Abstract
Subtypes of intestinal metaplasia may have different manifestations in the carcinogenesis of gastric mucosa. The present study aimed to investigate expression of murine double minute gene 2 (mdm2) in atypical intestinal metaplasia (AIM) and its relationship to gastric carcinoma. Intestinal metaplasia (IM) specimens were obtained from 58 cases. Using a novel classification of IM, the specimens were classified according to morphological changes exhibited in the gastric mucosa; specifically, atypical intestinal metaplasia (AIM) and simple intestinal metaplasia (SIM). The gatric carcinoma specimens were then compared with types I, II and III IM based on different substances present in the mucous. Envision immunohistochemical technique was applied to the detection of the expression of p53 and mdm2 in 58 IM and 30 gastric carcinoma cases. Expression of both p53 and mdm2 proteins was found to be higher in gastric carcinomas (p53, 56.67%, 17/30 and mdm2, 53.33%, 16/30) and AIM (p53, 51.85%, 14/27 and mdm2, 51.85%, 14/27) as compared to SIM (p53, 25.81%, 8/31 and mdm2, 19.35%, 6/31) (P<0.05). A similar pattern of expression of mdm2 protein was found in type I (36.84%, 7/19), type II (38.46%, 10/26) and type III (23.08%, 3/13) IM and gastric carcinoma (53.33%, 16/30). p53 expression was higher in gastric carcinoma (56.67%) compared to type I IM (26.32%) (P<0.05). However, no differences were evident among type II (42.31%, 11/26), type III (46.15%, 6/13) IM and gastric carcinoma. AIM may reveal the precancerous nature of gastric carcinoma more clearly than SIM or the conventional IM subtypes. Additionally, AIM may be involved as a preneoplastic lesion and therefore be an effective indicator in the clinical follow-up of gastric carcinoma patients.
Keywords: atypical intestinal metaplasia, simple intestinal metaplasia, murine double minute gene 2
Introduction
Gastric carcinoma is the fourth most prevalent malignancy worldwide (1) and is one of the most common causes of cancer-related mortality in China (2). The only effective way of improving the survival rate of patients suffering from gastric carcinoma is an early diagnosis. More than half of patients presenting with gastric carcinoma diagnosed from a biopsy were in an advanced stage of cancer progression. Thus, a more critical understanding of preneoplastic lesions in the gastric mucosa may prove helpful in the detection of early-stage carcinoma in a clinical setting. The development of gastric carcinoma is closely associated with the presence of atrophic gastritis as well as intestinal metaplasia (IM). Furthermore, it has been shown that the presence of IM significantly increases the risk of gastric carcinoma (3). However, not all individuals with intestinal metaplasia progress to gastric cancer. Therefore, the issue as to which IM patients should be clinically followed has yet to be resolved (4).
Three types (I–III) of IM have been described according to morphology and mucin histochemistry (5,6). Findings of a number of studies revealed that type III was closely involved in intestinal gastric carcinoma (7–10), whereas investigations that have been conducted conclude that sulphomucin-positive IM does not identify a high-risk group and is of no value in the surveillance of gastric cancer (11). Additionally, Petersson et al suggest that type III IM is a less sensitive indicator of future development of gastric carcinoma than previously anticipated (12).
