Abstract
Background: The 2010 Dietary Guidelines emphasized that dietary sodium should be limited to 2300 mg/d, with a lower limit of 1500 mg/d for adults aged >50 y, non-Hispanic blacks, and those with diabetes, hypertension, or chronic kidney disease. The potassium goal remained at 4700 mg/d.
Objective: The objective was to identify subpopulations for whom the 1500- or 2300-mg Na/d goals applied and to examine the joint sodium and potassium intakes for these persons.
Design: The analyses were based on NHANES 2003–2008 data for 12,038 adult men and women aged ≥20 y. Persons aged >50 y, non-Hispanic blacks, and persons with hypertension, diabetes, and chronic kidney disease were identified. Mean sodium, potassium, and energy intakes were obtained from 2 nonconsecutive 24-h dietary recalls. Historical analyses of the sodium-potassium ratios in the American diet were based on NHANES 1971–2006.
Results: Among persons recommended to consume <2300 mg Na/d, <0.12% jointly met the sodium and potassium guidelines. In the 1500-mg/d group, the guidelines were jointly met by <0.015%. Based on Dietary Guidelines, the corresponding dietary sodium-potassium ratio was either 0.49 (2300/4700) or 0.32 (1500/4700). Historical analyses of NHANES data by age-sex groups from 1971 to 2006 showed that sodium-potassium ratios were never <0.83.
Conclusions: Joint dietary guidelines for sodium and potassium, intended for most American adults, are currently being met by ≤0.015% of the population. Extraordinary efforts will be needed to meet the recommendations of the Dietary Guidelines.
INTRODUCTION
Adult Americans consume too much sodium and not enough potassium (1). Current sodium consumption is estimated at 2300–4500 mg/d, whereas potassium consumption is estimated at 2400–3200 mg/d, depending on age and sex (1). The health consequences of excessive sodium intakes and a high sodium-potassium ratio are severe, leading to high blood pressure, heart disease, and stroke (2–5). In recent analyses of deaths linked to NHANES III data (1988–1994), higher sodium-potassium ratios were associated with a higher risk of all-cause and cardiovascular disease mortality (6).
Public health recommendations have stressed a reduction in sodium and a simultaneous increase in potassium intakes (1). The 2010 Dietary Guidelines advise Americans to reduce daily sodium intake to <2300 mg/d per person, with an even lower goal of 1500 mg/d for persons who are aged ≥51 y, are African American, or have hypertension, diabetes, or chronic kidney disease (CKD)4. The 1500-mg/d goal applies to about half of the US population, including children, and to most adults. The 2010 Dietary Guidelines kept potassium goals at the current amount of 4700 mg/d per person (1).
To our knowledge, no study has examined the extent of simultaneous compliance with the sodium and potassium guidelines using nationally representative data. A recent report from the CDC noted that among persons aged ≥18 y with a recommendation of 2300 mg Na/d, 5% met this goal (7). Among persons aged ≥18 y with a recommendation of 1500 mg Na/d, only 0.6% met this goal. The CDC report concluded that meeting the Dietary Guidelines recommendations will require new population-based strategies and increased public health and private efforts (7).
The current hypothesis was that joint compliance with the sodium and potassium guidelines by the targeted groups would be substantially lower than the 0.6% observed for sodium alone. The current research objective was to identify those subpopulations for whom the 1500-mg/d and 2300-mg/d recommendations applied and to estimate their joint compliance with dietary sodium and potassium goals, as based on two 24-h dietary recalls from a nationally representative sample. The associated public health policy objective was to determine whether the analyses of published federal databases would offer insight into the feasibility of the Dietary Guidelines themselves and their likely adoption by the American public, given the current food supply.
METHODS
Analyses of the NHANES 2003ndash2008 database
The current analyses used data for 2003–2008 from NHANES 2003–2008. NHANES is a nationally representative survey of the US noninstitutionalized population aged ≥2 y. The current sample was limited to adults aged ≥20 y with 2 completed and valid 24-h dietary recalls. The following exclusions were made: missing information on diagnosed diabetes, missing information on taking prescriptions to control hypertension, serum creatinine (needed to estimate glomerular filtration rate [GFR]), or missing ratio of urinary albumin to creatinine. The final sample was 12,038 adults aged >20 y.
