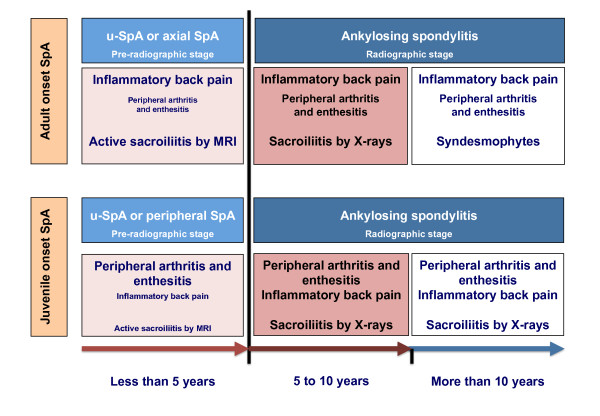
Figure 1.
The modified schematic representation of Rudwaleit’s scheme[49]on the transition of undifferentiated juvenile-onset spondyloarthritis (u-SpA) to ankylosing spondylitis (AS) in the context of axial and peripheral SpA. Note: In this model, we present the idea that axial SpA is mostly representative of adult-onset patients (upper panel) whereas the subset that could mostly be adapted to children and adolescents with juvenile-onset SpA is that of peripheral SpA (lower panel). Time to transition is an estimation based on scarce published reports. Note that during the interval between disease onset and the 5th year of symptoms, the most frequent and characteristic symptoms and signs in juvenile-onset SpA are peripheral arthritis and enthesitis and not inflammatory back pain (small fonts; IBP). In contrast, IBP, and not peripheral symptoms, (small fonts) is the most important characteristic in adult patients. Beyond the 5th year of disease, the proportion of patients with both juvenile and adult onset SpA fulfilling the modified New York criteria for AS [3] increases to reach a maximum around 10 years after onset. Imaging of the sacroiliac joints, particularly the early inflammatory stage by magnetic resonance imaging (MRI) is essential in the study of adult patients with IBP. This approach does not seem the logical in the study of juvenile-onset SpA since IBP occurs in less than 15% in the initial years of disease. While the demonstration of edema in the sacroiliac joints by MRI has therapeutic implications in adult-onset SpA –the earliest the treatment, the better the response, the indications for early treatment of children and adolescents with SpA with tumor necrosis factor (TNF) blockers could mostly rely on peripheral symptoms. Regarding the ostechondral proliferative stage of spinal involvement, it is only probable that in juvenile-onset patient this stage takes a long time to develop, perhaps similar to that seen in adults.