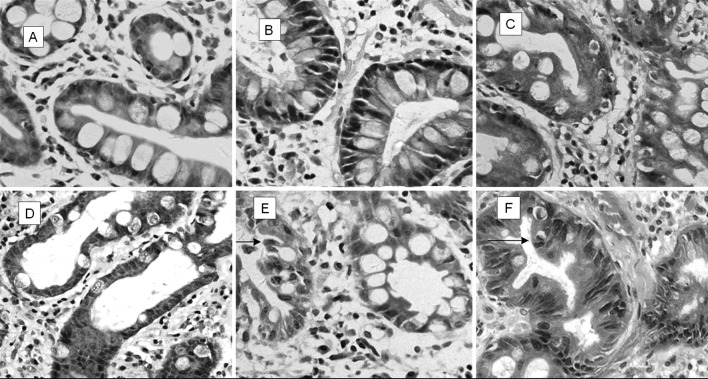
As in our previous study, in this study IM was divided into two subtypes according to morphology of the metaplastic epithelium: simple intestinal metaplasia (SIM), in which no or minimal polymorphism was found and atypical intestinal metaplasia (AIM), in which metaplastic cells presented significantly more polymorphisms or atypical changes (13). The predominant feature of AIM is the appearance of immature goblet cells scattered in the epithelium of IM already present in the gastric mucosa. These cells exhibit an enlarged cell nucleus with several mucin vacuoles in the cytoplasm and the nucleus loses its polarity. As with the immature goblet cells, changes are also observed in some columnar cells. In contrast, no or minimal nuclear pleomorphism and polarity change of goblet and columnar cells in SIM has been observed. The key to distinguishing the two groups of IM is the identification of the immature goblet cells since there was little difficulty in comparing the columnar cell atypical changes in the two groups. The growth pattern in AIM was more focal and showed fewer Paneth cells than those in SIM; partially serrated growth with predominant nucleoli was observed in AIM.
Different subtypes of IM in relation to tumor suppressor gene p53 (expressed in AIM) were investigated in the present study and compared with the expression of its downstream target gene murine double minute gene 2 (mdm2). Under normal physiological conditions, the wild-type p53 protein suppresses cell proliferation, stops cell division at the G1 checkpoint, and promotes the repair of damaged DNA. p53 protein also initiates apoptosis in case of failed DNA repair. In the absence of normally functioning wild-type p53 protein, cells are sensitive to the S-phase entry with injured DNA and the genetic changes, resulting in cell malignant change and tumor formation. As a negative regulator of p53, mdm2 interacts with p53 protein to inhibit the transcriptional activation of p53, leading to cell proliferation in a tumor. The interaction between p53 and mdm2 plays a crucial role in cell cycle arrest, as well as apoptosis following DNA damage (14,15). The wild-type p53 gene induces the expression of mdm2 protein, which, in turn, strictly regulates the p53 protein level. By depriving p53 of antineoplastic activity, a high expression of mdm2 can obstruct the p53-mediated transactivation (16). This p53-mdm2 feedback loop is vital for cell-cycle regulation, and the elimination of p53-dependent checkpoints is associated with carcinogenesis (17,18).
SIM and AIM classification may better indicate the essential nature of IM. SIM, due to its hyperplastic nature induced in gastritis, was devoid of cellular pleomorphism as well as molecular diversity. On the other hand, AIM possessed atypia initiated by an oncogene during carcinogenesis. This classification was performed to determine which type of IM is more relevant to gastric carcinoma.
Materials and methods
Subjects
Informed consent was obtained from each patient and the study was approved by the institutional ethics committee of the Shandong University School of Medicine. We obtained 58 samples of IM from endoscopic biopsy and 30 gastric carcinoma specimens by surgical resection at Qilu Hospital of Shandong University. Of 88 patients studied, 59 were males and 29 females, with ages ranging from 30 to 80 years of age (median 54.56). Additionally, in the 58 cases of IM, 38 patients were male and 20 female, with an age range of 30–76 years (median 55.88), while in the 30 gastric carcinoma cases, 21 patients were male and 9 female, with an age range of 30–80 years (median 52.00).
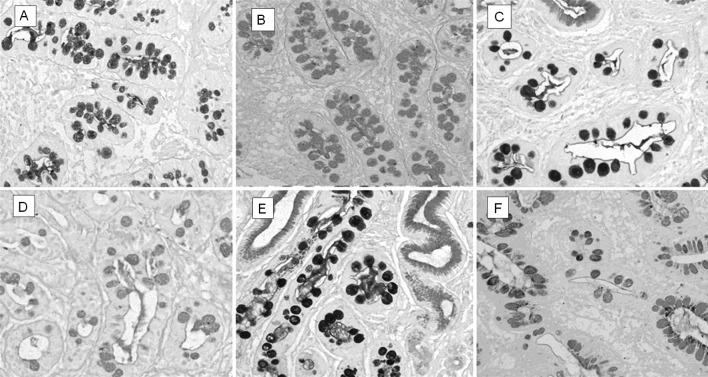
Mucin histochemical staining for IM subtypes was performed. Serial sections were cut and stained with hematoxylin and eosin. To determine mucin expression patterns, alcian blue pH 2.5/periodic acid-Schiff and high-iron-diamine (AB pH 2.5/PAS, AB pH 2.5/HID) were performed to identify IM subtypes (19). A total of 58 cases of IM were classified in accordance with the system used by Jass and Filipe (6,20): type I (complete) IM goblet cells secrete predominantly acid sialomucins; type II (incomplete) IM goblet cells secrete predominantly sialomucins; columnar mucous cells secrete non-sulfated mucins; type III (incomplete) IM resembles type II except that columnar mucous cells predominantly secrete sulfomucins (Fig. 1).