Information on age, race-ethnicity, CKD, and self-reported hypertension and diabetes was used to identify individuals in the population recommended to consume ≤1500 mg Na/d. All respondents aged >50 y, who reported being non-Hispanic black, who took prescriptions to control hypertension, who reported being told by a medical professional that they have diabetes, or who had a GFR <60 mL · min−1 · m−2 or a urinary albumin-to-creatinine ratio >30 mg/g were included in the reduced-sodium group. GFR was estimated by using the Modification of Diet in Renal Disease study estimating equation (8). All other respondents were included in the 2300-mg Na group. Self-reported hypertension and diabetes assessments were used rather than clinical or laboratory measurements to preserve a sufficiently large sample size and to keep the focus on individuals with known, rather than undiagnosed, diabetes and hypertension.
For each survey participant, sodium, potassium, and energy intakes were obtained from 2 nonconsecutive 24-h dietary recalls. The average of these 2 d was the estimated intake used in this study. This measure reflects less variability than a single 24-h dietary recall, although the means are generally the same. However, the second 24-h dietary recall is done by telephone and systematically results in lower reported energy intakes (and consequently lower nutrient intakes). Although the 2-d values better reflect the true distribution of nutrient intakes, as compared with a single 24-h dietary recall, they do not reflect true estimates of habitual intake. They do provide an upper bound of the proportion of the population meeting a given recommendation, because intakes based on data from multiple days will have less variable distributions. The current purpose was to estimate the more optimistic upper bound for joint adherence to the sodium and potassium guidelines from a representative sample of US adults. Several studies have made the point that a low dietary sodium-potassium ratio may be a marker of high intake of plant foods and lower intake of processed foods (9). Examining food choices characteristic of low-sodium, high-potassium diets may provide additional insight as to how Dietary Guidelines ought to be communicated to the public. All analyses of 2003–2008 NHANES data were conducted by using Stata 11.0 (StataCorp) and accounted for the complex survey design.
Analyses of NHANES data for 1971ndash2006
Previously published results from federal dietary surveys were evaluated with the goal of identifying any population groups that came close to achieving the current recommendations. Published sodium and potassium intakes for males and females aged 12–74 y, by age-sex groups, were based on federal dietary surveys conducted between 1971 and 2006.
Details on NHANES I, which was conducted in 1971–1975, were previously published (10, 11). NHANES II was conducted in 1976–1980 and was based on one 24-h dietary recall. Individual estimates of sodium added in cooking or at the table were not available. NHANES III was conducted in 1988–1994.The data on separate sodium and potassium intakes by age-sex groups, based on NHANES data, were published in the successive Nutrition Monitoring in the United States Reports (12–14). Additional historical data came from the 2005–2006 cycle of NHANES as reported in the 2010 Dietary Guidelines for Americans (15). It is important to note that these sodium-potassium ratios were based on aggregate as opposed to individual-level data.
RESULTS
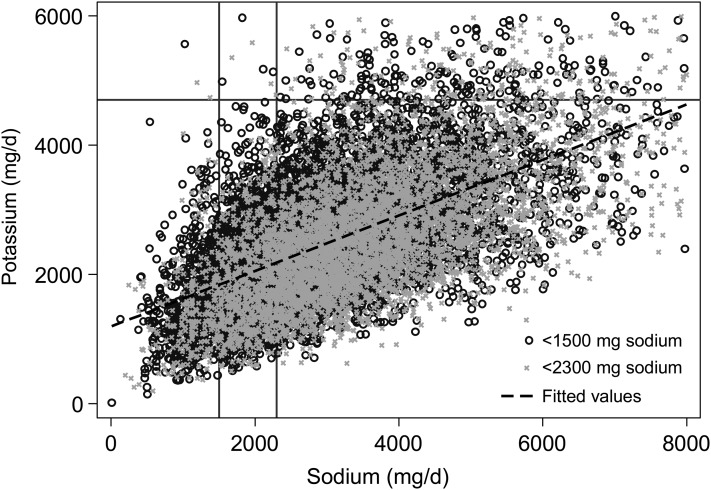
Two-day mean sodium and potassium intakes from NHANES 2003–2008 for adults aged ≥20 y are shown in Figure 1. Persons with recommended sodium intakes of 2300 mg/d and those with recommended sodium intakes of 1500 mg/d are identified. The figure was cropped to exclude potassium intakes >6000 mg/d and sodium intakes >8000 mg/d; however, those persons were included in all other analyses. The recommended sodium and potassium goals (solid lines) and the observed dietary sodium-potassium ratio (dashed line) are also shown in Figure 1.
