps tendinitis. However, the time to revision was significantly shorter in those who experienced biceps rupture after a primary tenodesis procedure.
Both primary biceps tenotomy and tenodesis have had excellent outcomes, and have proven to be effective for pain relief. In our practice, biceps tenotomy is indicated for older, sedentary patients, or patients who are not concerned about the possibility of cosmetic deformity. Gill et al. noted pain relief in 96.7% of patients who underwent arthroscopic primary biceps tenotomy.[10] Walch et al. described an 87% satisfaction rate in patients who underwent an arthroscopic biceps tenotomy in the setting of a massive irreparable rotator cuff tear.[12] Although the primary “complication” of biceps tenotomy has been considered to be a cosmetic deformity of the arm (Popeye deformity), rates of persistent biceps pain and cramping after tenotomy have been reported to range from 3 to 38%.[4,10,15] In the 1 (4.8%) patient in our series who underwent revision biceps tenodesis due to failed tenotomy, the presenting complaint was biceps pain, not cosmetic deformity. Intraoperatively, the tendon was found to be scarred down within the bicipital groove.
Tenodesis has been found to have excellent results, and is indicated in our practice for younger, active patients. Various techniques exist, and most demonstrate success rates of pain relief greater than 90%.[4,8,11,13,14,16,18,22–24] The open subpectoral tenodesis technique that we utilize has shown equally good results.[16] Nho et al. described a series of 353 patients who underwent subpectoral biceps tenodesis with interference screw fixation and reported a complication rate of only 2.0% over a 3-year period.[17] Failure of tenodesis can include mechanical failure or persistent bicipital pain. Mechanical failure presents similar to a biceps tendon rupture, with cosmetic deformity and possible pain or cramping. It typically presents in the early postoperative period.[2] Rates of mechanical failure after tenodesis have been reported to range from 2 to 6%.[7,13,16] Persistent bicipital pain can also be seen after tenodesis. This complication can depend on the type and location of tenodesis performed. Proximal biceps tenodesis at the bicipital groove may either leave diseased tendon within the glenohumeral joint[2] or fail to address pathology within bicipital groove below the tenodesis site. Tenodesis to other structures such as the conjoint tendon, coracoid, or rotator interval may place the tendon in a non-anatomic position, potentially leading to shoulder pain and dysfunction.
We utilized an open subpectoral tenodesis technique for these revision cases for several reasons. This patient population was young (mean age 46.5 years) and highly active (38% worker's compensation). As discussed earlier, biceps tenodesis has been shown to be successful for providing pain relief in this population.[4,8,11,13,14,16,18,22–24] Benefits of the open subpectoral approach include full visualization of the biceps tendon and excision of the diseased proximal biceps tendon. Fixation occurs at an area not typically affected by pathology.[6] Additionally, normal resting length of the tendon within the bicipital groove can be restored by aligning the musculotendinous junction at the level of the inferior border of the pectoralis muscle. The tendon is secured with interference screw fixation and back-up suture fixation, which has been shown to have superior load to failure versus other techniques.[25–31] In the revision setting, conversion to a subpectoral tenodesis eliminates the biceps tendon as a proximal pain generator, which ensures that proximal intertubercular pain that persists is likely to be not biceps related.[2] In patients who underwent a previous subpectoral tenodesis, the tendon was fixed in a different location during revision.
Subpectoral tenodesis can cause persistent anterior humeral pain in some patients. Mazzocca et al. reported anterior humeral pain in 9 out of 41 patients (22%) after subpectoral tenodesis, although none required re-operation.[16] We report 8 out of 15 patients (53.3%) who demonstrated some level of residual pain, although none was severe enough to warrant re-operation. It remains unclear whether the patients with residual pain have anterior humeral pain or pain due to concomitant pathology. We note no cases of re-operation, biceps rupture, or hardware failure in this series. Additionally, although our failure rate of 33.3%, as defined by UCLA score, is greater than published series of primary biceps tenodesis,[4,8,11,13,14,16,18,22–24] we note that 93% of patients were fully satisfied with the procedure. We believe that our strict definition of failure contributes to this increased number, as well as the challenge of treating patients in this revision setting. We could not identify any existing literature regarding outcomes of revision biceps tenodesis; consequently, we are unable to compare these results.
