SUMMARY
Objective
The aim of this study is a systematic review of the literature on the strength and long-term behavior of zirconia FPDs.
Methods
The literature search was performed using as the primary source the Medline database. Were also imposed a set of inclusion and exclusion criteria in order to narrow the search to differentiate the two distinct parts in which it was structured the review. In addition, MeSH terms were applied to further refine the choice of articles more relevant to the review. In the part of the review concerning the long-term behavior of zirconia fixed partial dentures were considered useful only those studies with a minimum follow-up of one year.
Results
The search provided a total of 813 articles, but only 25 were considered for the review because they were the only ones who satisfied search criteria. In particular, 13 items relate to the mechanical strength of zirconia prostheses and 12 regarding the long term behavior of zirconia FPDs. The resistance values also exceed the 2000 N while the survival rate reaches to almost 94%.
Conclusions
Based on this review, Zirconia FPDs can be considered reliable products in both the anterior and posterior fields with survival rates comparable to traditional metal-ceramic prostheses.
Keywords: zirconia, fixed partial dentures, fracture strenght, connector size, long term behavior
RIASSUNTO
Obiettivo
Lo scopo del lavoro è una revisione della letteratura sulla resistenza delle protesi fisse in zirconia ed il comportamento a lungo termine delle stesse.
Metodi
La ricerca della letteratura è stata effettuata utilizzando come principale fonte il database Medline. Sono stati altresì imposti dei criteri di inclusione e di esclusione al fine di restringere il campo di ricerca differenziati per le due diverse parti in cui è stata strutturata la revisione. Inoltre sono stati applicati dei termini MeSH per raffinare ulteriormente la scelta degli articoli più utili ai fini della revisione. Nella parte della revisione riguardante il comportamento a lungo termine delle protesi fisse in zirconia sono stati considerati utili solo quegli studi con un follow-up minimo di un anno.
Risultati
La ricerca ha prodotto un totale di 813 articoli ma solo 25 sono stati presi in considerazione per la seguente revisione in quanto erano i soli a soddisfare i criteri di ricerca. In particolare 13 articoli riguardano la resistenza meccanica delle protesi fisse in zirconia mentre 12 il comportamento a lungo termine delle stesse. I valori di resistenza superano anche i 2000 N mentre la percentuale di sopravvivenza arriva a sfiorare il 94%.
Conclusioni
Basandosi sulla presente revisione le protesi fisse in zirconia possono essere considerate dei manufatti affidabili sia nei settori anteriori sia nei settori posteriori con percentuali di sopravvivenza paragonabili alla tradizionale protesi metallo-ceramica.
Introduction
The increasing demand from the patient to an aesthetic ideal of the restorations placed in the mouth, has led the scientific research towards the discovery of a material that has, in addition to the aforementioned aesthetic characteristics, also mechanical strength suitable to withstand masticatory loads that develop in the posterior areas of the oral cavity.
For several years many scholars have followed at a relentless pace in order to find a material that combines excellent aesthetic characteristics with high mechanical properties.
The so-called “metal-free” restorations (or non-metallic) have always represented a challenge for dentistry and only in recent years, with the introduction of zirconia, has achieved this goal.
The story contains several attempts to create a material that would allow to replace metal of the traditional metal-ceramic prostheses with often disappointing results.
We have moved from the use of all-ceramic crowns made by a feldspar of Land (1) from the beginning of the nineteenth century and without acceptable mechanical properties in products with higher strength, however, rather low, with the addition of aluminum oxide feldspathic ceramics dating from the mid-nineteenth century thanks to the work of McLean and Hughes (2).
To make ceramics more resistant many efforts were made mainly consisting in increasing the percentage of crystals: hence the Empress (containing more leucite), the Cerapearl (containing more hydroxyapatite), the In-Ceram (infiltration of a set of oxides of aluminum, magnesium, zirconia) or Procera (polycrystalline ceramic), and more.
In recent years there has been a sudden improvement in materials that can be used for the fabrication of prostheses with high mechanical properties; this led to the introduction of zirconia (Y-TZP) for the construction of prosthetic devices and the results were exceptional: in fact, thanks to its outstanding mechanical properties, zirconia is suitable to be used for restoration in the posterior of the mouth, areas that until recently were exclusively the prerogative of the metal-ceramic.