FIGURE 1.
Two-day mean sodium and potassium intakes among US adults (age ≥20 y), NHANES 2003–2008. Persons with recommended sodium goals of 1500 and 2300 mg/d, respectively, are indicated. Regression lines show the current (broken line) sodium-potassium ratio. Dietary recommendations for sodium and potassium in relation to actual intakes are indicated.
The current estimate was that the recommendation to consume <2300 mg Na/d applied to 49.7% of adults, whereas the 1500-mg/d recommendation applied to 50.3% of adults. Among persons recommended to consume <2300 mg Na/d, 0.12% (95% CI: 0.043, 0.31%; n = 6) jointly met the sodium and potassium guidelines. Among those recommended to consume <1500 mg Na/d, 0.015% (95% CI: 0.002, 0.11%; n = 1) jointly met the sodium and potassium guidelines. Because these values are based on only 2 d of dietary intakes, they are likely overestimates (or an upper bound) of the true proportion in the population who jointly adhere to the 2 recommendations. Thus, the proportion of the US population to whom the 1500-mg/d and 2300-mg/d recommendations apply and who were currently complying with the joint sodium-potassium recommendations can be estimated at being between 0% and 0.015% and 0% and 0.12%, respectively.
A secondary analysis excluded those individuals with CKD from the evaluation of joint adherence to sodium and potassium guidelines, because it is recommended that this population should be consuming a low-potassium diet (16). After this exclusion was applied (n = 2177 excluded), the proportion of the US population to whom the 1500-mg/d recommendation applied and who were currently complying with the joint sodium-potassium recommendations rose from 0.015% to 0.021% (n = 1). The corresponding percentage for those recommended to consume <2300 mg Na/d remained at 0.12%. Even after this subpopulation was excluded, the estimates of joint adherence remained extremely low, between 0% and 0.02% for the reduced sodium group and 0.12% for the 2300 mg/d group.
Additional analyses addressed the correlation between sodium, potassium, and energy intakes. These data are presented in Table 1. The correlation between sodium consumption and energy intakes was 0.81, whereas the correlation between potassium and energy intakes was 0.72. Further analyses evaluated the foods and beverages consumed by the individual whose average 2-d intakes met the recommended guidelines for sodium and potassium (Table 2). The 6 recalls that jointly met the 2300-mg daily sodium and potassium recommendations are provided elsewhere (see supplemental tables under “Supplemental data” in the online issue).
TABLE 1.
Survey-weighted correlation coefficients (and P values) between potassium, sodium, and energy intakes among US adults (n = 12,038)1
| Potassium (mg) | Sodium (mg) | |
| Sodium (mg) | 0.62 (P < 0.001) | — |
| Energy (kcal) | 0.72 (P < 0.001) | 0.81 (P < 0.001) |
These values were obtained by taking the square root of the r2 from bivariate survey-weighted linear regression models.
TABLE 2.