Figure 1.
Three types of intestinal metaplasia (IM) according to immunohistochemical stains. (A) Type I IM: AB-PAS AB-positive, PAS-negative. (B) Type I IM: HID-AB AB-positive, HID-negative. (C) Type II IM: AB-PAS AB-positive, PAS-positive. (D) Type II IM: HID-AB AB-positive, HID-negative. (E) Type III IM: AB-PAS AB-positive (blue), PAS-positive. (F) Type III IM: HID-AB AB-positive (blue), HID-positive (grey and black) (magnification, ×200).
IM subtyping according to morphology and structural changes
A total of 58 IM cases were classified as AIM and SIM according to the morphology with or without structural and cellular changes of pleomorphism in the metaplastic epithelium.
Immunohistochemical staining
Immunohistochemical staining was performed using the Envision method. Expression analyses of p53 and mdm2 proteins were performed on formalin-fixed, paraffin-embedded specimens. p53 monoclonal antibody (ZM-0408) and mdm2 (ZM-0425) as well as PV-9000 2-step plus poly-HRP anti-mouse/rabbit IgG detection system were purchased from ZSGB-Bio (Beijing, China).
Briefly, 4 μm sections were cut and dewaxed in xylene and then rehydrated through graded alcohol. For the antigen retrieval regimen, all slides were microwaved in 10 mmol/l sodium citrate buffer (pH 6.0) at 10-min intervals for a total of 20 min. The endogenous peroxidase activity was blocked by 10 min of incubation with 3% hydrogen peroxidase (reagent A) at room temperature. After washing in phosphate-buffered saline (PBS), the sections were incubated with monoclonal mouse anti-human antibodies p53 (ZM-0408) and mdm2 (ZM-0425) overnight at 4°C. The sections were washed with PBS and incubated with polymerase auxiliary (reagent B) for 20 min. After washing in PBS, the sections were incubated with biotinylated HRP-conjugated secondary antibody (reagent C) for 30 min at room temperature and 3,3′-diamino- benzidine was visualized. Tissues were counterstained with hematoxylin. A negative control used PBS instead of the primary antibodies.
Immunohistochemical analysis
Positive nuclear staining of p53 and mdm2 proteins appeared as brown granules. The percentage of positively stained cells was estimated in an average of 100 cells counted in more than 5 high-magnification fields (high-power field, ×400). A positive result was defined as ≥10% of the cells exhibiting positive staining.
Statistical analysis
The significance of association was determined using the analysis of variance (ANOVA) or χ2 test. P<0.05 was considered to be statistically significant.
Results
Subtype distribution of 58 IM samples
Since IM was multifocally present, 19 (32.75%) cases with foci of type I IM, 26 (44.82%) cases of type II IM, and 13 (22.41%) cases of type III IM were identified. In 31 (53.44%) SIM samples, there were 9 type I, 15 type II and 7 type III IM samples. In 27 (46.55%) AIM samples, there were 10 type I, 11 type II and 6 type III IM samples (Table I).
Table I.
The distribution of 58 IM cases with different subtypes of intestinal metaplasia.
| Type I | Type II | Type III | Total (%) | |
|---|---|---|---|---|
| SIM | 9 | 15 | 7 | 31 (53.45) |
| AIM | 10 | 11 | 6 | 27 (46.55) |
| Total (%) | 19 (32.76) | 26 (44.83) | 13 (22.41) | 58 (100.00) |
IM, intestinal metaplasia; SIM, simple intestinal metaplasia; AIM, atypical intestinal metaplasia.