The main problem that prevented the use of metal-free restoration is due to the fact that the ceramic has some micro defects in its structure that over time they tend to widen and in the end lead up to the fracture and the failure of the prostheses. This is true for almost all ceramic materials but not for the zirconia that can overcome this problem by transforming from tetragonal phase to the monoclinic one (t → m) known as “transformation toughening”, and that allows the material to increase greatly its strength. In fact, when a micro defect estabilishes in the material, the transformation (t → m) takes place accompanied by a volume increase of 3–4 %, which creates a force that opposes further crack propagation resulting in immediate increase in mechanical properties of material (3,4).
In order to demonstrate the absolute reliability of zirconia in the development of prosthetic devices in all areas of the oral cavity, was conducted a thorough review of the literature focused mainly on two aspects of fundamental importance: the mechanical strength of zirconia fixed partial dentures with special reference to the size of the connector and the long-term behavior of FPDs, essential parameter to define a material as “reliable.”
Methods
The literature search was performed using as the main source of research database Medline (Pubmed). For research have been typed the following words ‘zirconia dental’ and were obtained a total of 813 articles. The items considered were published from November 1990 until January 2010.
In order to make the search more specific and exclude items not relevant for the purposes of the study were applied the following inclusion criteria:
Zirconia single crowns
Zirconia bridges
Literary reviews
Studies in english
Follow-up at least 1 year
And the following exclusion criteria:
Descriptive studies
Case reports
Other manufactures (implants, pins, etc.)
Items of discussion and debate
Follow-up less than 1 year
To further narrow the search have been used the following Mesh terms (Medical Subject Headings):
Crowns, fixed partial dentures, strenght, resistance, FPDs, dental prostheses regarding the articles on the strenght of zirconia FPDs.
Clinical behavior, lifetime, reliability, survival, long term survival, prospective, strenght, crowns, fixed partial dentures regarding the articles on the long term behavior of zirconia FPDs.
Results
By applying the various criteria outlined above and the MeSH terms listed above, it was possible to obtain a total of 25 articles divided into two strands:
13 articles on the strength of zirconia fixed partial dentures
12 articles on the long-term behavior of zirconia fixed partial dentures
Going more in particular of the 13 articles relating to the strength of zirconia fixed partial dentures, five articles focus on the size of the connector of the zirconia bridges which is a key parameter for the success of the prostheses. The remaining 8 articles dealing with instead of the mechanical capacity of the bridges in zirconia with particular regard to the fracture resistance.
The following table lists the eight items relating to the strength of the zirconia bridges (Table 1).
Table 1.
Zirconia bridges strength.
| Author | Year | System | Zirconia | FPDs | Unit | Average resistance to fracture (N) | |
|---|---|---|---|---|---|---|---|
| Anterior | Posterior | 3 | >3 | ||||
| Rosentritt et al.(5) | 2001 | Lava™ | - | 32 | 32 | - | 992 |
| Rountree et al.(6) | 2001 | Lava™ | - | 32 | 16 | 16 | 1816/978 |
| Suttor et al.(7) | 2001 | Lava™ | - | 16 | 16 | - | 1457 |
| Tinschert et al.(8) | 2001 | DCM | - | 16 | 16 | - | > 2000 |
| Luthy et al.(9) | 2004 | DCM | - | 15 | 15 | - | 755 |
| Stiesch-Scholz et al.(10) | 2007 | DCM | - | 40 | - | 40 | 1265 |
| Dornhofer et al.(11) | 2007 | InCeram® | - | 20 | 20 | - | 2527 |
| Wael Att et al.(4) | 2007 | DCM | - | 48 | 48 | - | 1522/1702 |
The year of publication of the articles examined varies from 2001 to 2007. Moreover, the type of zirconia taken into account varies in 8 articles:
7 articles deals with the most common type of zirconia on the market, the so-called Y-TZP: this is a type of zirconia which undergoes a process from presintered blocks, that are more easily to work, through the use of the CAD/CAM, a software that operate a scan of the prostheses (CAD) and then arrange for its milling (CAM) to form the final structure.