In our study population, all but four patients underwent concomitant procedures at the time of surgery. Therefore, clinical improvements cannot be entirely linked to the revision biceps tenodesis procedure. However, all patients presented with pain and disability related to the biceps tendon, either due to tendinitis or rupture. Pain related to the biceps tendon often presents in association with other glenohumeral pathology,[1–6] and management of concomitant pathology plays an important role in obtaining successful patient outcomes.[11]
Study limitations include the fact that this is a case series with no control group. Additionally, we were only able to collect postoperative data on 15 out of 21 patients (71.4%). Of these, 14 had complete preoperative data as well. Despite losing 6 patients to follow-up, we chose to include all 21 patients in our analysis of revision causes and time to revision to highlight the total group of patients treated during the study time frame. Other criticism includes the lack of objective strength measurement or cosmetic deformity data, which would be needed to quantify any postoperative improvement in these areas. Additionally, we do not have detailed intraoperative data to fully characterize the failure mechanisms of the patients who underwent revision due to biceps rupture.
The nature of our follow-up (average follow-up 33.4 ± 23.5 months) is relatively short term. However, biceps rupture or hardware failure is typically seen in this early postoperative period, and in our series, the average time from primary surgery to revision was 5.5 months. As such, we feel that our follow-up was sensitive enough to capture the majority of patients who would eventually go on to have re-revision surgery or clinical failure. Clearly, long-term results are needed in order to fully understand this complex patient population.
CONCLUSION
Overall, we demonstrate significant improvement in pain relief and functional outcome with revision biceps tenodesis at a mean follow-up of 33.5 months. We demonstrate complete satisfaction in 14 out of 15 patients (93.3%), although we report a UCLA score failure rate of 33%. To our knowledge, this is the first series examining the outcomes of revision biceps tenodesis. Although the success rate of revision biceps tenodesis is lower than that of primary biceps tenodesis, proper patient selection can lead to significant clinical improvement in patients with symptomatic biceps pathology after prior tenodesis or tenotomy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mazzocca AD, Rios CG, Romeo AA, Arciero RA. Subpectoral biceps tenodesis with interference screw fixation. Arthroscopy. 2005;21:896. doi: 10.1016/j.arthro.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Heckman DS, Creighton RA, Romeo AA. Management of failed biceps tenodesis or tenotomy: causation and treatment. Sports Med Arthrosc. 2010;18:173–80. doi: 10.1097/JSA.0b013e3181e892c1. [DOI] [PubMed] [Google Scholar]
- 3.Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581–92. doi: 10.1016/j.arthro.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Wittstein JR, Queen R, Abbey A, Toth A, Moorman CT., III Isokinetic strength, endurance, and subjective outcomes after biceps tenotomy versus tenodesis: a postoperative study. Am J Sports Med. 2011;39:857–65. doi: 10.1177/0363546510387512. [DOI] [PubMed] [Google Scholar]
- 5.Chen CH, Hsu KY, Chen WJ, Shih CH. Incidence and severity of biceps long head tendon lesion in patients with complete rotator cuff tears. J Trauma. 2005;58:1189–93. doi: 10.1097/01.ta.0000170052.84544.34. [DOI] [PubMed] [Google Scholar]
- 6.Friedman DJ, Dunn JC, Higgins LD, Warner JJ. Proximal biceps tendon: injuries and management. Sports Med Arthrosc. 2008;16:162–9. doi: 10.1097/JSA.0b013e318184f549. [DOI] [PubMed] [Google Scholar]
- 7.Boileau P, Krishnan SG, Coste JS, Walch G. Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Arthroscopy. 2002;18:1002–12. doi: 10.1053/jars.2002.36488. [DOI] [PubMed] [Google Scholar]
- 8.Froimson AI. O I. Keyhole tenodesis of biceps origin at the shoulder. Clin Orthop Relat Res. 1975:245–9. [PubMed] [Google Scholar]
- 9.Romeo AA, Mazzocca AD, Tauro JC. Arthroscopic biceps tenodesis. Arthroscopy. 2004;20:206–13. doi: 10.1016/j.arthro.2003.11.033. [DOI] [PubMed] [Google Scholar]
- 10.Gill TJ, McIrvin E, Mair SD, Hawkins RJ. Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg. 2001;10:247–9. doi: 10.1067/mse.2001.114259. [DOI] [PubMed] [Google Scholar]
- 11.Becker DA, Cofield RH. Tenodesis of the long head of the biceps brachii for chronic bicipital tendinitis.Long-term results. J Bone Joint Surg Am. 1989;71:376–81. [PubMed] [Google Scholar]