Foods and beverages consumed over 2 d by a single participant (recommended to consume <1500 mg Na/d) whose diet was consistent with the joint sodium and potassium guidelines (<1500 mg Na/d and >4700 mg K/d)
| Recall day | Food description | Weight | Energy | Sodium | Potassium |
| g | kcal | mg | mg | ||
| 1 | Coffee, made from grounds, regular | 4277 | 43 | 86 | 2096 |
| 1 | Milk, cow, fluid, whole | 244 | 146 | 98 | 349 |
| 1 | Sugar, white, granulated, or lump | 50 | 194 | 0 | 1 |
| 1 | Yogurt, fruit variety, not specific as to milk type | 85 | 87 | 49 | 166 |
| 1 | Cookie, peanut | 45 | 215 | 187 | 75 |
| 1 | White potato, chips (including flavored) | 11 | 59 | 57 | 177 |
| 1 | Pork roast, not specific as to cut, cooked, lean only | 208 | 432 | 121 | 879 |
| 1 | White potato, not further specified | 80 | 83 | 19 | 255 |
| 1 | Carrots, cooked, from fresh, fat added | 80 | 45 | 58 | 183 |
| 1 | Celery, cooked, fat added | 77 | 31 | 82 | 213 |
| 1 | Ice cream, regular, chocolate | 200 | 431 | 152 | 497 |
| 2 | Coffee, made from grounds, regular1 | 385 | 4 | 8 | 189 |
| 2 | Chicken, breast, coated, baked/fried, skin eaten | 158 | 412 | 447 | 339 |
| 2 | Coffee, made from grounds, regular1 | 474 | 5 | 9 | 232 |
| 2 | Yogurt, fruit variety, low-fat milk | 170 | 174 | 99 | 332 |
| 2 | Coffee, made from grounds, regular1 | 192 | 2 | 4 | 94 |
| 2 | Pork chop, fried, lean, and fat | 76 | 212 | 46 | 315 |
| 2 | White potato, baked, peel eaten, fat added in cooking | 429 | 466 | 116 | 2225 |
| 2 | White potato skins, with adhering flesh, fried | 85 | 356 | 25 | 852 |
| 2 | Squash, summer, cooked, from canned, fat added | 139 | 52 | 24 | 259 |
| 2 | Corn, yellow, cooked, from frozen, fat added | 354 | 439 | 123 | 854 |
| 2 | Margarine, stick, salted | 15 | 106 | 98 | 3 |
| 2 | Coffee, made from grounds, regular1 | 385 | 4 | 8 | 189 |
| 2 | Ice cream, regular, not chocolate | 175 | 351 | 140 | 347 |
Each row represents a unique food at a unique eating occasion. Therefore, coffee is repeated because it was consumed at different times of the day.
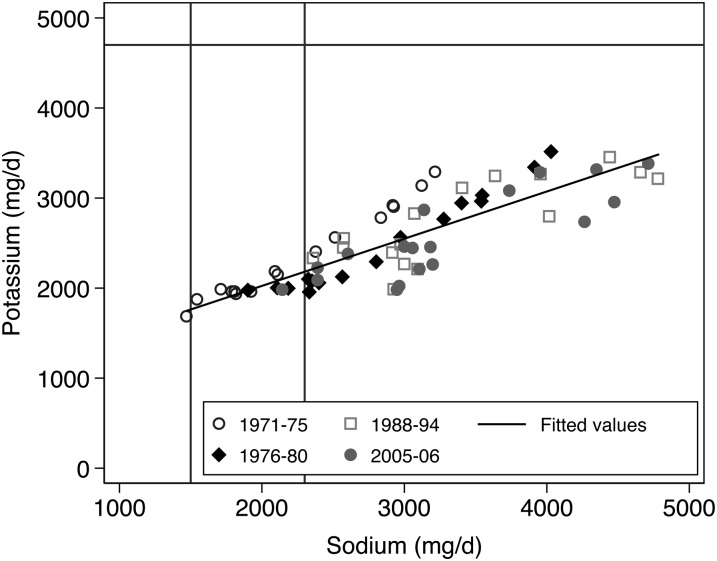
Sodium intakes in the NHANES I data were in the range of 1473 to 3219 mg/d, depending on age and sex, whereas potassium intakes were in the range of 1683 to 3287 mg/d (Figure 2). On the basis of these aggregate data, the mean sodium-potassium ratio was 1.05 (range: 0.83–1.49). The lowest ratios were observed for older women, who had the lowest sodium and energy intakes.
FIGURE 2.
Sodium-potassium ratios calculated from published means by age-sex groups, NHANES 1971–1975, 1976–1980, 1988–1994, and 2005–2006. The values on the plot correspond to mean values of sodium and potassium by different age and sex groups from 4 cycles of NHANES.