1 article on the Inceram Zirconia®: this is a type of zirconia obtained by the addition of alumina to its structure. In particular, it is composed of 67 % by weight of alumina (Al2O3) and 33 % zirconium oxide (ZrO2). It is a type of zirconia introduced for aesthetic reason but now superseded by Y-TZP because of its lower mechanical properties.
Moreover there is a difference in the type of prostheses (for anterior or posterior) and in the number of units of FPDs (3,4,5 units). In all the studies are examinated only posterior prostheses and this is easy to understand. In fact, the modern zirconia used in the prosthetic field has mechanical qualities that make sure the placement in the anterior of the mouth where chewing forces developed are certainly much lower than those of the posterior. So it was useless to consider prostheses for anterior because of the absolute safety concern in prosthetic applications in these areas of the mouth.
Also important is the number of elements constituting the prostheses: in most cases are examined 3 elements bridge, while only a minority of cases are dealt with bridges of several elements (4 or 5). The test used is a traditional three point bending. Analyzing the results we can immediately see how the zirconia bridges exceed in almost all cases the threshold of 1000 N (range between 992 N and 2527 N), while in one study achieved values are even higher than 2000 N (8). In another study instead the values obtained are very low (755 N) but this is due to the fact that have been examined only zirconia structures in the absence of the veneering ceramic (9).
The next 5 items are focused on the minimum size of the connector of the zirconia FPDs. The results are shown in the following table (Table 2).
Table 2.
Recommended size connector of Zirconia FPDs.
The year of publication of the articles range from 2001 to 2007. Examining these results, you may notice differences in the number of units making up the prostheses. In particular, in two studies are examined only bridges of 3 units (12,13), in other two studies only 4-unit bridges (9,15) and only one paper deals with 5-unit bridges (14). It is also important to point out that all studies examined only posterior bridges.
The size of the connector varies greatly from one another and these variations depend primarily on the number of constituent units of the prostheses (3.4 or 5), then on the procedures that were submitted to the prostheses (artificial aging procedures). In almost all cases, the recommended size of the connector for the bridges of three elements is greater than 6.25 mm2. The size obviously rise as the number of units making up the bridge (4 or 5).
The connector is definitely the weak point of the entire restorations and its size should be adjusted in height and width in order to allow long-term survival of the restoration without the danger of unexpected failure. In fact, in several studies it was shown that the failure of the restoration is almost always due to a fracture that begins at the gingival portion of the connector.
One important study of Studart et al. (14) based on the evaluation of some fatigue parameters of the prostheses, found that the size of the connector should be at least 5.7 mm2, 12.6 mm2 and 18.8 mm2 for the bridges respectively of 3, 4 and 5 units (14).
The second part of the review is focused instead on long-term behavior of zirconia FPDs. The selected studies amount to a total of 12 and are listed in the following table (Table 3).
Table 3.
Long term behavior of Zirconia FPDs.
| Author | Year | System | Zirconia | FPDs | Unit | Follow-up | Fracture (%) | Fracture (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Anterior | Posterior | 3 | >3 | year | (core) | (veneer) | |||
| Sturzenegger et al.(16) | 2000 | Direct ceramic machining | - | 21 | 21 | - | 1 | 0.0 | 0.0 |
| Pospiech et al.(17) | 2003 | Lava™ | - | 38 | 38 | 0 | 1.5 | 0.0 | 2.5 |
| Bornemann et al.(18) | 2003 | Cercon® | - | 59 | 44 | 15 | 1 | 0.0 | 4.3 |
| Suarez et al.(19) | 2004 | Inceram® | - | 18 | 18 | - | 3 | 0.0 | 0.0 |
| Von Steyern et al.(20) | 2005 | Precident | 3 | 17 | 2 | 18 | 2 | 0.0 | 15.0 |
| Sailer et al.(21) | 2006 | Direct ceramic machining | - | 57 | N.R. | N.R. | 3 | 0.0 | 13.0 |
| Raigrodski et al.(22) | 2006 | Lava™ | - | 20 | 20 | 0 | 3 | 0.0 | 15.0 |
| Sailer et al.(23) | 2007 | Direct ceramic machining | - | 33 | - | - | 5 | 2.2 | 15.2 |
| Edelhoff et al.(24) | 2008 | Digident® | 4 | 18 | 14 | 8 | 3 | 0.0 | 9.5 |
| Tinschert et al.(25) | 2008 | Precident | 15 | 50 | 44 | 21 | 3 | 0.0 | 6.1 |
| Molin et al.(26) | 2008 | Cad. esthetics® | 0 | 19 | 19 | 0 | 5 | 0.0 | 0.0* |
| Roediger et al.(27) | 2009 | Cercon® | - | 99 | N.R. | N.R. | 4 | 1.0 | 13.1 |
The year of publication for selected articles ranging from 2000 to 2009. The studies differ in the system used:
3 articles deal with DCM systematic;
2 articles deal with Lava™ systematic;
2 articles deal with Cercon® systematic;
2 articles deal with Precident® systematic;
1 article deals with Inceram® systematic;
1 article deals with Digident® systematic;
1 article deals with Cad. esthetics® systematic;
Moreover, all the articles deal with zirconia bridges. Of these, only three articles deal with bridges for anterior and posterior (20, 24,25) whereas in the remaining cases are reviewed only posterior bridges. In most cases are examined 3-unit bridges while only four studies involved more elements (> 3) (18,20,24,25). In two studies are not specified the number of bridges examined (21, 27).