- 12.Walch G, Edwards TB, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14:238–46. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 13.Checchia SL, Doneux PS, Miyazaki AN, Silva LA, Fregoneze M, Ossada A, et al. Biceps tenodesis associated with arthroscopic repair of rotator cuff tears. J Shoulder Elbow Surg. 2005;14:138–44. doi: 10.1016/j.jse.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 14.Drakos MC, Verma NN, Gulotta LV, Potucek F, Taylor S, Fealy S, et al. Arthroscopic transfer of the long head of the biceps tendon: functional outcome and clinical results. Arthroscopy. 2008;24:217–23. doi: 10.1016/j.arthro.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 15.Kelly AM, Drakos MC, Fealy S, Taylor SA, O’Brien SJ. Arthroscopic release of the long head of the biceps tendon: functional outcome and clinical results. Am J Sports Med. 2005;33:208–13. doi: 10.1177/0363546504269555. [DOI] [PubMed] [Google Scholar]
- 16.Mazzocca AD, Cote MP, Arciero CL, Romeo AA, Arciero RA. Clinical outcomes after subpectoral biceps tenodesis with an interference screw. Am J Sports Med. 2008;36:1922–9. doi: 10.1177/0363546508318192. [DOI] [PubMed] [Google Scholar]
- 17.Nho SJ, Reiff SN, Verma NN, Slabaugh MA, Mazzocca AD, Romeo AA. Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19:764–8. doi: 10.1016/j.jse.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 18.Verma NN, Drakos M, O’Brien SJ. Arthroscopic transfer of the long head biceps to the conjoint tendon. Arthroscopy. 2005;21:764. doi: 10.1016/j.arthro.2005.03.032. [DOI] [PubMed] [Google Scholar]
- 19.Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the single assessment numeric evaluation method and two shoulder rating scales.Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27:214–21. doi: 10.1177/03635465990270021701. [DOI] [PubMed] [Google Scholar]
- 20.Lippitt S, Harryman DI, Matsen F. A practical tool for evaluating shoulder function: the simple shoulder test. In: Matsen FA, Fu FH, Hawkins RJ, editors. A Balance of Mobility and Stability. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1993. pp. 501–18. [Google Scholar]
- 21.King GJ, Richards RR, Zuckerman JD, Blasier R, Dillman C, Friedman RJ, et al. A standardized method for assessment of elbow function. Research Committee, American Shoulder and Elbow Surgeons. J Shoulder Elbow Surg. 1999;8:351–4. doi: 10.1016/s1058-2746(99)90159-3. [DOI] [PubMed] [Google Scholar]
- 22.Nord KD, Smith GB, Mauck BM. Arthroscopic biceps tenodesis using suture anchors through the subclavian portal. Arthroscopy. 2005;21:248–52. doi: 10.1016/j.arthro.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 23.Post M, Benca P. Primary tendinitis of the long head of the biceps. Clin Orthop Relat Res. 1989:117–25. [PubMed] [Google Scholar]
- 24.Dines D, Warren RF, Inglis AE. Surgical treatment of lesions of the long head of the biceps. Clin Orthop Relat Res. 1982:165–71. [PubMed] [Google Scholar]
- 25.Golish SR, Caldwell PE, III, Miller MD, Singanamala N, Ranawat AS, Treme G, et al. Interference screw versus suture anchor fixation for subpectoral tenodesis of the proximal biceps tendon: a cadaveric study. Arthroscopy. 2008;24:1103–8. doi: 10.1016/j.arthro.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 26.Kusma M, Dienst M, Eckert J, Steimer O, Kohn D. Tenodesis of the long head of biceps brachii: cyclic testing of five methods of fixation in a porcine model. J Shoulder Elbow Surg. 2008;17:967–73. doi: 10.1016/j.jse.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Mazzocca AD, Bicos J, Santangelo S, Romeo AA, Arciero RA. The biomechanical evaluation of four fixation techniques for proximal biceps tenodesis. Arthroscopy. 2005;21:1296–306. doi: 10.1016/j.arthro.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 28.Ozalay M, Akpinar S, Karaeminogullari O, Balcik C, Tasci A, Tandogan RN, et al. Mechanical strength of four different biceps tenodesis techniques. Arthroscopy. 2005;21:992–8. doi: 10.1016/j.arthro.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 29.Jayamoorthy T, Field JR, Costi JJ, Martin DK, Stanley RM, Hearn TC. Biceps tenodesis: a biomechanical study of fixation methods. J Shoulder Elbow Surg. 2004;13:160–4. doi: 10.1016/j.jse.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 30.Patzer T, Rundic JM, Bobrowitsch E, Olender GD, Hurschler C, Schofer MD. Biomechanical comparison of arthroscopically performable techniques for suprapectoral biceps tenodesis. Arthroscopy. 2011;27:1036–47. doi: 10.1016/j.arthro.2011.03.082. [DOI] [PubMed] [Google Scholar]
- 31.Patzer T, Santo G, Olender GD, Wellmann M, Hurschler C, Schofer MD. Suprapectoral or subpectoral position for biceps tenodesis: biomechanical comparison of four different techniques in both positions. J Shoulder Elbow Surg. 2012;21:116–25. doi: 10.1016/j.jse.2011.01.022. [DOI] [PubMed] [Google Scholar]