Expression of p53 protein
A positive expression of p53 was observed in 25.81% (8/31) of SIM, 51.85% (14/27) of AIM and 56.67% (17/30) of gastric carcinomas. Expression of p53 in gastric carcinomas and AIM was higher than that in SIM (P<0.05) while no significant difference was observed between AIM and gastric carcinomas (P>0.05).
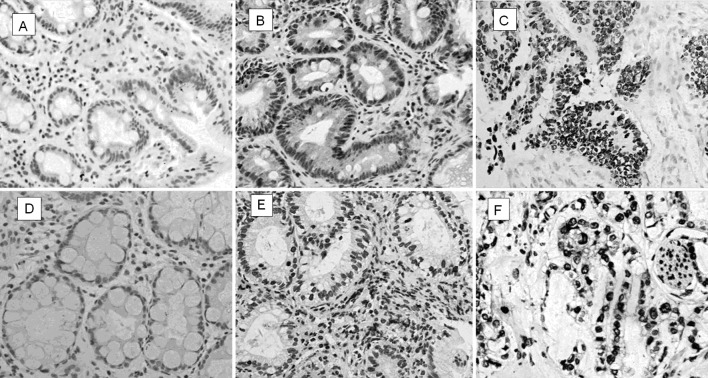
p53 observed in the conventional IM was expressed in 26.32% (5/19) of type I, 42.31% (11/26) of type II and 46.15% (6/13) of type III IM. A reduced expression of p53 was only found in type I IM (P<0.05) while no difference was observed between gastric carcinomas and types II or III IM (P>0.05) (Table II; Fig. 2).
Table II.
Expression of p53 and mdm2 proteins in different subtypes of IM and gastric carcinoma.
| Total (n) | p53 | mdm2 | |||
|---|---|---|---|---|---|
|
|
|
||||
| Positive (%) | Negative | Positive (%) | Negative | ||
| SIM | 31 | 8a (25.80) | 23 | 6a (19.35) | 25 |
| AIM | 27 | 14 (51.85) | 13 | 14 (51.85) | 13 |
| Type I | 19 | 5b (26.31) | 14 | 7 (36.84) | 12 |
| Type II | 26 | 11 (42.30) | 15 | 10 (38.46) | 16 |
| Type III | 13 | 6 (46.15) | 7 | 3 (23.07) | 10 |
| Gastric carcinoma | 30 | 17 (56.66) | 13 | 16 (53.33) | 14 |
P<0.05 simple inestinal metaplasia (SIM) vs. gastric carcinoma.
P<0.05 type I vs. gastric carcinoma.
AIM, atypical intestinal metaplasia.
Figure 2.
Expression of p53 and mdm2 proteins in simple intestinal metaplasia (SIM), atypical intestinal metaplasia (AIM) and gastric carcinoma. (A) p53-negative in SIM. (B) p53-positive in AIM (nuclei). (C) p53 expression increased in gastric carcinoma (nuclei). (D) mdm2-negative in SIM. (E) mdm2-positive in AIM (nuclei). (F) mdm2 expression increased in gastric carcinoma (nuclei) (Envision method, magnification, ×200).
Expression of mdm2 protein
Positive expression rates of mdm2 were observed in SIM 19.35% (6/31), AIM 51.85%, (14/27) and gastric carcinomas 53.33% (16/30), respectively. The expression of mdm2 in gastric carcinomas and AIM was significantly higher than that in SIM (P<0.05), while no significant difference was found between AIM and gastric carcinomas (P>0.05) (Table II, Fig. 2).
The positive expression rates of mdm2 in types I, II and III of IM were 36.84% (7/19), 38.46% (10/26) and 23.07% (3/13), respectively. No statistical significance was found in the expression of mdm2 among the gastric carcinomas and the three types (I, II and III) of IM (P>0.05).
Discussion
Intestinal metaplasia (IM) occurs in benign lesions as well as in carcinoma of the gastric mucosa, but only a small proportion of cases are disposed towards or develop into carcinoma. The relationship between IM and gastric carcinoma has yet to be elucidated, as has the issue of which type of IM is closely related to gastric carcinoma. In this study, IM in the gastric mucosa was classified into two groups: SIM (simple intestinal metaplasia, IM with minimal or no pleomorphism), and AIM (atypical intestinal metaplasia, IM with atypical changes) (13). Various differences between the two groups were observed (Table III, Fig. 3).