The average follow-up of these studies is 3 years with a minimum of one year recorded in two studies (16,18) and a maximum of 5 years recorded in two other studies (23,26). From these studies it is possible to obtain the failure rates in terms of fracture of zirconia structure (core) or veneering ceramic (veneer).
Very interesting are the two studies by Sailer et al. (2007) based on a systematic literature review to assess the survival of all-ceramic restorations than metal-ceramic. In particular, the observation period was at least 3 years. They, in the 9 items that studied the all-ceramic restorations, selected 343 bridges in total, with a follow-up period of 3.8 years. Of these 343 bridges, 33 are lost. So a median survival at 5 years was 93.3%. In the posterior survival rate at 5 years was 84, 4%. These results are not unique to zirconia restorations but also alumina ceramics. Instead for the metal-ceramic bridges were examined 1163 prostheses after a follow-up period of 8 years and only 121 are lost after this period. Thus, a survival rate of 95.6% (21,23).
Moreover, in several studies in the literature is clear that complications of the restorations can be divided into biological and technical. The most important complication is fracture of the veneering ceramic, which is one of those technical, while the fracture of the zirconia core or restoration decementation are quite rare complications (24,25).
Discussion
Analyzing the articles selected for this review, it is possible to make some interesting observations. We start by analyzing the aspects concerning the strength of zirconia fixed prostheses examined in detail in the first part of the review. From the selected studies can be seen that the prostheses subjected to load exceed almost always and widely the threshold of 1000 N. This threshold is identified by scholars as the minimum value of load that a posterior prostheses has to bear in order to be placed in that areas of the oral cavity with sufficient security. Thus, while acknowledging that normally grow mean forces around 500 N in these areas of the mouth, it is imperative that a prostheses should bear at least twice this load. This is because the restorations placed in the oral cavity undergo a decrease in strength over time of approximately 50% of the initial value, so when they are placed in the mouth must have a initial value of strength of about twice of the majority of forces that on average develop in the posterior areas. So the threshold of 1000 N is very important and has been widely verified that the zirconia FPDs exceed this limit. It is also true that, when in the oral cavity there is the presence of parafunctions like bruxism etc., it is better to resort to the traditional metal-ceramic restorations because the forces that come into play are certainly much higher and can cause the failure of restorations.
Another consideration to do regard differences in values obtained in different studies. This is attributable to proceedings to which the specimens were subjected. Indeed, in some studies were implemented procedures for artificial aging (thermal and mechanical cycles), while in other studies not. The artificial aging procedures are intended to simulate conditions which are to establish the patient’s mouth that is continuous mechanical stresses and temperature changes of some significance that in time lead to a substantial decrease in the strength of the prostheses. All this to emphasize that in cases where the specimens were subjected to these procedures (4,5,6,7,10) resistance to fracture was significantly lower than when such procedures were not applicate (8, 9,11).
From these studies it is clear, however, such as zirconia prostheses largely exceed the threshold of 1ooo N even when subjected to artificial aging procedures.