Sodium intakes in NHANES II data, also shown in Figure 2, were in the range of 1903 to 4030 mg/d, depending on age and sex, whereas potassium intakes were in the range of 1952 to 3510 mg/d. The mean sodium-potassium ratio was 1.14 (range: 0.96–1.22). Sodium intakes in NHANES III were in the range of 2360 to 4783 mg/d, whereas potassium intakes were in the range of 1984 to 3451 mg/d. The mean sodium-potassium ratio was 1.24 (range: 1.01–1.49). The sodium and potassium intakes for 16 different age-sex groups in the NHANES 2005–2006 cycle were published in the 2010 Dietary Guidelines (1). The previously unpublished mean sodium-potassium ratio was 1.29 (range: 1.08–1.56). At no point from 1971 to 2006 did any age or sex group come close to jointly adhering to the current sodium and potassium recommendations.
DISCUSSION
The 2010 Dietary Guidelines recommend that Americans simultaneously reduce sodium and increase potassium intakes. This is the first report to address simultaneous compliance with the published sodium and potassium goals. Estimates of compliance with the 1500-mg/d and 2300-mg/d sodium goals alone were published by the CDC only recently (7).
The current analyses of NHANES 2003–2008 data used age, sex, race-ethnicity, and health status to distinguish between those adults to whom the 1500-mg/d goal applied and those to whom the 2300-mg/d goal applied. The estimated joint compliance in the first group (1500 mg/d) was 0.015%. The estimated joint compliance in the second group (2300 mg/d) was 0.12%. Because the estimates were based on two 24-h dietary recalls as opposed to habitual intakes, they represent upper bounds. In other words, the true joint compliance with the published sodium and potassium guidelines by the American population was between 0% and 0.015%
To comply with the Dietary Guidelines, sodium intakes would need to decrease by two-thirds from existing intakes, whereas potassium intakes would need to double. This will not be easy, given that both potassium and sodium intakes are closely tied to energy consumption (r = 0.72 for potassium and r = 0.81 for sodium observed here) (17). Young adults with high energy intakes may be able to consume adequate potassium but may not be able to reduce energy intakes sufficiently to meet the low-sodium goals. In contrast, older adults with low energy intakes may meet the low-sodium goals but will not reach adequate potassium levels. To complicate matters further, potassium and sodium are sometimes contained in the same foods (18, 19).
It is a potential problem that the potassium and sodium goals were formulated in terms of milligrams per person per day, regardless of energy needs. One way to address this issue is to index sodium and potassium goals to energy requirements. Such a nutrient-indexing model was used in 1999 for the Dietary Approaches to Stop Hypertension (DASH) diet (20). The 2010 Dietary Guidelines DASH eating plan indicates that sodium is to remain at ≤2300 mg/d regardless of caloric requirements (1).
On the basis of published goals, the sodium-potassium ratio ought to be <1.0. Historical NHANES data from 1971 to 2006, previously published in US Government reports, show that even 40 y ago the sodium-potassium ratio was never <0.83 for any age-sex group. The feasibility of a dramatic 75% reduction in the population-wide sodium-potassium ratio remains to be determined.
Lowering the dietary sodium-potassium ratio by increasing the consumption of potassium-rich foods can be a useful component of dietary advice (21, 22). Increases in dietary potassium have been shown to delay the incidence of hypertension (23). There have also been proposals to replace the absolute potassium and sodium goals with recommended sodium-potassium ratios (6, 24). For example, the DASH eating plan is low in saturated fat, cholesterol, and total fat but encourages the consumption of fruit, vegetables, low-fat milk and dairy products, whole grains, fish, poultry, nuts, and seeds (25). The diet was generally well accepted by study participants and has been shown to have beneficial effects on blood pressure (26, 27) and on heart disease and colorectal cancer (28, 29). Despite the effectiveness of the DASH eating plan, adherence to the plan remains quite low (30).