Table III.
The differences in morphology between SIM and AIM.
| SIM | AIM | |
|---|---|---|
| Tissue organization | Glands arranged neatly with uniform goblet cells | Glands arranged irregularly, enlarged round nuclei with polarity changes |
| Goblet cells | Minimal changes resemblance to normal intestine | Immature differentiation, polarity changes and rare mitosis |
| Column cells | Minimal changes resemblance to normal intestine | Enlarged nuclei with foamy cytoplasm. |
| Gastric pit | The mucosa is flat | Ruffled mucosa with deeper pit, appeared to serrated change |
SIM, simple intestinal metaplasia; AIM, atypical intestinal metaplasia.
Figure 3.
Morphological differences in SIM and AIM. (A) SIM, uniform goblet cells. (B) SIM, glands arranged neatly. (C) AIM, irregular goblet cells. (D) AIM, changed polarity of goblet cells. (E) AIM, reversed polarity of goblet cell (arrow). (F) AIM, mitosis (arrow) and gastric pit appeared to serrated change (hematoxylin and eosin; magnification, ×400).
There are three substantial advantages to this novel classification of IM into AIM and SIM as compared to conventional classification. Firstly, the novel classification is easy and practical for the pathologist to diagnose under microscope without supplementary staining. Secondly, the cellular morphologic variants of IM usually coordinate with molecular changes as well as progression, since classification of AIM as such clarifies its precancerous nature. Thirdly, the classification is not only a diagnostic method, but also a theory that may promote the understanding of IM along with clinically pragmatic activities in the follow-up of IM patients such as ‘optical biopsy’ of gastric mucosa, for which IM was diagnosed under confocal endoscopy without histopathological biopsy (21,22). As for the conventional classification of IM, our data show that both AIM and SIM distributed in all three types, whereas intrinsic precancerous information was obscured by the conventional classification of IM based on mucous chemical staining.
p53, a tumor suppressor gene, plays an important role in the regulation of gene expression in cell cycle progression and apoptosis in response to DNA damage (23). Mutation in the p53 gene is one of the most prevalent genetic abnormalities in human cancer (24), including gastric carcinoma. A number of studies suggest that gastric precancerous lesions exhibit p53 abnormalities, particularly in the early stages of intestinal metaplasia (25–27). In this study, the expression of p53 was significantly higher in gastric carcinoma than that in type I, but not in types II or III IM. The positive expression rates of p53 in SIM, AIM and gastric carcinomas were 25.81, 51.85 and 56.67%, respectively, and the expression of p53 in gastric carcinomas was significantly higher in AIM as compared to SIM. Results of various studies also showed that the frequency of p53 mutations is consistent at around 40% in early and advanced differentiated gastric carcinomas as well as advanced undifferentiated carcinomas (28,29), whereas it is low in early undifferentiated carcinomas (30,31). The finding that p53 mutations were detected in IM and gastric cancer (32) suggests that IM is a precursor of differentiated carcinomas. Therefore, our data confirm the hypothesis that p53 gene mutation is an early event in the development of gastric carcinoma.
mdm2, a newly discovered oncogene, is located at chromosome 12q13–14; the gene’s organization on the human chromosome was evaluated in 1992 (33). Due to its association with the tumor suppressor p53 gene and its implication in human cancer, the biochemical activities of mdm2 in cancer cells have been investigated thoroughly. A high expression of the mdm2 protein has been found in 36% of all types of sarcomas and 10% of well-differentiated gliomas, as well as esophageal cancer, neuroblastoma, and anaplastic astrocytoma (34), suggesting that mdm2 expression is one of the common causes of oncogenesis (35). In our study, the expression of mdm2 in gastric carcinomas was not significantly higher than that in types I, II and III of IM, while it was significantly higher in AIM as compared to SIM (the positive expression rates of mdm2 in SIM, AIM and gastric carcinomas were 19.35, 51.85 and 53.33%, respectively). Findings of previous studies have suggested that the expression of mdm2 increases in gastric carcinoma (36,37). Nakajima et al (3) reported that expression of the mdm2 protein increased not only in gastric cancer, but also in intestinal metaplasia as compared to chronic gastritis. A distinct mdm2 expression was observed in our study, indicating the precancerous nature of AIM more accurately than mucous classification. Further investigation into the level of p53 and mdm2 expression through RT-PCR is required. However, the main objective of this study was to observe p53 and mdm2 expression through routine immunohistochemical studies as these methods are readily available in the clinical environment.