Subject of considerable importance is that concerning the size of the connector of the zirconia bridges. The connector is the portion of the restoration that serves as a “trait d’union” between the intermediate section of the bridge and the crown pillar that holds the prostheses. The connector is definitely the weak point of the entire restoration and its size should be adjusted in height and width sufficient to allow long-term survival of the restoration without the danger of unexpected failure. In fact, in several studies it was shown that the failure of the restoration is almost always due to a fracture that begins at the gingival portion of the connector.
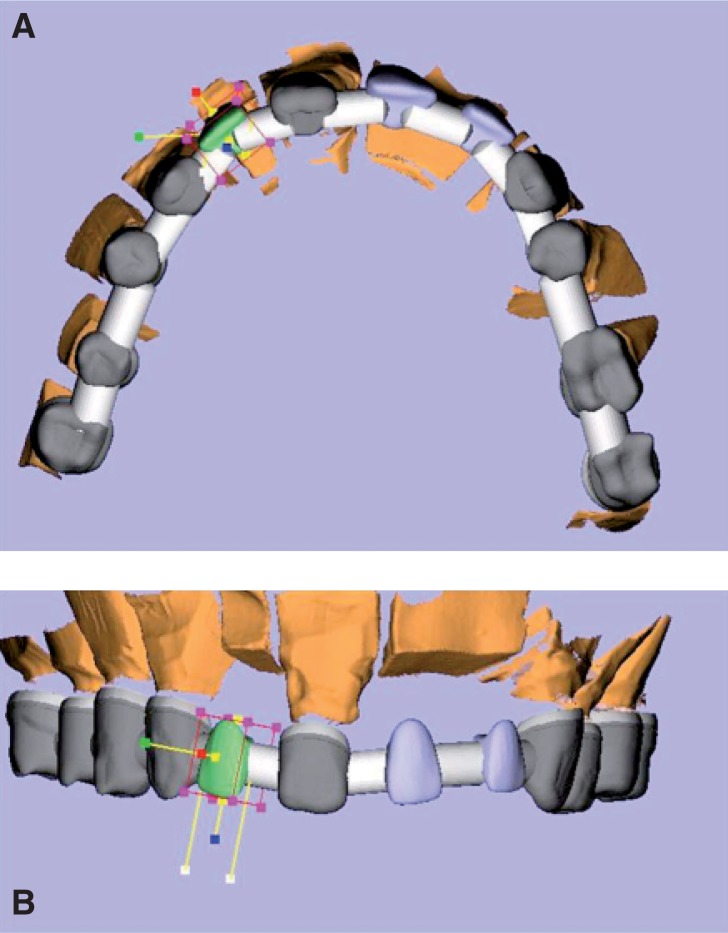
From several studies in the literature the ideal size of connector should be 9 mm2 (3 mm X 3 mm) (Figs. 1a–1b–2). For some, this size may fall as low as 6.25 mm2 always referring to the bridges of three elements.
Figura 1.
In literature, several studies indicate that the ideal size of connector should be 9 mm2 (3 mm X 3 mm), and that the correct computer programming at CAD greatly increases the predictability of the prosthesis.
Figure 2.
The framework just out of phase CAM. At this stage the diameter of the connectors is oversize to allow the technician to work it in the finishing stages, obtaining a wide margin of safety.
If the prostheses replaces two teeth instead of one, the connector should be larger than the above and still be more than 7 mm2.
Indeed it was demonstrated that the ability to withstand the masticatory loads is two times lower in bridges of 4 elements than those of 3 elements (9). An important study of Studart et al. (2007) based on the evaluation of some fatigue parameters of the restorations, found that the size of the connector should be at least 5.7 mm2, 12.6 mm2 and 18.8 mm2 for the bridges respectively of 3, 4 and 5 units (14). These dimensions are quite safe considering the forces that normally develop during chewing. In fact, according to various studies, the maximum forces that are developed during normal mastication vary greatly from person to person. In the anterior region it comes to values of a few hundred Newton (about 20 kg) while in the posterior values increase considerably even up to a thousand Newton (nearly 100 kg). Average values that are obtained amounted to about 500 N (about 50 kg). The maximum values are obtained at the first molar. Lower values are recorded in women, children and even in patients with signs and symptoms of the masticatory system dysfunction. However, the forces that develop during normal chewing activity (eg chewing gum) are much lower than the maximum occlusal forces that are normally registered (14).