The 2010 Dietary Guidelines stresses the importance of increasing the consumption of potassium-rich foods. White potatoes, prune and carrot juices, tomato paste and juice, citrus juices, beet greens, spinach, lentils, halibut, yellow fin tuna, and bananas were listed among potassium sources (1). Recent studies on diet quality and cost suggest that meeting dietary guidelines for potassium was associated with sharply higher diet costs (31). In contrast, sodium was not as sensitive to cost as were other components of the 2005 Healthy Eating Index (32). The selection of high-potassium foods may be influenced by cost, taste, accessibility, and acceptability. Many people may find it easier to achieve higher potassium intakes with commonly eaten foods/beverages, such as coffee, potatoes, and milk than with some vegetables, fish, nuts, and seeds. For the 7 individuals who jointly met the reduced sodium and potassium recommendations, coffee, potatoes, dairy products, bananas, fruit juices, dried fruit, nuts, and vegetables were keys to achieving the potassium recommendation, and moderate consumption of processed foods aided in achieving the sodium recommendation (Table 2; see supplemental tables under “Supplemental data” in the online issue). Identifying potassium sources that are both affordable and appealing ought to be a component of practical dietary advice.
The current analyses point to the difficulty of complying with multiple nutrient requirements simultaneously. The Dietary Guidelines are based, in part, on food patterns that were designed to meet sodium and potassium goals at different levels of energy need (1). Linear programming, a mathematical optimization technique, offers an alternative approach to the creation of food patterns that meet multiple nutrient recommendations, while taking into account consumption patterns and cost constraints (33, 34). For example, very-low-sodium diets can be achieved, in principle, by using high amounts of fruit juices, nuts, and seeds and very few grains or meats. However, mathematical modeling, analogous to the Thrifty Food Plan, has shown that the recommended amounts of other nutrients cannot be met at that level of sodium restriction for some age-sex groups. Notably, for all persons aged <50 y, the 1500-mg goal was not feasible, and no mathematical solution was obtained, primarily because of the relatively high energy requirements for this group (35).
The current study had some limitations. First, data analyses were based on the average intake over two 24-h food recalls as opposed to habitual intakes. However, recently developed statistical approaches that can be used to estimate habitual intakes do not allow evaluation of more than one nutrient at a time on an absolute scale or permit the identification of specific persons (and diets) that meet the recommendation. As a result, our population estimates represent a range from 0% to 0.015%. Second, all nutrient intakes were based on self-reports and thus were subject to underreporting or overreporting. Urinary sodium excretion is the gold standard measure of sodium consumption, but it was not available in this large nationally representative sample. Third, sodium intakes from table salt and supplements were not included, which indicates that the current values are underestimates of actual intakes. Last, whereas all cycles of NHANES data have relied on data from a 24-h dietary recall and excluded sodium from table salt in estimating sodium intakes, the methods used in these recalls (eg, nutrient composition tables to estimate intakes and presence of additional queries relevant to sodium intakes) varied from cycle to cycle (36). Even with the disparate and often poor quality of dietary sodium measurements, it can be seen that the sodium-potassium ratios were >1 (Figure 2). Combining NHANES data from more recent cycles (2003–2004, 2005–2006, and 2007–2008) is a standard practice, and the 24-h recall methods are comparable. Despite these limitations, the current data represent the best source of information on the dietary habits of a large and nationally representative sample of adults that informs the nation's food and nutrition policy (7, 10, 11).
The current analyses of federal data raise some final questions about the role of feasibility research in the formulation of public policy. First, the fact that the proposed sodium and potassium goals are currently met by <0.015% of the US population should be an indication of potential problems ahead. Dealing with 99.985% noncompliance will be a challenge for public health practitioners. Reducing the sodium content of the US diet may be a challenge for the food industry (7, 31, 37). Preliminary analyses showed that reducing the sodium content of all foods and beverages in NHANES participants by as much as 25% would raise compliance levels to 0.044% (n = 3) in the 1500-mg Na/d group and to 0.3% (n = 16) in the 2300 mg Na/d group. Future dietary guidelines might also note whether the proposed goals are intended as realistic or aspirational. Ideally, cost and feasibility analyses ought to precede or accompany the issuing of dietary guidelines instead of following them by >1 y.
Supplementary Material
Acknowledgments
We thank 4 anonymous reviewers for helpful comments on a previous draft.
The authors’ responsibilities were as follows—AD, MM, and CR: designed and conducted the research and wrote the manuscript; AD and CR: analyzed the data; and AD: had primary responsibility for the final content. All authors read and approved the final manuscripts. No conflicts of interest were declared.