Since the expression of p53 and mdm2 proteins was found to be significantly higher in AIM and gastric carcinomas as compared to SIM, our findings revealed that AIM had more atypia at the molecular level than that of SIM, together with more morphological disturbances. Additionally, compared to SIM, AIM has greater potential to progress to a severe precancerous lesion or gastric cancer. Findings of the present study therefore suggest that SIM is a response to stimuli such as inflammation, whereas AIM may undergo malignant transformation and be considered a preneoplastic lesion (13). This is an effective criterion by which to diagnose early gastric carcinomas in the clinical follow-up of AIM patients. However, the exact pathogenesis or pathways of AIM in the multi-step carcinogenesis of the gastric mucosa has yet to be elucidated. Effective analysis of diagnostic samples is required to draw a definitive conclusion. Therefore, further studies with a larger patient population and a thorough retrospective follow-up using a rigorous research design are required.
Acknowledgements
This study was funded by a program from Shandong Province Science and Technology Committee Dept. of Health (2006TK47).
References
- 1.Burkitt MD, Varro A, Pritchard DM. Importance of gastrin in the pathogenesis and treatment of gastric tumors. World J Gastroenterol. 2009;15:1–16. doi: 10.3748/wjg.15.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen XM, Chen GY, Wang ZR, Zhu FS, Wang XL, Zhang X. Detection of micrometastasis of gastric carcinoma in peripheral blood circulation. World J Gastroenterol. 2004;10:804–808. doi: 10.3748/wjg.v10.i6.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakajima N, Ito Y, Yokoyama K, Uno A, Kinukawa N, Nemoto N, Moriyama M. The expression of murine double minute 2 (MDM2) on helicobacter pylori-infected intestinal metaplasia and gastric cancer. J Clin Biochem Nutr. 2009;44:196–202. doi: 10.3164/jcbn.08-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leung WK, Sung JJ. Review article: intestinal metaplasia and gastric carcinogenesis. Aliment Pharmacol Ther. 2002;16:1209–1216. doi: 10.1046/j.1365-2036.2002.01300.x. [DOI] [PubMed] [Google Scholar]
- 5.Jass JR. Role of intestinal metaplasia in the histogenesis of gastric carcinoma. J Clin Pathol. 1980;33:801–881. doi: 10.1136/jcp.33.9.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jass JR, Filipe MI. A variant intestinal metaplasia associated with gastric carcinoma: a histochemical study. Histopathology. 1979;3:191–199. doi: 10.1111/j.1365-2559.1979.tb02996.x. [DOI] [PubMed] [Google Scholar]
- 7.Dixon MF. Campylobacter and chronic gastritis. In: Rathbone BJ, Heatley RV, editors. Campylobacter and Gastroduodenal Disease. Blackwell Scientific Publications; Oxford: 1989. pp. 1061–1116. [Google Scholar]
- 8.Sipponen P, Hyvainen H. Role of helicobacter pylori in the pathogenesis of gastric peptic ulcer and gastric cancer. Scand J Gastroenterol Suppl. 1993;196:3–6. doi: 10.3109/00365529309098333. [DOI] [PubMed] [Google Scholar]
- 9.Dixon MF. Pathophysiology of helicobacter pylori infection. Scand J Gastroenterol Suppl. 1994;201:7–10. [PubMed] [Google Scholar]