In addition, increasing the size of the connector from 3 to 4 mm in diameter the stress in the area of the connector are reduced by approximately 50% (14). Some authors suggest that the size of the connector should be more vertically instead horizontal (13,14). However in other studies is highlighted as the horizontal forces are predominant in some cases.
However, when the chewing forces are excessive, as in patients with deep bite, with bruxism or where there were already previous failures in rehabilitation, it would be appropriate to use larger diameter of 4 mm or better to opt for the traditional metal-ceramic restorations.
Moreover, even if it would be preferable to increase as much as possible the size of the connector (Fig. 2), this is not always possible because of the damage that would be created on the periodontium, because of it is impossible to implement adequate oral hygiene maneuvers at the prostheses, if it has a connector too large in dimension (Fig. 3).
Figure 3.
Detail of the structure of zirconia in a full arch: the connectors after finishing. This is needed to ensure spaces for adequate oral hygiene of the prosthesis, to protect the periodontium and / or the peri-implant tissue.
From all these studies is clear how the connector is the critical factor of the whole restoration and that it should be not less than 6.25 mm2 or more. This is valid for 3-unit posterior bridges. In the case of bridges of 4 elements it must surely be greater than 7 mm2 (9 mm2, or better 16 mm2). This is valid in the case of normal chewing activities while in the case of parafunctions is more appropriate to use the classic metal-ceramic rehabilitation.
The last point is that regarding the long-term behavior of zirconia fixed partial dentures.
The studies in the literature are not numerous and have a mean follow-up of 3 years. For metal-ceramic that time period increased to 8 years. In addition, the maximum follow-up is 5 years, while for metal-ceramic are reaching follow-up studies of up to 20 years. For many authors, the follow-up considered for the zirconia is not enough to establish with certainty the absolute reliability of the material in the long term. Despite all this, it is interesting to note that the behavior of the material, although in the short term, seems to be promising.
The survival rates are very high although slightly lower than the traditional metal-ceramic.
In fact, for the traditional metal-ceramic prostheses the 5-year survival rate is about of 95.6% while for zirconia it comes to 93.3% (23).Another study has even obtained a 5-year survival rate of 97.8% (26). From all this it is possible to deduce how the zirconia FPDs represent a long-term behavior very encouraging.
The failures are mainly related to technical problems and in most cases due to fracture of the veneering ceramic (Fig. 4). In particular the proportion of fracture of the veneering ceramic is between 6 and 15% in a period ranging from 3 to 5 years from the placement of the restoration but may even reach 50%, while for metal-ceramic restorations this rate is between 4 and 10% after 10 years (22,24). The origin of this complication is unknown but has been advanced the hypothesis that it depends on a failure of the link between the zirconia core and veneering ceramic.
Figure 4.
Same detail of full arch after veneering. In the literature, possible fractures of ceramic veneering, detected after follow up, are almost always due to poor design of the connectors, in terms of size of the diameter and shape.
This failure is due to a number of factors affecting core-veneer interface: stresses due to differences in thermal expansion coefficient between the two materials, lack of humidity in the core due to the ceramic veneering, ceramic cooking process, phase transformation of zirconia at core-veneer interface due to thermal or mechanical stress influences, the formation of defects during the different procedures (24,25). Another important cause of fracture of ceramics is the lack of uniform support of the veneering ceramic due to the shape of the zirconia core. The shape of the core depends on the depth of cut, abutment height, interdental space and the length of the dental lacuna (24,25,26). In particular, the connector shape plays an important role in this. Other causes of failure, but certainly less frequent than the former are represented by biological complications: secondary caries (11%), fracture of the abutment tooth (38%), loss of retention (13%) and periodontal disease (27%).
Despite all of this in some studies in the literature it is stated that the expectation on the survival of posterior zirconia fixed partial dentures is estimated to be over 20 years (14). Moreover, in agreement with the available data, the zirconia FPDs can be compared to those in metal-ceramic and therefore able to withstand the masticatory loads of the posterior areas of the oral cavity (23).
