Figure 1.
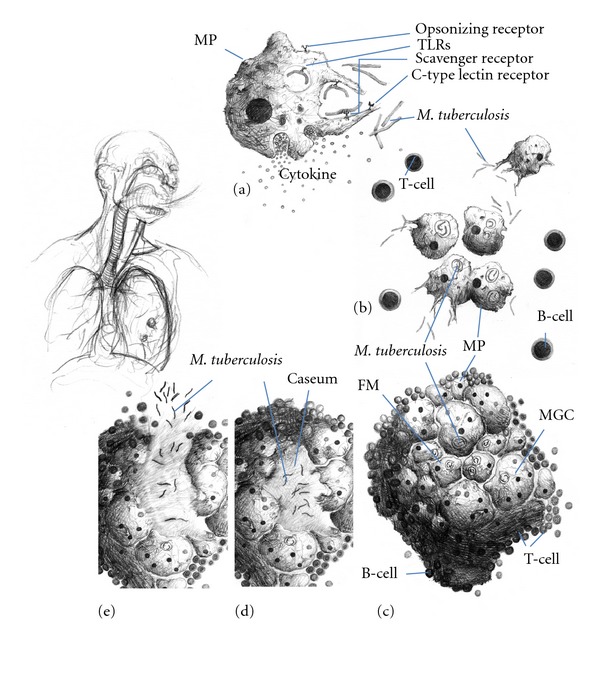
Formation and maturation of lung tuberculous granulomas. Following inhalation of contaminated aerosols, M. Tuberculosis moves to the lower respiratory tract where it is recognized by alveolar macrophages. This recognition is mediated by a set of surface receptors (see text), which drive the uptake of the bacteria and trigger innate immune signalling pathways leading to the production of various chemokines and cytokines (a). Epithelial cells and neutrophils can also produce chemokines in response to bacterial products (not represented). This promotes recruitment of other immune cells (more macrophages, dendritic cells, and lymphocytes) to the infection site (b). They organise in a spherical structure with infected macrophages in the middle surrounded by various categories of lymphocytes (mainly CD4+, CD8+, and γ/δ T cells). Macrophages (MP) can fuse to form MGCs or differentiate into lipid-rich foamy cells (FM). B lymphocytes tend to aggregate in follicular-type structures adjacent to the granuloma ((c), see text for details). The bacteria can survive for decades inside the granuloma in a latent state. Due to some environmental (e.g., HIV infection, malnutrition etc.) or genetic factors, the bacteria will reactivate and provoke the death of the infected macrophages. A necrotic zone (called caseum due to its milky appearance) will develop in the centre of the granuloma (d). Ultimately the structure will disintegrate allowing exit of the bacteria, which will spread in other parts of the lungs and more lesions will be formed. Infection will also be transmitted to other individuals due to release of the infected droplets by coughing (e).