- 10.Rothery GA, Day DW. Intestinal metaplasia in endoscopic biopsy specimens of gastric mucosa. J Clin Pathol. 1985;38:613–621. doi: 10.1136/jcp.38.6.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ectors N, Dixon MF. The prognostic value of sulphomucin positive intestinal metaplasia in the development of gastric cancer. Histopathology. 1986;10:1271–1277. doi: 10.1111/j.1365-2559.1986.tb02570.x. [DOI] [PubMed] [Google Scholar]
- 12.Petersson F, Borch K, Franzén LE. Prevalence of subtypes of intestinal metaplasia in the general population and in patients with autoimmune chronic atrophic gastritis. Scand J Gastroenterol. 2002;37:262–266. doi: 10.1080/003655202317284156. [DOI] [PubMed] [Google Scholar]
- 13.Zheng Y, Wang L, Zhang JP, Yang JY, Zhao ZM, Zhang XY. Expression of p53, c-erbB-2 and Ki67 in intestinal metaplasia and gastric carcinoma. World J Gastroenterol. 2010;16:339–344. doi: 10.3748/wjg.v16.i3.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barak Y, Juven T, Haffner R, Oren M. mdm2 expression is induced by wild type p53 activity. EMBO J. 1993;12:461–468. doi: 10.1002/j.1460-2075.1993.tb05678.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Momand J, Zambetti GP. Mdm-2: ‘big brother’ of p53. J Cell Biochem. 1997;64:343–352. [PubMed] [Google Scholar]
- 16.Lev Bar-Or R, Maya R, Segel LA, Alon U, Levine AJ, Oren M. Generation of oscillations by the p53-Mdm2 feedback loop: a theoretical and experimental study. Proc Natl Acad Sci USA. 2000;97:11250–11255. doi: 10.1073/pnas.210171597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leach FS, Tokino T, Meltzer P, Burrell M, Oliner JD, Smith S, Hill DE, Sidransky D, Kinzler KW, Vogelstein B. p53 mutation and MDM2 amplification in human soft tissue sarcomas. Cancer Res. 1993;53:2231–2234. [PubMed] [Google Scholar]
- 18.Leite KR, Franco MF, Srougi M, Nesrallah LJ, Nesrallah A, Bevilacqua RG, Darini E, Carvalho CM, Meirelles MI, Santana I, Camara-Lopes LH. Abnormal expression of MDM2 in prostate carcinoma. Mod Pathol. 2001;14:428–436. doi: 10.1038/modpathol.3880330. [DOI] [PubMed] [Google Scholar]
- 19.Reis CA, David L, Nielsen PA, Clausen H, Mirgorodskaya K, Roepstorff P, Sobrinho-Simões M. Immunohistochemical study of MUC5AC expression in human gastric carcinomas using a novel monoclonal antibody. Int J Cancer. 1997;74:112–121. doi: 10.1002/(sici)1097-0215(19970220)74:1<112::aid-ijc19>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 20.Jass JR, Filipe MI. The mucin profile of normal gastric epithelium, intestinal metaplasia and gastric carcinoma. Histochem J. 1981;13:831–939. doi: 10.1007/BF01002633. [DOI] [PubMed] [Google Scholar]
- 21.Hwang JH. To perform a biopsy or not to perform a biopsy? Does confocal endomicroscopy provide the answer for surveillance in Barrett’s esophagus? Gastrointest Endosc. 2009;70:655–657. doi: 10.1016/j.gie.2009.04.047. [DOI] [PubMed] [Google Scholar]
- 22.Liu H, Li YQ, Yu T, Zhao YA, Zhang JP, Zhang JN, Guo YT, Xie XJ, Zhang TG, Desmond PV. Confocal endomicroscopy for in vivo detection of microvascular architecture in normal and malignant lesions of upper gastrointestinal tract. J Gastroenterol Hepatol. 2008;23:56–61. doi: 10.1111/j.1440-1746.2007.05221.x. [DOI] [PubMed] [Google Scholar]
- 23.Vogelstein B, Kinzler KW. p53 function and dysfunction. Cell. 1992;70:523–526. doi: 10.1016/0092-8674(92)90421-8. [DOI] [PubMed] [Google Scholar]