Conclusions
At the conclusion of this work may be said that the zirconia is an innovative material in the landscape of modern dentistry. It combines excellent aesthetic characteristics with many exceptional mechanical properties that make it suitable for production of restorations in the posterior areas of the oral cavity.
Its applications are many and range through the orthodontics, implantology and endodontics. But it is certainly the prosthetic field that draws most benefit from this material. With the zirconia is, in fact, possible to realize single crowns and bridge restorations up to five elements also in the posterior oral cavity. The data in the literature comfort us in this direction, indicating exceptional strength values when compared to other commercially available ceramic materials and the same metal-ceramic. An important factor that can strongly influence the longevity of the restoration is the size of the connector, whose size, if inappropriate, can lead to rapid failure of the restoration.
Even the long-term studies, although few, indicate that zirconia is a reliable material for the production of prostheses in the posterior areas of the oral cavity with 5-year success rate up to 97.8%. Even these values are comparable to those obtained with the traditional metal-ceramic. However, further studies are needed with longer follow-up to remove any doubt about the actual reliability of the material. With this background, the zirconia is certainly a very promising material and it is intended to get more and more acceptance on the part of modern dentistry.
References
- 1.Kelly JR, Nishimura I, Campbell SD. Ceramics in dentistry: historical roots and current perspectives. J Prosthet Dent. 1996 Jan;75(1):18–32. doi: 10.1016/s0022-3913(96)90413-8. [DOI] [PubMed] [Google Scholar]
- 2.Mc Lean JW, Hughes TH. The reinforcement of dental porcelain with ceramic oxides. Brit. Dent. J. 1965;119:251–267. [PubMed] [Google Scholar]
- 3.Denry I, Robert Kelly J. State of the art of zirconia for dental applications. Dental Materials. 2008;24:299–307. doi: 10.1016/j.dental.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Att W, Stamouli K, Gerds T, Strub RJ. Fracture resistance of different zirconium dioxide three-unit all-ceramic fixed partial venture. Acta Odontologica Scandinavica. 2007;65:14–21. doi: 10.1080/00016350600856232. [DOI] [PubMed] [Google Scholar]
- 5.Rosentritt M, Behr M, Lang R. Fracture strength of tooth colored posterior fixed partial venture. J. Dent. Res. 2001;80:57. (abstract 174). [Google Scholar]
- 6.Rountree P, Nothdurft F, Pospiech P. In-vitro investigations on the fracture strength of all-ceramic posterior bridge of ZrO2- ceramics. J. Dent. Res. 2001;80:57. (abstract 173) [Google Scholar]
- 7.Suttor D, Bunke K, Hoescheler S, Hauptmann H, Hertling G. LAVA – the system for all-ceramic ZrO2 crown and bridge frameworks. Int J Comput Dent. 2001 Jul;4(3):195–206. [PubMed] [Google Scholar]
- 8.Tinschert J, Natt G, Mautsch W, Augthun M, Spiekermann H. Fracture resistance of lithium- disilicate-, alumina-, and zirconia- based three-unit fixed partial dentures: a laboratori study. Int J Prosthodont. 2001;14:231–238. [PubMed] [Google Scholar]
- 9.Luthy H, Filser F. Strenght and reliability of four-unit all-ceramic posterior bridge. Dental Materials. 2005;21:930–937. doi: 10.1016/j.dental.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 10.Stiesh-Scholz M, Borchers L, Herzg TJ, Kohorst P. Load-bering capacity of all-ceramic posterior four-unit fixed partial dentures with different zirconia frameworks. Eur J Oral Sci. 2007;115(2):161–166. doi: 10.1111/j.1600-0722.2007.00429.x. [DOI] [PubMed] [Google Scholar]