Footnotes
Abbreviations used: CKD, chronic kidney disease; DASH, Dietary Approaches to Stop Hypertension; GFR, glomerular filtration rate
REFERENCES
- 1.US Department of Agriculture, US Department of Health and Human Services. Dietary Guidelines for Americans, 2010 7th ed Washington, DC: US Government Printing Office, 2010 [Google Scholar]
- 2.He J, Ogden LG, Vupputuri S, Bazzano LA, Loria C, Whelton PK. Dietary sodium intake and subsequent risk of cardiovascular disease in overweight adults. JAMA 1999;282:2027–34 [DOI] [PubMed] [Google Scholar]
- 3.Appel LJ, Frohlich ED, Hall JE, Pearson TA, Sacco RL, Seals DR, Sacks FM, Smith SC, Jr, Vafiadis DK, Van Horn LV. The importance of population-wide sodium reduction as a means to prevent cardiovascular disease and stroke: a call to action from the American Heart Association. Circulation 2011;123:1138–43 [DOI] [PubMed] [Google Scholar]
- 4.Cook NR, Obarzanek E, Cutler JA, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK; Trials of Hypertension Prevention Collaborative Research Group Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention Follow-up Study. Arch Intern Med 2009;169:32–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ 2009;339:b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, Chang MH, Gwinn M, Dowling N, Khoury MJ, et al. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 2011;171:1183–91 [DOI] [PubMed] [Google Scholar]
- 7.Usual sodium intakes compared with current dietary guidelinesmdashUnited States, 2005-2008. MMWR Morb Mortal Wkly Rep 2011;60:1413–7 [Google Scholar]
- 8.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 2003;139:137–47 [DOI] [PubMed] [Google Scholar]
- 9.Dietary Guidelines Advisory Committee Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010, to the Secretary of Agriculture and the Secretary of Health and Human Services. Washington, DC: US Department of Agriculture, Agricultural Research Service, 2010 [Google Scholar]
- 10.McDowell A, Engel A, Massey JT, Maurer K. Plan and operation of the Second National Health and Nutrition Examination Survey, 1976-1980. Vital Health Stat 1 1981;15:1–144 [PubMed] [Google Scholar]
- 11.Engel A, Murphy RS, Maurer K, Collins E. Plan and operation of the HANES I augmentation survey of adults 25-74 years United States, 1974-1975. Vital Health Stat 1 1978;14:1–110 [PubMed] [Google Scholar]
- 12. Nutrition Monitoring in the United States–an update report on nutrition monitoring. Life Sciences Research Office, Federation of American Societies for Experimental Biology. Available from: http://www.cdc.gov/nchs/data/misc/nutri89acc.pdf (cited 10 September 2011.
- 13. Third Report on Nutrition Monitoring in the United States–Executive Summary. Life Sciences Research Office, Federation of American Societies for Experimental Biology. Available from: http://www.cdc.gov/nchs/data/misc/tronm.pdf (cited 5 September 2011)
- 14.US Department of Agriculture, Human Nutrition Information Service, Nutritional Monitoring Division Nationwide Food Consumption Survey Continuing Survey of Food Intakes by Individuals—women 19-50 years and their children 1-5 years, 4 days. Washington, DC: USDA, 1987:63 [Google Scholar]
- 15. What we eat in America, NHANES 2005-2006. US Department of Health and Human Services. Available from: http://www.ars.usda.gov/Services/docs.htm?docid=13793 (cited 11 August 2011)
- 16. Nutrition and Chronic Kidney Disease. National Kidney Foundation. Available from: http://www.kidney.org/atoz/pdf/nutri_chronic.pdf (cited 10 November 2011)
- 17.Arbeit ML, Nicklas TA, Berenson GS. Considerations of dietary-sodium potassium energy ratios of selected foods. J Am Coll Nutr 1992;11:210–22 [PubMed] [Google Scholar]
- 18. NCI, Applied Research Program. Sources of sodium among the US population. 2005–06. Updated 21 December 2010. Risk Factor Monitoring and Methods Branch. Available from: http://riskfactor.cancer.gov/diet/foodsources/sodium/ (cited 13 November 2011)
- 19. NCI, Applied Research Program. National Cancer Institute. Sources of potassium among the US population. 2005–06. Updated 21 December 2010. Risk Factor Monitoring and Methods Branch. Available from: http://riskfactor.cancer.gov/diet/foodsources/potassium/ (cited 13 November 2011.