- 24.Harris AL. Mutant p53 - the commonest genetic abnormality in human cancer? J Pathol. 1990;162:5–6. doi: 10.1002/path.1711620103. [DOI] [PubMed] [Google Scholar]
- 25.Correa P, Shiao YH. Phenotypic and genotypic events in gastric carcinogenesis. Cancer Res. 1994;54:1941–1943. [PubMed] [Google Scholar]
- 26.Tahara E, Kuniyasu H, Yasui W, Yokozaki H. Gene alterations in intestinal metaplasia and gastric cancer. Eur J Gastroenterol Hepatol. 1994;6:97–101. [PubMed] [Google Scholar]
- 27.Shiao YH, Ruqqe M, Correa P, Lehmann HP, Scheer WD. p53 alteration in gastric precancerous lesions. Am J Pathol. 1994;144:511–517. [PMC free article] [PubMed] [Google Scholar]
- 28.Uchino S, Noguchi M, Ochiai A, Saito T, Kobayashi M, Hirohashi S. p53 mutation in gastric cancer: a genetic model for carcinogenesis is common to gastric and colorectal cancer. Int J Cancer. 1993;54:759–764. doi: 10.1002/ijc.2910540509. [DOI] [PubMed] [Google Scholar]
- 29.Maesawa C, Tamura G, Suzuki Y, Ogasawara S, Sakata K, Kashiwaba M, Satodate R. The sequential accumulation of genetic alterations characteristic of the colorectal adenoma-carcinoma sequence does not occur between gastric adenoma and adenocarcinoma. J Pathol. 1995;176:249–258. doi: 10.1002/path.1711760307. [DOI] [PubMed] [Google Scholar]
- 30.Tamura G, Sato K, Akiyama S, Tsuchiya T, Endoh Y, Usuba O, Kimura W, Nishizuka S, Motoyama T. Molecular characterization of undifferentiated-type gastric carcinoma. Lab Invest. 2001;81:593–598. doi: 10.1038/labinvest.3780268. [DOI] [PubMed] [Google Scholar]
- 31.Ranzani GN, Luinetti O, Padovan LS, Calistri D, Renault B, Burrel M, Amadori D, Fiocca R, Solcia E. p53 gene mutations and protein nuclear accumulation are early events in intestinal type gastric cancer but late events in diffuse type. Cancer Epidemiol Biomarkers Prev. 1995;4:223–231. [PubMed] [Google Scholar]
- 32.Ochiai A, Yamauchi Y, Hirohashi S. p53 mutations in the non-neoplastic mucosa of the human stomach showing intestinal metaplasia. Int J Cancer. 1996;69:28–33. doi: 10.1002/(SICI)1097-0215(19960220)69:1<28::AID-IJC6>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 33.Oliner JD, Kinzler KW, Meltzer PS, George DL, Vogelstein B. Amplification of a gene encoding a p53-associated protein in human sarcomas. Nature. 1992;358:80–83. doi: 10.1038/358080a0. [DOI] [PubMed] [Google Scholar]
- 34.Bueso-Ramos CE, Manshouri T, Haidar MA, Huh YO, Keating MJ, Albitar M. Multiple patterns of MDM-2 deregulation in human leukemias: implications in leukemogenesis and prognosis. Leuk Lymphoma. 1995;17:13–18. doi: 10.3109/10428199509051698. [DOI] [PubMed] [Google Scholar]
- 35.Iwakuma T, Lozano G. MDM2, an introduction. Mol Cancer Res. 2003;1:993–1000. [PubMed] [Google Scholar]
- 36.Günther T, Schneider-Stock R, Häckel C, Kasper HU, Pross M, Hackelsberger A, Lippert H, Roessner A. Mdm2 gene amplification in gastric cancer correlation with expression of Mdm2 protein and p53 alterations. Mod Pathol. 2000;13:621–626. doi: 10.1038/modpathol.3880107. [DOI] [PubMed] [Google Scholar]
- 37.Tanière P, Martel-Planche G, Maurici D, Lombard-Bohas C, Scoazec JY, Montesano R, Berger F, Hainaut P. Molecular and clinical differences between adenocarcinomas of the esophagus and of the gastric cardia. Am J Pathol. 2001;158:33–40. doi: 10.1016/S0002-9440(10)63941-7. [DOI] [PMC free article] [PubMed] [Google Scholar]