- 11.Dornhofer R, Arnetlz GV, Koller M. Comparison of the static loading capacity of all-ceramic bridge frameworks in posterior teeth using three hard core materials. Int J Comp Dent. 2007;10:1–14. [PubMed] [Google Scholar]
- 12.Filser F, Kocher K, Weibel F, Luthy H, Scharer P, Gauckler LJ. Reliability and strength of all-ceramic dental restorations fabricated by direct ceramic machining (DCM) Int J Comput Dent. 2001;4:89–106. [PubMed] [Google Scholar]
- 13.Oh WS, Anusavice KJ. Effect of connector design on the fracture resistance of all-ceramic fixed partial dentures. J Prosthet Dent. 2002;87:536–542. doi: 10.1067/mpr.2002.123850. [DOI] [PubMed] [Google Scholar]
- 14.Studart AR, Filser F, Kocher P, Gauckler LJ. In vitro lifetime of dental ceramics under cyclic loading in water. Biomaterials. 2007;28:2695–2705. doi: 10.1016/j.biomaterials.2006.12.033. [DOI] [PubMed] [Google Scholar]
- 15.Larsson C, Holm L, Lovgren N, Kokubo Y. Fracture strength of four-unit Y-TZP FPD cores designed with varying connector diameter. An in-vitro study. J. Of Oral Rehabilitation. 2007;34:702–709. doi: 10.1111/j.1365-2842.2007.01770.x. [DOI] [PubMed] [Google Scholar]
- 16.Sturzenegger B, Feher A, Luthy H, Schumacher M, Loeffel O, Filser F, et al. Clinical study of zirconium oxide bridges in the posterior segments fabricated with the DCM system. Schweiz Monatsschr Zahnmed. 2000;110:131–139. [PubMed] [Google Scholar]
- 17.Pospiech PR, Rountree PR, Nothdurft FP. Clinical evaluation of zirconia-based all ceramic posterior bridges: two year results. J Dent Res. 2003;(Special Issue B):82. 114. IADR Abstract No. 817. [Google Scholar]
- 18.Bornemann G, Rinke S, Huels A. Prospective clinical trial with conventionally luted zirconia-based fixed partial denture – 18-months results. J Dent Res. 2003;82(Special Issue B):117. IADR Abstract No. 842. [Google Scholar]
- 19.Suarez MJ, Lozano JF, Paz Salido M, Martinez F. Three-year clinical evaluation of In-Ceram Zirconia posterior FPDs. International Journal of Prosthodontic. 2004;17:35–8. [PubMed] [Google Scholar]
- 20.Vult von Steyern P, Carlson P, Nilner K. All-ceramic fixed partial denture designed according to the DC-Zirkon tecnique. A 2-year clinical study. J Oral Rehabil. 2005;32:180–187. doi: 10.1111/j.1365-2842.2004.01437.x. [DOI] [PubMed] [Google Scholar]
- 21.Sailer I, Feher A, Filser F, Luthy H, Gauckler LJ, Scharer P, et al. Prospective clinical study of zirconia posterior fixed partial dentures: 3-year follow-up. Quintessence International. 2006;37:685–93. [PubMed] [Google Scholar]
- 22.Raigrodski AJ, Chiche GJ, Potiket N, et al. The efficacy of posterior three-unit zirconium-oxide-based ceramic fixed dental prostheses: a prospective clinical pilot study. J. Prosth. Dentistry. 2006 Oct;96:237–244. doi: 10.1016/j.prosdent.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Sailer I, Feher A, Filser F, Gauckler LJ, Luthy H, Hammerle CH. Five year clinical results of zirconia frameworks for posterior fixed partial denture. Int J Prosthodont. 2007;20:383–388. [PubMed] [Google Scholar]
- 24.Edelhoff D, Beuer F, Weber V, Johnen C. HIP zirconia fixed partial denture. Clinical results after 3 years of clinical service. Quintessence Int. 2008;39:459–471. [PubMed] [Google Scholar]
- 25.Tinschert J, Schulze KA, Natt G, Latzke P, Heussen N, Spiekermann H. Clinical behavior of zirconia-based fixed partial venture made of DC-Zirkon: 3-year results. Int J Prosthodont. 2008;21:217–222. [PubMed] [Google Scholar]
- 26.Molin MK, Karlsson SL. Five-year clinical prospective evaluation of zirconia-based Denzir 3-unit FPDs. Int J Prosthodont. 2008;21:223–227. [PubMed] [Google Scholar]
- 27.Roediger M, Rinke S, Huels A. Prospective clinical evaluation of Cercon TM premolar and molar FPDs. J Dent Res. 2009;88(Special Issue B) IADR Abstract No. 2347. [Google Scholar]