- 20.Lin PH, Windhauser MM, Plaisted CS, Hoben KP, McCullough ML, Obarzanek E. The Linear Index Model for establishing nutrient goals in the Dietary Approaches to Stop Hypertension trial. DASH Collaborative Research Group. J Am Diet Assoc 1999;99:S40–4 [DOI] [PubMed] [Google Scholar]
- 21.Mozaffarian D, Appel LJ, Van Horn L. Components of a cardioprotective diet: new insights. Circulation 2011;123:2870–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grimes CA, Campbell KJ, Riddell LJ, Nowson CA. Sources of sodium in Australian children's diets and the effect of the application of sodium targets to food products to reduce sodium intake. Br J Nutr 2011;105:468–77 [DOI] [PubMed] [Google Scholar]
- 23.Morris RC, Jr, Sebastian A, Forman A, Tanaka M, Schmidlin O. Normotensive salt sensitivity: effects of race and dietary potassium. Hypertension 1999;33:18–23 [DOI] [PubMed] [Google Scholar]
- 24.Meneton P, Lafay L, Tard A, Dufour A, Ireland J, Ménard J, Volatier JL. Dietary sources and correlates of sodium and potassium intakes in the French general population. Eur J Clin Nutr 2009;63:1169–75 [DOI] [PubMed] [Google Scholar]
- 25.National Heart Lung and Blood Institute. Your guide to lowering your blood pressure with DASH. Revised April 2006. Available from: http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf (cited 15 October 2011)
- 26.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997;336:1117–24 [DOI] [PubMed] [Google Scholar]
- 27.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, III, Simons-Morton DG, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001;344:3–10 [DOI] [PubMed] [Google Scholar]
- 28.Levitan EB, Wolk A, Mittleman MA. Relation of consistency with the dietary approaches to stop hypertension diet and incidence of heart failure in men aged 45 to 79 years. Am J Cardiol 2009;104:1416–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fung TT, Hu FB, Wu K, Chiuve SE, Fuchs CS, Giovannucci E. The Mediterranean and Dietary Approaches to Stop Hypertension (DASH) diets and colorectal cancer. Am J Clin Nutr 2010;92:1429–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mellen PB, Gao SK, Vitolins MZ, Goff DC, Jr, Mellen PB, Gao SK, Vitolins MZ, Goff DC. Jr. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med 2008;168:308–14 [DOI] [PubMed] [Google Scholar]
- 31.Monsivais P, Aggarwal A, Drewnowski A. Following federal guidelines to increase nutrient consumption may lead to higher food costs for consumers. Health Aff (Millwood) 2011;30:1471–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rehm CD, Monsivais P, Drewnowski A. The quality and monetary value of diets consumed by adults in the United States. Am J Clin Nutr 2011;94:1333–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Darmon N, Ferguson EL, Briend A. A cost constraint alone has adverse effects on food selection and nutrient density: an analysis of human diets by linear programming. J Nutr 2002;132:3764–71 [DOI] [PubMed] [Google Scholar]
- 34.Rambeloson ZJ, Darmon N, Ferguson EL. Linear programming can help identify practical solutions to improve the nutritional quality of food aid. Public Health Nutr 2008;11:395–404 [DOI] [PubMed] [Google Scholar]
- 35.Maillot M, Drewnowski A. A conflict between nutritionally adequate diets and meeting the 2010 dietary guidelines for sodium. Am J Prev Med 2012;42:174–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loria CM, Obarzanek E, Ernst ND. Choose and prepare foods with less salt: dietary advice for all Americans. J Nutr 2001;131:536S–51S [DOI] [PubMed] [Google Scholar]
- 37.Bernstein AM, Willett WC. Trends in 24-h urinary sodium excretion in the United States, 1957-2003: a systematic review. Am J Clin Nutr 2010;92:1172–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.